-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(11): 784-787
doi:10.5923/j.ajmms.20211111.08
Received: Oct. 20, 2021; Accepted: Nov. 5, 2021; Published: Nov. 15, 2021

Disorders in the Hemostastic System in the Toxemic Stage of Acute Burning in Persons with Burning Injuries
Oybek Turayevich Yunusov1, Sanjar Abdusalamovich Ruzibayev2, Murodulla Isomiddinovich Rustamov3, Qodir Usmanqulovich Sherqulov1, Shovkat Usmonovich Baysariev1
1Department of General Surgery, Assistant Teacher, Samarkand State Medical Institute, Uzbekistan, Samarkand
2Department of 2 nd Surgical Diseases, Doctor of Medical Sciences, Docent, Samarkand State Medical Institute, Uzbekistan, Samarkand
3Department of General Surgery, Candidate of Medical Sciences, Assistant Teacher, Samarkand State Medical Institute, Uzbekistan, Samarkand
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Thermal injury poses a serious medical, social, and economic problem. The development of heavy industry and chemical industry, as well as the widespread use of electricity in domestic and industrial environments will lead to a significant increase in burn injuries. Purpose. The state of the hemostasis system and blood biochemical parameters were studied in 59 patients aged 18 to 75 years in the acute toxemia phase of burns in the burn area of more than 20% of the body surface in the period 4-5 to 12 days after injury. In 59 patients with severe burns in the acute toxemia phase, we examined the state of the hemostasis system. At the stage of toxemia, we performed various surgical interventions after complex therapy against shock in the main group: 23 necrotomies with deep burns of 11-15% of the body surface, early necrectomy in 40 patients and autodermoplasty in 49 patients. Analysis of the blood coagulation system and fibrinolytic activity after surgical interventions showed a tendency to normalize all parameters.Our studies have shown that early surgical necrectomy and slice autotransplantation show bleeding from donor areas (6-10 ml per 100 cm2 area), sudden application of hemostatic powder Geprotsel completely stops bleeding and the wound surface becomes shiny due to the adhesion of the film takes shape. The sensation of pain is very low. It has been observed that when the wound defect is closed with a donor autoimmune tissue, the skin tissue adheres well to the wound beneath it.In view of the above, comprehensive anti-shock measures aimed at improving water-salt balance, acid-base balance and homeostasis disorders should be carried out when all patients are hospitalized.
Keywords: Disseminated vascular transfusion (DCS) - syndrome, Circulating blood volume (CBV), Recovery time, Antithrombin, Prothrombin index, Burn injury
Cite this paper: Oybek Turayevich Yunusov, Sanjar Abdusalamovich Ruzibayev, Murodulla Isomiddinovich Rustamov, Qodir Usmanqulovich Sherqulov, Shovkat Usmonovich Baysariev, Disorders in the Hemostastic System in the Toxemic Stage of Acute Burning in Persons with Burning Injuries, American Journal of Medicine and Medical Sciences, Vol. 11 No. 11, 2021, pp. 784-787. doi: 10.5923/j.ajmms.20211111.08.
1. Introduction
- Any injury triggers the process of blood clotting, but thermal injuries, which are characterized by shock, lead to abrupt changes in all coagulation systems. Jilinskiy E.V., Tsvirko V.N.2018y. Any damage to the vascular wall, "blood damage", on the one hand, leads to varying degrees of plasma loss, on the other - can be considered physiological, and then pathological changes in the hemostasis system can lead to spontaneous death of the organism. Legitimate severe and common complications of massive injury include acute disseminated vascular hardening syndrome, hemostasis disorder in patients with severe burns is manifested by QDTQ-syndrome. Krylov K.M., Shlyk I.V., Pivovarova L.P., 2010y. Disseminated vascular hemorrhage (DV) - the syndrome is not completely detectable, or is detected at the stage of giving a clear clinical picture, such as hemorrhage and organ dysfunction. There are several forms of QDTQ-syndrome: severe, acute, acute, chronic, recurrent, latent. The acute form is characterized by an acute period of burns.Purpose of the study was to study the disturbances in the hemostasis system in the stage of burn toxemia in patients with burn injuries.
2. Materials and Methods
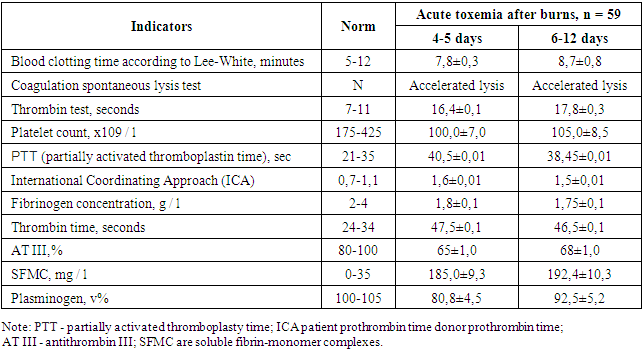
- Coagulation tests in different directions, which are characteristic for the onset of the development of acute DCS-syndrome in the first 4-5 days of burn toxemia in patients after burn injury, were identified (Table 1). This means that if the testosterone ICA, prothrombin time, SFMC values are clearly increased compared to the norm, then fibrinogen, plasminogen and AT-III - decreased, clot dissolution is accelerated. Indications for the development of acute DCS- syndrome were in the form of increased consumption of coagulation substrates - platelets and fibrinogen. In our study, thrombocytopenia occurred in the majority of patients, with a platelet count of 100.0 ± 7 × 109 / l, 32.8% lower than normal (r <0.05), and a fibrinogen level of 1.7 in patients with burn toxemia. times lower. More severe differences between patients with a severe course of burn toxemia and the control group were identified on the basis of one of the markers of thrombinemia: the presence of large amounts of intermediate products of fibrinogen to fibrin transformation in plasma. The amount of SFMC was 5.3 times higher in patients with burn toxemia. In patients with burn shock, significant physiological anticoagulants C were found to be significantly reduced by 1.6 times and AT III by 20% (r <0.05) compared to the norm. In parallel, the amount of plasminogen in the anti-coagulation system decreased by 1.3 times (p <0.05) compared to the norm.
|
3. Results and Discussion
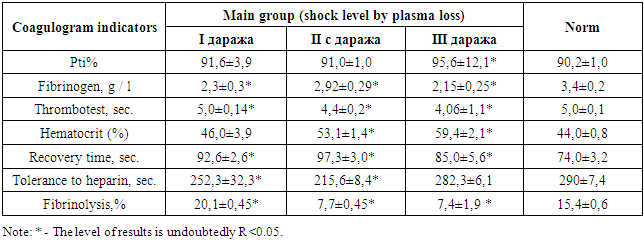
- Disorders of the hemostasis system in the stage of toxemia in patients with burn injuries. Studies showed that a reduction in blood clotting time (5.5 ± 0.5 min) was observed in 15 patients of group 1 (with sepsis). Plasma recalculation time was 66 ± 3.8 seconds and increased to 82 ± 4.2 seconds by the end of the third day. In group 2 patients (with severe sepsi), the blood clotting time was 3.6 ± 0.3 minutes.At this time, plasma recalculation was reduced to 40 ± 5.0 s and by the end of the third day was 76 ± 3.8 s. In group 3 burns (with septic shock refractory hypotension), blood clotting time was 4.0 ± 0.4 minutes and increased to 5.8 ± 0.5 minutes on the third day. Plasma reclamation time was reduced to 33 ± 7.8 seconds on the first day and decreased to 45 ± 3.5 seconds by the end of the third day. In both the 2nd and 3rd groups of the lesions, increased fibrinogen concentrations were found on the first day after burns.Fibrinogen concentrations increased significantly by the first day alone, averaging 5.3 ± 0.3 g / l. The reaction to fibrinogen “V” was sharply positive. The results of studies show that burn injury leads to a decrease in anticoagulant activity of the blood. Similarly, in patients with FI 90 units and above, fibrinolytic activity decreased to 3.7 ± 0.6% in the first days and remained abruptly reduced until the end of the third day.At the stage of toxemia, we performed various surgical interventions after complex therapy against shock in the main group: 23 necrotomies with deep burns of 11-15% of the body surface, early necrectomy in 40 patients and autodermoplasty in 49 patients. Analysis of the blood coagulation system and fibrinolytic activity after surgical interventions showed a tendency to normalize all parameters (Table 2).
|
4. Conclusions
- In view of the above, comprehensive anti-shock measures aimed at improving water-salt balance, acid-base balance and homeostasis disorders should be carried out when all patients are hospitalized.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML