-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2024; 14(4): 964-967
doi:10.5923/j.ajmms.20241404.34
Received: Mar. 18, 2024; Accepted: Apr. 8, 2024; Published: Apr. 11, 2024

Features of Hemostasis in Women with MenstruaL-Ovarian Cycle Disorders Against the Background of COVID-19
Yuldasheva N. Z.1, Shukurov F. I.2
1Assistant of the Department of Obstetrics and Gynecology Termez branch, Tashkent Medical Academy, Tashkent, Uzbekistan
2Doctor of Medical Sciences, Head of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: Shukurov F. I., Doctor of Medical Sciences, Head of the Department of Obstetrics and Gynecology, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The study included 120 women with menstrual-ovarian cycle disorders against the background of COVID-19. According to the clinical course of COVID-19, all patients were divided into three groups. The first group consisted of 45 women (37.5%) with a mild form of COVID-19, the second group included 43 women (35.8%) with moderate COVID-19, and the third group comprised 32 women (26.7%) with severe COVID-19. The study results demonstrate a significant impact of COVID-19 on the hemostasis state in 92% of women with menstrual-ovarian function disorders against the background of COVID-19. The levels of fibrinogen are 1.8 times and D-dimer on average 2.0 times higher than in healthy women. A correlation has been established between the levels of D-dimer, fibrinogen, and the severity of the clinical course of COVID-19, specifically, the presence of a direct correlation of these indicators with the severe form of COVID-19.
Keywords: Hemostasis, Women, MenstruaL-Ovarian Cycle Disorders, COVID-19
Cite this paper: Yuldasheva N. Z., Shukurov F. I., Features of Hemostasis in Women with MenstruaL-Ovarian Cycle Disorders Against the Background of COVID-19, American Journal of Medicine and Medical Sciences, Vol. 14 No. 4, 2024, pp. 964-967. doi: 10.5923/j.ajmms.20241404.34.
1. Introduction
- In recent years, the world has faced an unprecedented challenge in the form of the COVID-19 pandemic caused by the SARS-CoV-2 virus [1-3]. This pandemic has had a significant impact on all aspects of healthcare, including women's reproductive health. The SARS-CoV-2 virus demonstrates a wide range of clinical manifestations, including effects on the blood system and hemostasis [4-5]. Hemostasis is a complex process that maintains the circulation of stationary blood within the vascular bed, preventing blood loss when vessels are damaged, and also prevents the formation of thrombi within vessels under normal conditions [6-7]. Disorders in the hemostasis system can lead to various pathological conditions, from thrombosis to bleeding. At the same time, a woman's menstrual cycle is closely linked to various physiological processes in the body, including the hemostasis system [8-9]. Menstrual cycle disorders can indicate various diseases and conditions, including hormonal imbalances, reproductive system problems, and even the overall state of health. It is reported that COVID-19 infection can affect the menstrual cycle, causing its disorders, making the study of this topic relevant and necessary for understanding the possible interactions between COVID-19, the menstrual-ovarian cycle, and the hemostasis system [1-11].The relevance of this study is driven by the growing need to understand the features of COVID-19's impact on women's reproductive health, particularly on the menstrual-ovarian cycle and hemostasis [12-14]. Despite extensive research on the impact of COVID-19 on the human body, data on the interaction of the infection with the women's reproductive system and the hemostasis system remain insufficient [15-17]. This creates a necessity for conducting targeted research to identify potential mechanisms of interaction and to develop appropriate methods of prevention and treatment.The aim of this study is to investigate the features of hemostasis in women with menstrual-ovarian cycle disorders against the background of past or current COVID-19 infection.
2. Materials and Methods
- The studies were conducted from 2021 to 2023, involving women aged 18 to 36. The study included 120 women with menstrual-ovarian cycle disorders against the background of COVID-19. According to the clinical course of COVID-19, all patients were divided into three groups. The first group consisted of 45 women (37.5%) with a mild form of COVID-19, the second group included 43 women (35.8%) with moderate COVID-19, and the third group comprised 32 women (26.7%) with severe COVID-19. All participants underwent hemostasis tests, such as thromboelastography, coagulogram, studies of the anticoagulant system, as well as the level of D-dimer. A complex of statistical methods was used for data analysis. Descriptive statistical methods (mean, median, standard deviation) as well as inferential statistics (t-test, analysis of variance (ANOVA), nonlinear methods when necessary) were applied to assess the significance of differences between the groups. The significance level was set at p < 0.05.
3. Research Results
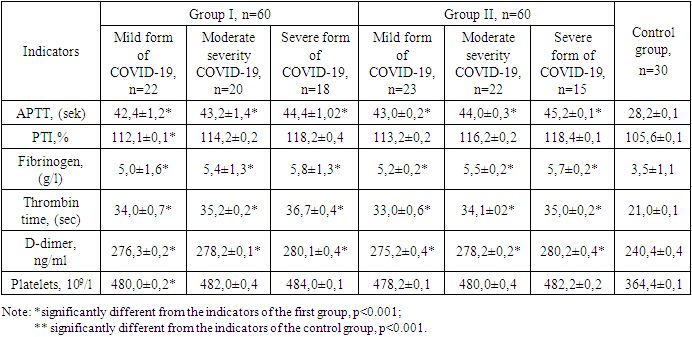
- The study showed that significant changes in the hemostasis system were observed in 87% of women with menstrual-ovarian function disorders against the background of COVID-19, 42% and 45% respectively in the groups. In 73.2% of women in these groups, increased levels of D-dimer and fibrinogen were identified, 34.8% and 38.4% respectively in the groups. An increase in the levels of blood coagulation factors V and VIII was noticed in 24.2%, which may indicate a tendency towards thrombus formation and thromboembolism. Moreover, the study results showed that the state of the hemostasis system in 120 women with menstrual-ovarian function disorders against the background of COVID-19 varies depending on the severity of COVID-19.The APTT analysis in the first group of women with menstrual-ovarian function disorders against the background of COVID-19 showed an increase in this indicator's time, respectively 42.4±1.2, 43.2±1.4, and 44.4±1.02 sec in the subgroups against 28.2±0.1 sec in the control group.The D-dimer level in the first group of women with menstrual-ovarian function disorders against the background of COVID-19 was higher compared to the control group, being respectively 276.3±0.2, 278.2±0.1, and 280.1±0.4 µg/mL against 240.4±0.4 ng/mL in the control group. The fibrinogen level analysis in the first group showed that in the subgroups, this indicator was 5.0±1.6, 5.4±1.3, and 5.8±1.3 g/L against 3.5±1.1 g/L in the control group. It was found that the fibrinogen level increased by 2.0 times in women with menstrual-ovarian function disorders against the background of COVID-19.The PTI analysis in the first group of women with menstrual-ovarian function disorders against the background of COVID-19 showed growth of this indicator in the subgroups, respectively 112.1±0.1, 114.2±0.2, and 118.2±0.4.The study of thrombin time showed that in the first group, this indicator was 34.0±0.7, 35.2±0.2, and 36.7±0.4 respectively in the subgroups. The average level of platelets in the subgroups of the first group was 480.0±0.2, 482.0±0.4, and 484.0±0.1x10^9/L against 364.4±0.1x10^9/L in the control group (see table).
|
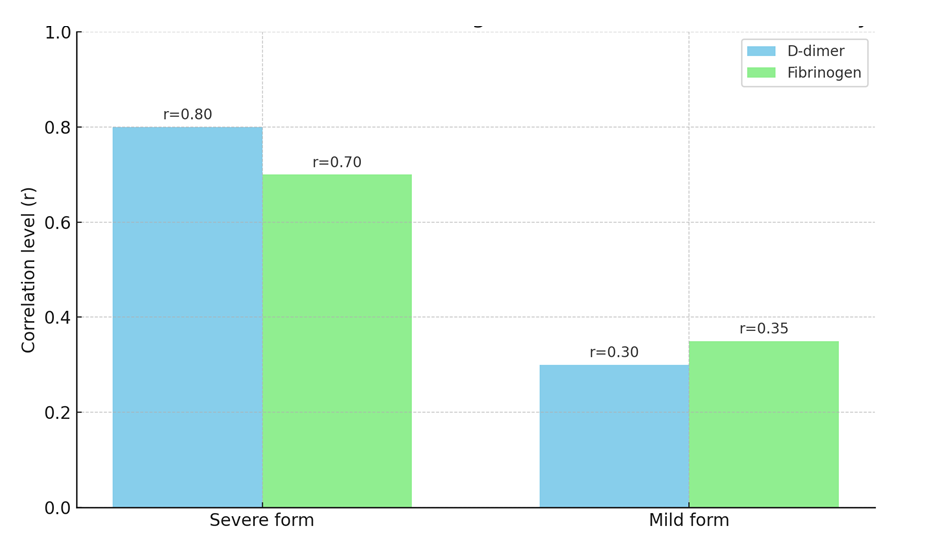 | Figure 1. Correlation between D-dimer and fibrinogen levels and the severity of the clinical course of COVID-19 |
4. Conclusions
- The study results demonstrate a significant impact of COVID-19 on the hemostasis state in 92% of women with menstrual-ovarian function disorders against the background of COVID-19. The levels of fibrinogen are 1.8 times and D-dimer on average 2.0 times higher than in healthy women. A correlation has been established between the levels of D-dimer, fibrinogen, and the severity of the clinical course of COVID-19, specifically, the presence of a direct correlation of these indicators with the severe form of COVID-19. The correlation coefficient was respectively (r=0.80) and (r=0.70), and a weak correlation with the mild form of COVID-19, with the correlation coefficient being respectively (r=0.35) and (r=0.30). Therefore, it is important to conduct research on the hemostasis state in such patients for early detection and prevention of thrombotic complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML