-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 959-963
doi:10.5923/j.ajmms.20241404.33
Received: Mar. 3, 2024; Accepted: Apr. 8, 2024; Published: Apr. 11, 2024

The Attitude of Suicides Suffering from Disabling Somatic Diseases to Their Illness and Treatment
Tursunkhodjayeva L. A.1, Ergasheva Y. Y.2
1Tashkent Institute of Advanced Medical Training, Tashkent, Uzbekistan
2Bukhara State Medical Institute, Uzbekistan, Bukhara, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Treatment of patients with chronic diseases is one of the main tasks of medicine of the future. It is known that the patient's attitude to his illness and treatment is extremely important for the effectiveness of medical care. The present study is aimed at clarifying the attitude of persons suffering from somatic disease and showing suicidal tendencies in behavior to their illness and treatment. A comparative study of the peculiarities of the perception of their disease was carried out in 327 patients with disabilities (group 1 – 277 patients) and non–disabled (group 2 - 50 patients) for endocrine diseases and malignant neoplasms. It is established that the attitude to the disease and motivation for treatment have a significant impact on the formation of suicidal behavior. The risk of suicidal actions is reduced if there is trust in doctors, faith in the weakening of the symptoms of the disease, patients' attempts to learn how to cope with them on their own, and the desire to improve interpersonal interactions. Passive behavior strategy correlates with a greater severity of suicidal tendencies. At the same time, the presence or absence of disability due to a somatic disease plays a secondary role.
Keywords: Suicidal behavior, Endocrine diseases, Malignant neoplasms, Disability, Attitude to the disease and treatment
Cite this paper: Tursunkhodjayeva L. A., Ergasheva Y. Y., The Attitude of Suicides Suffering from Disabling Somatic Diseases to Their Illness and Treatment, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 959-963. doi: 10.5923/j.ajmms.20241404.33.
1. Introduction
- Chronic diseases are the leading cause of death in the world and, according to forecasts, their frequency will increase, causing an increase in disability rates. Current data indicate that the risk of suicide in people suffering from chronic diseases such as malignant neoplasms, cirrhosis of the liver, kidney or heart failure is significantly higher than in the general population [1,2,3,4]. The diagnosis of a disease classified as incurable turns the fact of the disease into a serious mental trauma that can form mental disorders of a psychogenic-reactive nature. On the other hand, severe somatic illness is accompanied by physical asthenia, which significantly affects mental activity and forms somatogenic mental disorders [5]. At the same time, the opinion is expressed that the manifestations of psychological shifts and the severity of mental disorders practically do not correlate with the severity of the somatic disease, and even suicidal attempts cannot reflect the objective severity of the condition, since both an objective event and a person with the specifics of their attitude to this event participate in the process of mental experience.In countering a chronic disease, there are two strategies of behavior – active and passive [6]. The patient should realize the general change in the living situation and try to actively overcome obstacles with the help of a new lifestyle adapted to the disease. The requirement to "live with the disease" leads to the fact that many people react to changes in their functioning with such psychopathological disorders as fear, apathy, depression. Passive behavior includes defense mechanisms: reactions of downplaying the severity of the disease, such as ignoring, self-deception, rationalization or overcontrol.In chronic diseases, the lack of lifestyle modification and non-compliance with the medication regimen is a serious health problem [7]. Compliance with these conditions, in turn, largely depends on the attitude of patients to their disease, the attitude to treatment and trust in medical professionals.Patients often stop taking medications due to the fact that they consider them ineffective or experience unpleasant side effects [8,9]. Educational activities and behavioral techniques can improve patient compliance with the treatment regimen, but improving communication between the patient and the doctor remains one of the most effective strategies. However, little attention is still paid to the study of relationships in the doctor-patient system.
2. Material and Methods
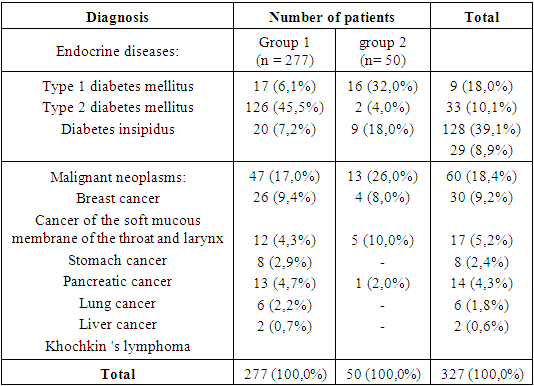
- 327 patients (180 men and 147 women) suffering from diseases of the endocrine system and malignant neoplasms of various organs were examined on the basis of the Bukhara Regional Endocrinological Hospital, regional VTEC and district polyclinics. The criteria for inclusion of patients in the study were: age over 21 years, satisfactory general condition, providing the ability to communicate with the researcher and fill out the questionnaire, the availability of voluntary informed consent for testing.A card was filled in for each patient, reflecting demographic data (age, gender, level of education, religious affiliation) and clinical information (time since diagnosis, awareness of the diagnosis, stage of the disease, characteristics of suicidal behavior, attitude to the disease). The age of patients at the time of examination ranged from 27 years to 71 years. The majority of the surveyed had secondary (41.0%) or specialized secondary (37.3%) education. The share of people with higher education was 21.7%. All patients were adherents of the Muslim religion, observed religious rites and commandments.Of the examined 277 (84.7%) had disability of groups I, II, III for somatic disease. Disability has not been established in 50 (15.3%) patients. By the time of the examination, 80 patients (28.9% of the number of persons with disabilities) had a disability group established for the first time in their lives, the rest had been on disability for several years, had been hospitalized at least five times and had been treated on an outpatient basis multiple times.In order to identify the main options for treatment settings, as well as to diagnose the motives that prompted patients to seek medical help, the questionnaire “Attitude to the disease and treatment” was used [6]. The questionnaire contains 22 statements in respect of which the patient must determine whether they are suitable for him. Each statement corresponds to 5 answer options: "absolutely not suitable", "not suitable", "rather not suitable", "rather suitable", "suitable", "perfectly suitable", which are evaluated in points from 1 to 6. The evaluation of the results is carried out using a special key. Points were awarded according to the following scheme: "absolutely not suitable" – 1 point, "not suitable" – 2, "rather not suitable" – 3, "rather suitable" – 4, "suitable" - 5, "perfectly suitable" – 6 points. The assessment of the severity of each of the five types of motivation consists of the sum of the points of the statements included in it. The technique allows us to identify five types of treatment settings: "setting to achieve insight", "setting to change behavior", "setting to achieve symptomatic improvement", "setting to receive a "secondary gain" from the disease (including hospital stay)", "other motivation (including passive position)", and also highlight the dominant option among them.The risk of suicidal behavior was assessed using the Beck questionnaire “Scale of suicidal thoughts". The Beck scale allows us to state both the presence, frequency and duration of suicidal thoughts, and the activity of suicidal intentions, as well as the presence of factors constraining their implementation. The maximum number of points on the Beck scale is 38, the higher the risk of suicide, the greater the amount of points received during the interview.The period of direct observation of the features of suicidal behavior in patients with chronic somatic diseases was 6 months. Testing was carried out in two groups: group 1 consisted of 277 patients with disabilities, group 2 – 50 patients without disabilities due to chronic somatic disease. The duration of the disease from the moment of diagnosis in group 1 patients ranged from 1 year to 3 years, in group 2 patients – from 1 year to 5 years. All patients were aware of their diagnosis. The distribution of the examined patients depending on the diagnosis of somatic disease is shown in
|
3. Research Results
- In the course of the study, we sought to determine whether the attitude to their illness and treatment differs in patients of groups 1 and 2, whether the disease is the main motive of suicidal behavior, what role disability plays in the formation of suicidal tendencies, for the subsequent selection of optimal approaches to providing psychotherapeutic care to patients suffering from chronic somatic diseases.Analysis of the survey results using the questionnaire “Attitude to illness and treatment” showed that the majority of patients in both groups tend to underestimate the severity of their disease. Their condition was considered so severe that they would not be able to function normally soon, only 39.0% of group 1 patients and 48.0% of group 2 patients (p > 0.05). The rest (61.0% of group 1 patients and 52.0% of group 2 patients; p > 0.05) denied its severity, despite being aware of their diagnosis or disability. It is characteristic that the proportion of such patients turned out to be more significant in group 1, where the manifestations of endocrine or oncological pathology differed in a more severe course. Underestimation of the severity of their condition indicated the presence in a large number of patients of an anosognosic reaction to their disease, disbelief in the correctness of the established diagnosis under the influence of actualization of psychological defense mechanisms.Many patients (53.4% of group 1 patients and 54.0% of group 2 patients; p > 0.05) expressed hope that specialists would finally discover the true nature and causes of their malaise. Most of these patients (48.4% of group 1 patients and 46.0% of group 2 patients; p > 0.05) expressed a desire to gain confidence in the true nature of their disease, since they had previously been diagnosed with different diagnoses, often contradicting each other.The majority of patients in both groups (54.9% of patients in group 1 and 56.0% of patients in group 2; p > 0.05) often experienced anxiety due to the uncertainty of their disease, the intensity of which decreased in hospital conditions. This is largely due to the construction of a compensatory system of psychological protection such as: “They won't let me die in the hospital.”At the same time, the majority of patients (52.3% of group 1 patients and 54.0% of group 2 patients; p > 0.05) agreed to treatment only under the pressure of relatives, hoping that during treatment they would learn to cope with their symptoms on their own (54.9% of group 1 patients and 52.0% of group 2 patients; p > 0.05). Less often (40.1% of group 1 patients and 42.0% of group 2 patients; p > 0.05) they sought help from a medical institution on the recommendation of doctors. Part of patients (48.7% of group 1 patients and 48.0% of group 2 patients; p > 0.05) would like to get acquainted with modern methods of treating their disease in well-known clinics, feeling distrust of the treatment being carried out due to the lack of a noticeable therapeutic effect. But a significant proportion of patients of both groups (56.0% of patients of group 1 and 42.0% of patients of group 2; p > 0.05) continued to believe in treatment, hoped for the appearance of former energy and restoration of working capacity. At the same time, 48.0% of group 1 patients and 50.0% of group 2 patients (p > 0.05) counted on the help of doctors, while 45.9% of group 1 patients and 48.0% of group 2 patients (p > 0.05) declared their awareness of which treatment method could help them and demanded its use.The analysis of the results of the questionnaire "Attitude to illness and treatment" also showed the presence in some patients of the desire for self-isolation, manifested in the difficulty of contacts with others (52.3% of patients of group 1 and 52.0% of patients of group 2; p > 0.05), not bringing a sense of satisfaction. Some patients noted the need to hide in a safe place from worries and worries (40.0% of group 1 patients and 38.0% of group 2 patients; p > 0.05), as well as feelings of resentment at the injustice of fate with a pessimistic assessment of the future (44.8% of patients in group 1 and 46.0% of patients in group 2; p > 0.05).In addition, it was possible to judge about the change in attitude not only to the external, but also to the internal world, the presence of an active struggle of the individual with a dangerous disease in some patients. Thus, 56.7% of patients of group 1 and 56.0% of patients of group 2 (p > 0.05) believed that the condition for alleviating their problems is deep self-knowledge, cognition and analysis of their own attitudes and attitudes towards other people (44.4% of patients of group 1 and 42.0% of patients of group 2; p > 0.05), and also to other aspects of life (48.7% of group 1 patients and 52.0% of group 2 patients; p > 0.05). In some cases, patients stressed that the situation of the disease puts them "outside of real life" (43.0% of patients in group 1 and 38.0% of patients in group 2; p > 0.05) and hoped to change their attitude to the environment as a result of hospital stay and receiving professional help from specialists (39.4% of patients in group 1 and 38.0% of patients 2 groups; p > 0.05).Thus, the analysis of the attitude to the disease and treatment in a group of patients with an established disability and a more severe somatic status in comparison with a group of patients without disabilities for the same diseases did not find statistically significant intergroup differences. Most patients of both groups continued to express doubts about the correctness of the established diagnosis, did not believe in the incurable nature of their disease, doubted the professional competence of doctors and the adequacy of the therapy. In the conversation, they stressed that they trusted doctors with an academic degree or a higher medical category more, who did not receive bonuses from pharmaceutical companies and worked in prestigious clinics.The analysis of motivation for treatment showed that the passive position was dominant in most patients (69.5% of group 1 patients and 46.0% of group 2 patients; p < 0.003), which was statistically more common in group 1 patients and was characterized by underestimation of the severity of their condition, distrust of doctors or their diagnosis, the forced nature of hospitalizations with the purpose of re-examination of the disability group or in accordance with the insistent demands of relatives. Some patients were attracted by the possibility of free laboratory and instrumental examination and treatment in public medical institutions due to financial problems.In patients of group 1, the second most frequent occurrence (19.6%), the dominant motivation was the desire to receive a “secondary gain” from the disease (including from hospital stay), including the desire to change the attitude of loved ones, attract attention to themselves, get rid of anxiety, get away from life's troubles and worries. Such patients showed a tendency to exaggerate the severity of their condition and rental settings. In group 2 patients, such motivation for treatment was less common (14.0%; p > 0.05), but the intergroup differences did not have statistical significance.Motivation to get symptomatic improvement dominated in only 8.7% of group 1 patients, with statistical reliability increasing in group 2 patients (34.0%; p < 0.001). Such patients pinned their hopes on the help of doctors in eliminating the symptoms of the disease that caused them suffering, and tried to learn how to cope with them on their own.Finally, the rarest dominant motivation was an attitude towards achieving “insight” (2.2% of patients in group 1 and 6.0% of patients in group 2; p > 0.05) with the desire to know themselves more deeply, clarify their attitude to the surrounding reality and other people in order to improve interpersonal contacts and interaction with loved ones.An interesting fact is that in both groups there were no patients with a dominant motivation to change behavior, which is characterized by the desire to overcome life difficulties independently, improve contacts with others, faith in treatment and restoration of lost strength and efficiency. Such motivation could indicate an active struggle of the individual with the disease and be the most favorable for carrying out therapeutic measures, maintaining adequate relations in the doctor-patient system and the patient's compliance with the treatment regimen.The study of the severity of suicidal tendencies on the Beck scale in patients suffering from endocrine diseases and malignant neoplasms showed that passive suicidal thoughts, that is, ideas and fantasies on the topic of their death (but not on the topic of taking their own life as a spontaneous action) were more often observed with statistical reliability in patients without disabilities (31.9% of patients group 1 and 60.0% of group 2 patients; p < 0.001). The frequency of suicidal thoughts with thinking over the method of suicide had no significant intergroup differences (33.3% of patients in group 1 and 32.0% of patients in group 2; p > 0.05), as well as the frequency of suicidal intentions (13.4% of patients in group 1 and 8.0% of patients in group 2; p > 0.05). However, during the period of direct observations of 21.4% of group 1 patients attempted suicide, while there were no such patients in group 2 (p < 0.001).The analysis of the correlation between the severity of suicidal tendencies and the dominant motivation for treatment revealed the presence of an average strong connection (Pearson's conjugacy coefficient C = 0.49; p < 0.001). With the dominance of motivation to achieve “insight” or symptomatic improvement, suicidal tendencies, as a rule, were limited to passive suicidal thoughts or suicidal intentions without an active desire to implement them. The greatest risk of suicidal actions was observed in patients with the dominance of a different motivation for treatment, including a passive position, who lost faith in the possibilities of medicine, showed distrust of doctors, diagnosis, suffered from disturbed interpersonal relationships and loss of previous social ties. The relationship of the severity of suicidal tendencies with the dominant motivation for treatment turned out to be closer than with the severity of the somatic condition and the presence or absence of disability (C = 0.24; p < 0.001).The obtained results indicate the need to change the attitude to the disease and the motivation for treatment in patients suffering from endocrine diseases and malignant neoplasms to prevent suicidal actions in patients with a high risk of suicidal behavior, including repeated suicide attempts. The possibility of such changes is created by the use of motivational technologies and cognitive behavioral psychotherapy.
4. Conclusions
- The attitude to the disease and motivation for treatment have a significant impact on the formation of suicidal behavior of patients suffering from endocrine diseases and malignant neoplasms. The risk of suicidal actions is reduced if there is trust in doctors, faith in the weakening of the symptoms of the disease, patients' attempts to learn how to cope with them on their own, the desire to know themselves more deeply, clarify their attitude to the surrounding reality, improve interpersonal interactions. Passive behavior strategy correlates with a greater severity of suicidal tendencies. At the same time, the presence or absence of disability due to a somatic disease plays a secondary role.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML