Polatova Djamilya Shogayratovna1, Alimov Ijod Rustamjonovich2, Khamrokulov Bekzod Bahodirovich3
1Doctor of Medical Sciences, Head of the Department of Oncology and Medical Radiology, Tashkent Dental Institute, Tashkent, Uzbekistan
2Doctor of Philosophy in Medical Sciences, Associate Professor, Department of Neurosurgery, Center for the Development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
3Basic Doctoral Student, Department of Neurosurgery, Center for the development of Professional Qualification of Medical Workers, Tashkent, Uzbekistan
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
Analysis of the effectiveness of a differentiated approach to the surgical treatment of oncological lesions of the vertebrae at different stages of the disease. At the Center for the Development of Professional Qualifications of Medical Workers and the Republican Specialized Medical Center of Oncology and Radiology from 2017 to 2021 54 patients with oncological diseases of the spine were treated. Of these, there were 17 men (31.5%), 37 women (68.5%). The age of the patients varied from 18 to 55 years. The average age of patients was 36 years. As diagnostic measures, in addition to general clinical and laboratory studies, patients underwent instrumental methods of examination, such as spondylogram, MRI, MSCT, skeletal bone scintigraphy, as well as all the necessary diagnostic options for oncosearch in the body. The results of treatment of 54 patients with tumor lesions of the spine were evaluated taking into account the 5-year survival rate after the identified oncological process and assessment of their quality of life according to the Karnofsky scale. A differentiated approach in choosing the tactics of treating oncological lesions of the vertebrae contributes to the correct restoration of the lost function of the spine and spinal cord. Based on the results of the work, it follows that with multiple malignant tumors of the vertebrae, it also makes sense to carry out surgical care in order to improve the quality of the patient's remaining life. The correct selection of surgical intervention tactics for spinal cancer creates a condition for a complete cure of the patient or a long-term preservation of the quality of his remaining life.
Keywords:
Tumors of the spine, Surgical treatment, Spondilodesis, Corporodesis, Vertebroplasty
Cite this paper: Polatova Djamilya Shogayratovna, Alimov Ijod Rustamjonovich, Khamrokulov Bekzod Bahodirovich, Tactics of Surgical Treatment of Tumor Lesions of the Spine, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 955-958. doi: 10.5923/j.ajmms.20241404.32.
1. Introduction
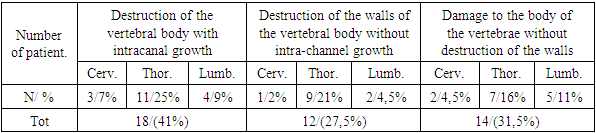
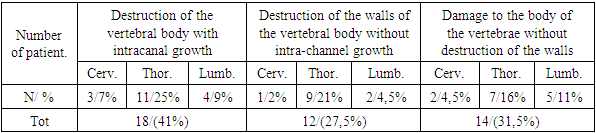
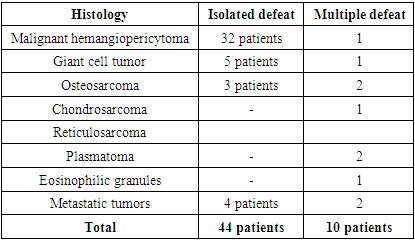
The increase in cancer of the world's population is observed among all organs and systems, in particular the lesion of the musculoskeletal system [6]. Among the tumors of the bone skeleton, the lesion of the vertebral column is 5% [7]. In the structure of spinal tumors, the vast majority are metastatic lesions of the vertebrae (96%), primary tumors of the spine are much less common (4-5%) [3,8]. Tumor damage of the vertebrae, as well as other parts of the musculoskeletal system, leads to early disability of patients with a sharp reduction in their quality of life. At the same time, the rehabilitation of this category of patients is very difficult, patients are forced to observe the rest regime for a long time, are limited in movements, which in turn is the cause of secondary complications from the cardiovascular system, trophic disorders of the skin. Lethal complications in patients who are on long-term rehabilitation with bed rest are 12-18% [4,9]. The issues of treatment tactics of this category of patients are still being studied by the world's leading medical institutions [2,5]. Despite this, today there are many controversial issues regarding the radical nature of surgical treatment, the timing and duration of combined treatment, as well as their further rehabilitation [1].In Center for the development of professional qualification of medical workers and Republican specialized scientific and practical medical center of oncology and radiology from 2017 to 2022, 54 patients with tumor lesions of the spine were treated. Of these, men 17 (31.5%), women 37 (68.5%). The age of the sick ranged from 18 to 55 years. The average age of patients is 36 years.In addition to general and lab diagnostic studies, patients underwent intual examination methods such as spondylogram, MRI, MSCT, PET scintigraphy of skeletal bones.Among the topical location of the pathological process in the spine, there was an isolated and multiple lesion of the vertebrae. Of these, 44 patients with isolated vertebral lesions, 10 patients with multiple. Among the number of patients with isolated lesions, in 6 (13%) patients the pathological process was located in the cervical spine, in 27 (61%) patients in the thoracic spine, in 11 (25%) patients in the lumbosacral spine. Among 10 patients with multiple spinal lesions, 3 (30%) patients in the cervical and thoracic spine, 5 (50%) patients in the thoracic and lumbar spine, 2 (20%) patients had lesions of the cervical, thoracic and lumbar-sacral spine. In 8 patients with multiple vertebral lesions, the pathological process was also detected in other parts of the bone skeleton according to scintigraphy in the form of metastases.Also, of the listed number of 44 patients with isolated lesions of the vertebral column, in 18 (40.5%) patients the pathological process spread beyond the spine intracanal (3 patients in the cervical spine, 11 patients in the thoracic spine, 4 patients in the lumbar spine) in 12 (27.5%) patients there was the destruction of the walls of the vertebrae without intracanal growth of the tumor (1 patient in the cervical spine, 9 patients in the thoracic part of the lumbar spine, 2 patients in the lumbar spine), the remaining 14 (32%) patients the lesion was limited to the body of the vertebrae without destruction of their walls (2 patients in the cervical spine, 7 patients in the thoracic spine, 5 Patients in the lumbar spine) (see table 1). Pathological fracture of vertebral bodies of 2-3 degrees as a result of their destruction was observed in 12 (27.5%) patients.Table 1. Topical characteristics of patients with isolated lesion of vertebral bodies
 |
| |
|
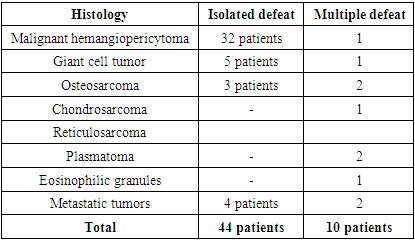
Of the listed number of 10 patients with multiple lesions of the spine, among 3 (30%) patients with lesions of the cervical and thoracic spine, in 1 patient, the pathological process in the cervical vertebra spread beyond the vertebra intracanally, in the remaining 2 patients the process proceeded without destruction of the walls of the body of the vertebra. Among 5 (50%) patients with lesions of the thoracic and lumbar spine, 2 patients had intra-channel distribution of tumors from the lumbar vertebrae, one patient had destruction of the thoracic vertebra wall, 2 patients had vertebral lesions without destruction of their walls. Among 2 (20%) patients with multiple lesions of the cervical, thoracic and lumbar spine, the lesion was limited by the body of the vertebrae without destruction of their walls.In all patients, the main clinical sign of the disease was severe pain in the spine in accordance with the localization of the pathological process. In addition, 18 (33%) patients with intracanal tumor growth had neurological disorders in the form of paraparesis, root pain, pelvic dysfunction, sensitivity loss. Neurological disorders corresponded to the localization of compression of spinal cord structures. In 2 (4%) patients, despite the absence of a squeezing factor in the spinal cord canal in the thoracic region, there was a lower parparesis, which is associated with circulatory disorders of this area of the spinal cord in the form of "snealing".All 54 patients received surgical care. The tactics of surgical intervention were determined in accordance with the following indicators:- localization of the pathological process - number of affected vertebrae- presence of intrachannel growth- the presence of lesions of the vertebral walls- the presence of distant metastases- the presence of severe concomitant diseasesIn isolated vertebral lesions, surgical treatment of 18 (40%) patients with intracanal tumor growth was carried out by open surgical means. At the same time, 3 patients with cervical spine lesions underwent an anterior corporectomy with a new implant spondylodesis. 11 patients with a thoracic spine underwent surgical treatment with a combined method in the form of a laminectomy with the removal of the tumor with the subsequent open vertebroplasty of the affected vertebra with bone cement and spondylodesis by the TPF system. 4 patients with lesions of the lumbar spine also underwent combined surgical treatment, three of them underwent the operation by the above method, one patient with complete destruction of the structure of the vertebra, underwent an anterior lateral corporectomy, spondylodesis with an interbody implant and the Z-plate system, laminectomy of the affected vertebrae and spondectomy with the TPF system.Among 12 (27%) patients with the presence of vertebral wall destruction without intracanal growth, open surgical operations were also performed. 1 patient with cervical vertebra lesions anterior corporectomy with spondylodesis titanium implant. 9 patients with thoracic spine lesions and 5 patients with lumbar spine lesions underwent a combined surgical treatment in the form of laminectomy with a biopsy of the affected vertebra, an open vertebroplasty with bone cement with subsequent spondylode with TPF system. 14 (31%) patients with a pathological process in the body without destruction of the walls of the vertebrae underwent surgical treatment by percutaneous vertebroplasty after preliminary biopsy of the affected vertebral body.With multiple vertebral lesions, surgical treatment 1 (10%) for patients with presence of intracranial growth of tumors from cervical vertebra and 1 (10%) to the patient with the presence of intracranial growth from lumbar vertebrae held open surgically. At the same time, the patient with Cervical vertebral lesion conducted anterior cortectomy with spondy titanium implant. Patient Lumbar vertebrae with in- Translucent growth surgical treatment combined method in Laminectomy with the removal of tumors subsequent open vertebroplasty A vertebral bone cement and spondylodesis system TPP. Both operas were carried out by patients of age up to 45 years of age to improve quality the rest of his life, despite the process in other vertebrae and sites. One (10%) patient with a lesion of the lumbar vertebrae with intracranial growth was not operated openly due to the presence of severe concomitant diseases, the patient performed a puncture biopsy of the affected vertebrae to verify the pathological process.Among the other 7 (70%) of patients with multiple spinal lesions, the percutaneous vertebroplasty method was performed by 4 patients, with 2 patients having 3 vertebrae lesions in the thoracic lumbar region, both patients having surgery on all affected vertebrae. In 2 patients, percutaneous vertebral plasty was limited to one vertebrae, as the destructive process in the other affected vertebrae was negligible. All patients with percutaneous vertebroplasty biopsied time-vertebral section for histological verification. 2 patients with process lesions in the cervical, thoracic and lumbar spine at the same time.A punctuation biopsy of the bodies of the affected vertebrae without further vertebral fibrosis sticks, given the extent of the process in the spine and the number of injuries vertebrae. All patients treated with tumor histological verification (Table 2).Table 2. Histological characteristics of the affected vertebrae
 |
| |
|
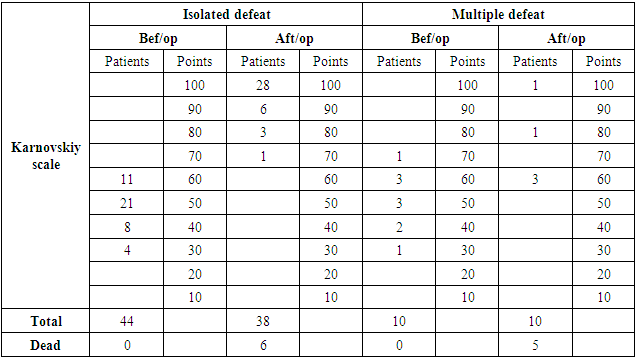
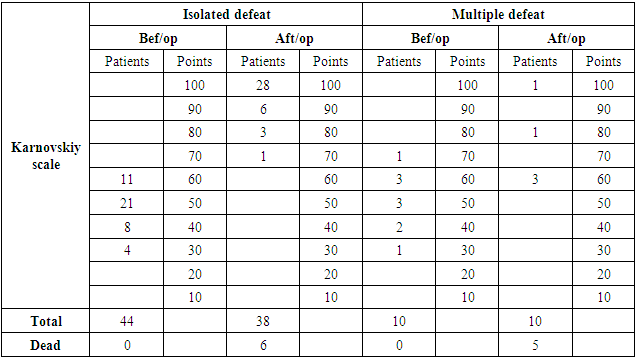
54 patients were diagnosed by histological examination various variants of malignant tumors.During the period of observation of lethal cases 11. At the same time, one patient with metastatic tumor died 8 months after the operation, 4 patients lived after the operation more than 2 years, 6 patients more than 3 years. The remaining 3 patients under supervision receive specialized treatment from oncologists periodically. Two patients with gigantic cell tumor have relapse growth.One of them had an increase for 12 months of observation, the other for 30 months. Since the relapse of the tumor does not affect the quality of life of patients due to the small growth of a vertebral tumor ventral, repeated operative treatment is delayed, further observation is carried out according to the Karnovsky scale, made in the fifth year after the surgery (Table 3) the quality of patients' lives is maintained at more than 50 points, which indicates that the postoperative quality of the remaining quality of the patient life.Table 3
 |
| |
|
2. Conclusions
A differentiated approach to the choice of tactics for the treatment of tumor lesions of the vertebrae contributes to the correct restoration of the lost function of the spine and spinal cord. Relief of pain syndrome. According to the results of the work, it follows that in multiple malignant tumors of the vertebrae it also makes sense to carry out surgical treatment in order to improve the quality of life of the patient. The correct selection of surgical tactics for tumor lesions of the spine creates a long-term improvement in the patient's quality of life.
References
| [1] | Curtis A. Dickman, Michael G. Fehlings, Ziya I. Gokaslan. // Spinal Cord and Spinal Column Tumors – Thieme verlagsgruppe 2010. |
| [2] | Gilardi L. Intramedullary spinal cord metastases from breast cancer: detection with 18F-FDG PET/CT / L. Gilardi, S. Vassallo, M. Colandrea et al. // Ecancer. – 2013. – Vol. 7. – Р. 329. |
| [3] | McGraw JK, Gardella J, Barr JD, Mathis JM, et al. Society of Interventional Radiology Quality Improvement Guidelines for Percutaneous Vertebroplasty // J Vasc Interv Radiol 2003. |
| [4] | Smith A. B. Radiologic-pathologic correlation of pediatric and adolescent spinal neoplasms: Part 1, Intramedullary spinal neoplasms / A. B. Smith, K. A. Soderlund, E. J. Rushing // Am. J. Roentgenol. – 2012. – Vol. 198, No 1. – Р. 34–43. |
| [5] | Thomas, D. M., & Skubitz, T. Giant-cell tumour of bone. Current Opinion in Oncology, 2009; 21, 338–344. |
| [6] | Валиев А.К., Мусев Э.Р. Сушенцов Е.А., Алиев М.Д., Хирургическое лечение метасттического поражения костей. Практическая онкология 2011. |
| [7] | Зозуля Ю.А., Слынько Е.И., Шамаев М.И., Чеботарева Л.Л., Чепкий Л.П. и др. Опухоли спинного мозга и позвоночника. Киев 2010г. |
| [8] | Прахова Л. Н. Возможности комплексного диагностического обследования при проведении дифференциальной диагностики воспалительных и опухолевых поражений спинного мозга (два клинических наблюдения) / Л. Н. Прахова, Ж. И. Савинцева, А. Ф. Гурчин и др. // Журнал неврол. и психиатр. - 2012. – No 9 (2). – С. 87–94. |
| [9] | Усиков В.Д., Пташникова Д.А., Магомедов Ш.Ш. и др. чрезкожная вертебропластика у больных с метастазами в позвононик. Травматология и ортопедия. Россия 2008. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML