-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(5): 1340-1345
doi:10.5923/j.ajmms.20241405.41
Received: Apr. 23, 2024; Accepted: May 19, 2024; Published: May 21, 2024

Complex Treatment of Chronic Adenoiditis in Children
U. I. Nurov, F. S. Ikramova
Bukhara State Medical Institute, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study examined the results of treatment of three groups of patients with chronic adenoiditis. Analysis of microorganisms revealed differences in the composition of bacteria in each group. The group receiving combined treatment with propolis tincture and photodynamic therapy showed the best results among all three groups. Patients in this group experienced improvement in nasal breathing and hearing, and did not experience recurrence of adenoiditis after surgery. The second group, which received etiological treatment, also showed a decrease in the likelihood of relapses. However, the results require confirmation in larger studies. Overall, this study confirms the potential effectiveness of propolis tincture and photodynamic therapy in the treatment of chronic adenoiditis, opening prospects for further research and application in clinical practice.
Keywords: Propolis tincture, Photodynamic therapy, Chronic adenoiditis
Cite this paper: U. I. Nurov, F. S. Ikramova, Complex Treatment of Chronic Adenoiditis in Children, American Journal of Medicine and Medical Sciences, Vol. 14 No. 5, 2024, pp. 1340-1345. doi: 10.5923/j.ajmms.20241405.41.
Article Outline
1. Introduction
- Chronic inflammation of the lymphoid structures of the nasopharynx is a common problem in medical practice and can lead to relapses and complications in the middle ear [2,7]. The peculiarities of the nasopharyngeal microbiome, anatomical and physiological features of the structure and the immunobiological state of the body play an important role in the development of this pathology [1.5]. Existing methods and remedies for the treatment of chronic inflammation of the adenoids are often ineffective. One of the reasons for this is a decrease in the body's resistance caused by improper use of antibiotics and reduced immune reactivity in children [4]. Respiratory viruses also play a role in the development and recurrence of inflammatory diseases in the nasopharynx. However, the role of respiratory viruses in patients with pharyngeal tonsil pathology has been poorly studied, and diagnostic and prognostic criteria for the complicated course of this pathology have not been determined [3,6]. An analysis of the frequency of complaints from children after adenotomy with complaints of difficulty in nasal breathing and hearing loss shows that surgery does not always prevent recurrence of lymphoid tissue growth and the development of exudative otitis media. This may be due to incomplete removal of lymphoid tissue, anatomical features of the nasopharynx in children, and other factors [8].The aim of the study is to increase the effectiveness of the treatment of chronic adenoiditis by developing a therapeutic and diagnostic algorithm that will include the use of an optimal photodynamic therapy (PDT) scheme in combination with a drug of natural origin "Propolis Tinctures".
2. Materials and Methods
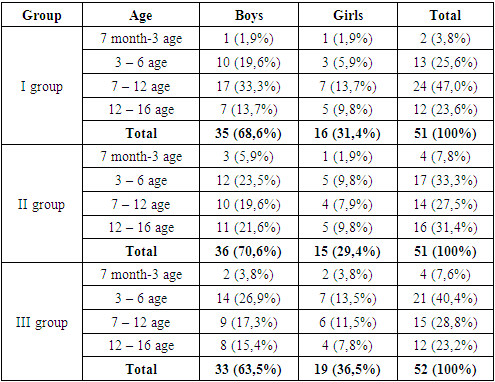
- The study conducted an extensive clinical evaluation of 154 children, whose ages ranged from 7 months to 16 years, and who were diagnosed with adenoiditis. Of these, 67.5% were boys and 32.5% were girls. The average age of the participants was 7.5 years.The main symptoms that led children to go to the clinic were difficulty in nasal breathing (98%), hearing loss (72%) and runny nose (61%). In all children, an increase in the size of the nasopharyngeal tonsil was confirmed on the basis of X-ray and/or endoscopic examinations.Concomitant diseases were also observed in children, including allergic rhinitis (67%), obstructive syndrome (49%), bronchial asthma (23%), chronic tonsillitis (16%) and other diseases of the upper respiratory tract.A clinical examination revealed an increase in the size of the nasopharyngeal tonsil, the presence of pustules, hyperemia and edema of the mucous membrane of the nasopharynx in children. 86% of children also had hearing loss, which can be associated with an increase in the size of the nasopharyngeal tonsil.In our study, we included 154 children (63% boys and 37% girls) aged 7 months to 16 years, according to the established criteria. The participants were divided into three groups:Group I (n=51) consisted of patients with acute adenoiditis who were monitored from September 2022 to April 2023 and received standard conservative treatment. In children of this group, typical clinical characteristics of the disease were identified, depending on the causes of inflammation of the pharyngeal tonsil.Group II (n=51) consisted of patients with exacerbation of adenoiditis who were monitored from October 2022 to May 2023 and received standard conservative treatment, including a drug of natural origin - "tincture propolis".Group III (n=52) consisted of patients with exacerbation of adenoiditis who were monitored from October 2022 to May 2023 and received standard conservative treatment, including a drug of natural origin - "propolis tincture" in combination with photodynamic therapy.Patients of all groups were also distributed according to the decreed age periods used in pediatrics (Table 1).
|
3. The Results and Their Discussion
- The analysis of anamnestic data revealed the following results: maternal smoking during pregnancy was observed with approximately the same frequency in patients of groups 1 and 2 (29.4% and 27.4%), and in group 3 - 21.1%. Patients of the second group were more likely to suffer from acute respiratory viral infections (86.2% versus 72.5% in group 1 and 78.8% in group 3). Family allergoanamnesis associated with allergic diseases was common in patients of the first and third groups (37.2% and 38.5%). The association between adenoiditis and acute respiratory viral infections prevailed in patients of the second and third groups (72.5%, 65.4% vs. 35.3%). ARVI suffered during pregnancy was observed with almost the same frequency (58.8%, 66.6% and 59.6%). The seasonality of patient complaints was also revealed: the largest number of cases is recorded in the autumn-winter period (40.6% - 43.2%), a smaller number in spring (17.5%), and in summer the number of cases is minimal (2%).During pharyngoscopy, all patients revealed a runoff of pathological secretions in the posterior wall of the pharynx. Then, after a general otorhinolaryngological examination, a diagnostic examination of the nasal cavity and nasopharynx was performed using both rigid and flexible optical systems.In all patients, the presence of a pathological secretion on the surface of the pharyngeal tonsil (GM) was found in 100% of cases. Pharyngeal tonsil edema was present with almost the same frequency in the three groups (86.3%, 82.4% and 78.8%, respectively). Grade III hypertrophy of the pharyngeal tonsil also occurred with the same frequency in all three groups (33.3%, 35.3% and 34.7%, respectively). The second degree of pharyngeal amygdala hypertrophy was almost equally common among patients of all groups (51.0%, 47.1% and 48.1%), while pharyngeal amygdala hypertrophy of the first degree was also observed with almost the same frequency in patients of the first group (15.7%), the second group (17.6%) and the third group (17.3%). The pharyngeal mouths of the auditory tubes were visible and free in 66.6% of patients in the second group, 69.2% of patients in the third group, while only 47.1% of patients in the first group.As a result of the analysis of the presented data on the otoscopic picture, it was revealed that pathological signs on otoscopy were more often observed in patients receiving standard conservative treatment. Exudate was found behind the eardrum in 35% of patients from the first group, 37% from the second group and 33% from the third group. Scarring of the eardrum was found only in patients of the first group. It should be noted that complaints of hearing loss were almost equally common in the three groups, amounting to 35.3%, 37.2% and 32.7%, respectively. During the study, we conducted daily monitoring of the concentration of hydrogen ions (pH) of secretions on the surface of the mucous membrane in all patients using the calorimetric method described earlier. The results of this monitoring, including the mean square deviation, median and 25-75 quartiles, were recorded throughout the treatment.Analysis of these results showed that at the beginning of the disease, the concentration of hydrogen ions in the nasal secretions varied both acidic and alkaline. We also found a correlation between the nature of the pathological process in the nasal cavity and changes in pH+ secretion. In the presence of purulent discharge as a result of inflammation of the nasal mucosa, the concentration of hydrogen ions shifted to the acidic side. On the contrary, in the presence of a serous mucosal discharge, the concentration of hydrogen ions was pronounced alkaline, and pH + reached 8.2.For example, the first group of patients with a pronounced alkaline secretion (pH 8-8.2) included 6 people, and as a result, the indicators shifted to a more neutral side. However, from the data obtained, it can be noted that the normalization of the concentration of hydrogen ions occurred already by the 6th day of treatment and amounted to 7.23 ± 0.14. This had a beneficial effect on the functioning of mucociliary transport in the nasal cavity and paranasal sinuses, which is a key protective function of the nose.At the first stage of treatment, group 1 patients received standard conservative therapy, including elimination therapy using seawater and intranasal antiseptic drops (2% protargol). In the presence of effusive otitis media (ESO), children were prescribed vasoconstrictors and electrophoresis with lidase. Efficacy was observed in 25 patients (16.2%), and in 11 cases (21.6%) conservative treatment did not help, and patients were referred for surgical treatment.Of the 51 patients, 11 (21.6%) required nasopharyngeal surgery, including 6 (11.8%) cases of middle ear surgery. The criteria for surgical treatment of children from group I were grade III pharyngeal tonsil hypertrophy with exudative otitis media, grade II pharyngeal tonsil hypertrophy with exudative otitis media and grade III pharyngeal tonsil hypertrophy. Surgical procedures were performed under combined anesthesia and endoscopy control. The effectiveness of surgical treatment was assessed based on complaints and clinical symptoms, research results and catamnesis. After surgery, there was a general improvement in nasal breathing and hearing. In patients undergoing adenotomy, type "A" was observed in the tympanogram. After a year in the catamnesis, all parents reported a decrease in inflammatory diseases of the nasopharynx and middle ear, as well as the restoration of hearing in children. Patients who received only conservative treatment experienced a recurrence of adenoiditis within a year after recovery and in the following 12 months.Taking into account the conducted study of patients of the first group, we analyzed the data and applied them to the treatment of patients of the second group. When prescribing treatment, we took into account the features of adenoiditis of bacterial etiology identified earlier. Antimicrobial agents, including topical antibiotics, and other medications were used in the treatment of patients.Group 1: 40 patients (age 7 months - 16 years) received antibacterial therapy using framycetin sulfate (Isofra) at a dosage of 1 dose endonasally 3 times a day. 8 patients from this group were diagnosed with exudate on the surface of the pharyngeal tonsil.Group 2: 51 patients (age 7 months - 16 years) received the same therapy as group 1, and also used propolis tincture: lubrication of the mucous membranes of the pharynx and tonsils 2-3 times a day (children 8-16 years old) and inhalation with a mixture of propolis tincture and water in a ratio of 1:20, 1-2 times a day (children under 7 years old).Group 3: received the same therapy as group 2, but also underwent photodynamic therapy.All patients were also prescribed drugs for elimination-irrigation therapy, including isotonic solutions of seawater, choosing the form of delivery depending on the patient's age. Decongestants were also prescribed to patients with effusion in the middle ear and endaural electrophoresis with lidase, blowing of the auditory tubes using the Politzer method and pneumatic massage of the eardrums were performed. The course of treatment lasted 7 days.The effectiveness of treatment was assessed by symptoms: difficulty in nasal breathing, discharge on the surface of the pharyngeal tonsil, runoff along the back wall of the pharynx, hyperemia of the mucous membrane of the pharyngeal tonsil, cough. The assessment was carried out before the start of treatment and on the 3rd, 5th and 7th days after the start of treatment using a 4-point scale (0 - no symptoms, 1 - mild symptoms, 2 - moderate symptoms, 3 - severe symptoms).In patients of three groups, there was a decrease in purulent and mucopurulent discharge on the surface of the pharyngeal tonsil and the posterior wall of the pharynx by the third day of treatment. By the end of the course of treatment, all patients in group 3 had no purulent and mucopurulent discharge on the surface of the pharyngeal tonsil. In group 2, the majority of patients (98.1%) also had no discharge on the surface of the pharyngeal tonsil. However, in group 1, 10% of patients retained purulent discharge, and 70% of patients completely lacked all symptoms. In all groups, there is a significant improvement in the condition of the mucous membrane of the pharyngeal tonsil. The hyperemia detected before the start of treatment decreases to 35%, 35.3% and 38%, respectively. By the 7th day of the disease in group 1, 75% of cases completely restore their normal condition, 27.5% of patients have moderate hyperemia, and 2.5% have severe hyperemia. In group 2, 90.2% of cases completely restore the condition of the mucous membrane, 7.8% have moderate hyperemia, and one patient has severe hyperemia. In group 3, the best results were achieved: complete recovery was observed in 96.1% of patients, only two patients had moderate hyperemia of the pharyngeal tonsil mucosa.The results of treatment in the three groups of patients presented in the table show statistically significant differences in the duration of symptoms, which allows for a comparative analysis of the effectiveness of therapeutic effects. Group 3 is characterized by the shortest duration of nasal breathing difficulty (3.2±0.38 days) compared with Group 1 (4.67±1.38 days) and Group 2 (3.5±1.01 days). In addition, Group 3 also demonstrates a shorter duration of discharge (mucous/mucopurulent) on the posterior wall of the pharynx and on the surface of the pharyngeal tonsil (3.3±1.31 days) compared with Group 1 (4.3±1.31 days) and Group 2 (3.7±1.6 days). Endoscopic changes are also more quickly removed in Group 3 (1.9±1.2 days) compared to Group 1 (3.9±1.2 days) and Group 2 (3.1±2.04 days). In addition, the duration of coughing or coughing is also significantly reduced in Group 3 (3.1±1.4 days) compared with Group 1 (5.1±1.4 days) and Group 2 (4.4±1.3 days). These results confirm the effectiveness of the proposed treatment in Group 3 and indicate the high effectiveness of therapeutic effects in this category of patients. However, there were no statistically significant differences between the groups for the parameter "Discharge along the back wall of the pharynx and on the surface of the GM" (p > 0.05).The results of the analysis of the occurrence of bacteria in three groups of patients showed the following. Staphylococcus aureus, Streptococcus pneumoniae and Haemophilus influenzae were the most common in monocultures. Group 1 had a higher incidence of Staphylococcus aureus (3 cases), Haemophilus influenzae (3 cases) and Klebsiella pneumoniae (2 cases). Group 2 was distinguished by the presence of Streptococcus viridans (1 case). In associations of microorganisms (2 pathogens), group 2 was distinguished by the presence of Staphylococcus aureus + Klebsiella pneumoniae (1 case), and group 1 - Staphylococcus aureus + Streptococcus viridans (1 case). Group 3 had only 1 case of Staphylococcus aureus. There were no statistically significant differences in the associations of microorganisms (3 pathogens). The analysis indicates differences in the composition of microorganisms in each group. Thus, the use of propolis tincture in combination with photodynamic therapy in the third group demonstrates the best results among all three groups.
4. Conclusions
- All children who were subject to medical supervision underwent surgical interventions in cases of appropriate indications, including obstructive sleep apnea syndrome (OSA) and grade III adenoid hypertrophy. Surgical treatment was also performed for grade II-III adenoid hypertrophy complicated by exudative otitis media (ESO), and in cases where there was no positive result from conservative treatment of adenoiditis. Patients' complaints included difficulty in nasal breathing, coughing, and hearing loss. An analysis of anamnestic data revealed a link between maternal smoking during pregnancy, the incidence of acute respiratory viral infections, allergic anamnesis and adenoiditis. The seasonality of patient referrals showed the highest number of cases in the autumn-winter period. A pathological secret on the surface of the pharyngeal tonsil was found in all patients. Bacteriological studies have revealed the most common microorganisms: Staphylococcus aureus, Streptococcus pneumoniae and Haemophilus influenzae.Patients in all groups had similar symptoms before starting treatment. On the 5th day of treatment, the majority of patients from all groups (28.9%, 49.5% and 48.4%, respectively) noticed an improvement in nasal breathing difficulties. On day 7, complete recovery of nasal breathing was noted in the third group (100%), while in the first and second groups these indicators were 81% and 87.8%.By the third day of the disease, there was a decrease in purulent discharge on the surface of the pharyngeal tonsil and the posterior wall of the pharynx (20%, 17.7% and 15.4%, respectively). Mucopurulent discharge persisted in 35.1%, 35.4% and 28% of cases, and mucous discharge on the surface of the pharyngeal tonsil was observed in 27.5%, 25.3% and 28% of patients.By the fifth day of treatment in all groups of patients, purulent discharge on the surface of the pharyngeal tonsil decreased to 18.1%, 12.1% and 11.5%, respectively. Mucosal discharge persisted in 20.3% of cases in group 1, in group 2 this indicator decreased to 14.4%, and in group 3 – to 7.7%.At the end of the course of treatment, purulent and mucopurulent discharge on the surface of the pharyngeal tonsil was not observed in group 3 patients. With the exception of 1 case (1.9%), there was no mucosal discharge on the surface of the pharyngeal tonsil in this group. In group 2, 98.1% of patients had no discharge on the surface of the pharyngeal tonsil, with the exception of 1 case (1.9%), where a mucous discharge remained. In group 1, 70% of patients had completely no purulent, mucopurulent and mucous discharge on the surface of the pharyngeal tonsil.In all groups, there was an improvement in the condition of the mucous membrane of the pharyngeal tonsil. Pre-hyperemia decreased to 35%, 35.3% and 38%, respectively. By the 7th day of the disease in group 1, the condition of the mucous membrane of the pharyngeal tonsil was completely normalized in 75% of cases. Moderate hyperemia was pronounced in 27.5% of patients, and in one (2.5%) patient it remained severe. In group 2, the condition of the pharyngeal tonsil mucosa was fully restored in 90.2% of cases. Moderate hyperemia was observed in 7.8% of patients, and in one patient it remained pronounced. In group 3, it was completely restored, consisting of the information provided, I cannot unambiguously determine what type of inflammatory process is meant. However, based on the described symptoms and changes during treatment, it can be assumed that we are talking about the treatment of an infectious process in the pharyngeal tonsil (tonsillitis).For example, an improvement in nasal breathing difficulties and a decrease in discharge on the surface of the pharyngeal tonsil indicate a positive dynamics of inflammation. In group 3, complete recovery of nasal breathing was noted, and purulent and mucopurulent discharge was completely absent. Positive changes were also observed in groups 1 and 2, but in some cases, the discharge on the surface of the pharyngeal tonsil was still present.Regarding the condition of the mucous membrane of the pharyngeal tonsil, all groups of patients showed improvement. The preliminary hyperemia decreased, and by the 7th day of treatment, the condition of the mucous membrane of the pharyngeal tonsil returned to normal in most patients.The analysis of bacteria after treatment in three groups of patients revealed the following features. Staphylococcus aureus, Streptococcus pneumoniae and Haemophilus influenzae were most common in monocultures. Group 1 was characterized by a high incidence of Staphylococcus aureus (3 cases), Haemophilus influenzae (3 cases) and Klebsiella pneumoniae (2 cases). Group 2 had Streptococcus viridans (1 case). Group 2 was distinguished by the presence of Staphylococcus aureus + Klebsiella pneumoniae (1 case), while group 1 was characterized by Staphylococcus aureus + Streptococcus viridans (1 case). Group 3 had only 1 case of Staphylococcus aureus. The analysis of associations of microorganisms (3 pathogens) did not reveal significant differences. The results obtained indicate differences in the composition of microorganisms in each group. The use of propolis tincture in combination with photodynamic therapy in the third group showed the best results among all three groups.Long-term monitoring of 140 children receiving conservative treatment and 11 operated children for 12 months after completion of treatment for chronic adenoiditis showed the following results. 7 children from the first group (17.5%) underwent adenotomy. Hypertrophy of pharyngeal tonsils of the 3rd degree with signs of exudative otitis media was in 4 (7.8%) patients from the second group, and hypertrophy of pharyngeal tonsils of the 2nd degree with signs of exudative otitis media was observed in 6 (4.3%) children from groups 1, 2 and 3.After surgery, all the operated children had improved nasal breathing and hearing, as well as the absence of recurrence of adenoiditis. All patients demonstrated type "A" on tympanograms. 22 children had recurrent adenoiditis within a year after treatment: a single episode of recurrence was recorded in 5 (6.7%) children, two episodes in 12 (16.2%) children, and three episodes in 5 (6.7%) children. With exacerbation of adenoiditis, appropriate etiological treatment was carried out, and during the year there were no cases of exudative otitis media among children with recurrent adenoiditis.The analysis showed that the etiological treatment given to patients of the second group significantly reduces the likelihood of relapses during the year. In children of the third group, no more than two episodes of adenoiditis were observed during the year after treatment, which also indicates the positive effect of using propolis tincture in combination with photodynamic therapy.However, it should be noted that the results of this study are based on a small sample of patients and require confirmation in larger studies. In addition, the effectiveness of propolis tincture and photodynamic therapy may vary depending on the individual characteristics of patients.In general, this study indicates the potential usefulness of propolis tincture in combination with photodynamic therapy in the treatment of chronic adenoiditis, especially in patients with certain microbial compositions. However, before making a decision on treatment, it is necessary to consult with a doctor in order to assess the benefits and risks of this approach in an individual case.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML