-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(11): 780-783
doi:10.5923/j.ajmms.20211111.07
Received: Oct. 20, 2021; Accepted: Nov. 3, 2021; Published: Nov. 15, 2021

Surgical Treatment of Critical Limb Ischemia at Multifocal Atherosclerosis
Karimov Sh. I., Irnazarov A. A., Rakhmanov S. U., Yulbarisov A. A., Asrarov U. A., Khasanov V. R., Avlanazarov Kh. Kh.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the surgical treatment of patients with critical lower limb ischemia at multifocal atherosclerosis. The results of surgical treatment of 105 patients with critical ischemia of the lower limbs who had hemodynamically significant lesions of the coronary and carotid arterial basins were analyzed. The possibilities of hybrid surgeries at multifocal atherosclerosis have been determined.
Keywords: Critical lower limb ischemia, Multifocal atherosclerosis, Hybrid surgeries
Cite this paper: Karimov Sh. I., Irnazarov A. A., Rakhmanov S. U., Yulbarisov A. A., Asrarov U. A., Khasanov V. R., Avlanazarov Kh. Kh., Surgical Treatment of Critical Limb Ischemia at Multifocal Atherosclerosis, American Journal of Medicine and Medical Sciences, Vol. 11 No. 11, 2021, pp. 780-783. doi: 10.5923/j.ajmms.20211111.07.
1. Introduction
- Multifocal atherosclerosis (MA) is an urgent problem of modern medicine today due to its high medical and social significance. The presence of MA is associated with the severity of the condition, difficulties in choosing the optimal treatment tactics and a negative prognosis [1]. Until recently the main attention in the diagnosis and treatment has been paid to the local manifestation of atherosclerosis in one particular vascular basin. The term MA defines a group of patients with hemodynamically significant stenosis of several arterial basins at once, and, according to various studies, is diagnosed with a frequency from 13.5 to 94.8% of cases [2]. Multilevel lesion of the arteries of the lower limbs in atherosclerosis is a frequent phenomenon that involves both the iliac and the infrainguinal segment, especially in patients with critical limb ischemia (CLI). Such a lesion leads to a high risk of limb loss and often requires performing a voluminous and traumatic open surgery [3]. Open surgeries are fundamental in the treatment of chronic lower limb ischemia. The result of using this method is good primary patency in both the aorto-femoral and femoral-popliteal segments. However, it also has its drawbacks: high injury rate, blood loss, significant risk of cardiovascular and cerebrovascular complications in persons with MA [4].Endovascular interventions, as well as open surgeries, restore the patency of the arteries. The main advantages of these interventions are minimally invasiveness and the ability to restore the lumen of small-diameter arteries. But, at the same time, the use of endovascular intervention depends on the location, nature and extent of the lesion, and, perhaps, not in all treatment cases of a multilevel lesion, especially at occlusion and severe calcification [5]. Hybrid surgery combines the traditional angio-surgical approach and interventional techniques. The use of hybrid interventions in the treatment of occlusive processes in the arteries of the lower limbs has a number of advantages. In particular, this eliminates the need to perform large open surgical interventions, which helps to reduce complications, reduces the time of its implementation and traumatic consequences [6]. Thus, all the mentioned above indicates the need for an integrated approach to the treatment of patients with MA, individual consideration of clinical symptoms severity, determination of vascular lesion degree, detection and prevention of complications in the early and late postoperative periods. Aim of the study was to improve clinical treatment results of patients with critical limb ischemia with multifocal atherosclerosis.
2. Material and Methods
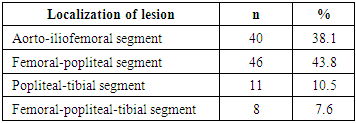
- The results of examination and treatment of 105 patients with CLI in combination with lesions of coronary and carotid arterial basins after USD and MSCT angiography treated in the department of vascular surgery of the multidisciplinary clinic of the Tashkent Medical Academy for the period from 2016 to 2020 were analyzed. There were 89 (84.7%) males and 16 (15.5%) females. The mean age of the patients amounted 64.67 ± 4.2 years.In all cases the cause of the disease was atherosclerosis. The criterion for selecting patients was the presence of CLI in combination with hemodynamically significant atherosclerotic lesions of the coronary and carotid arteries. All patients were performed staged interventions. Minimally invasiveness of interventions was a priority; before open large surgeries on the arteries of the lower limbs we initially tried to reconstruct the carotid and coronary basin. In addition to general clinical studies, the patients were examined for their neurological status; ultrasound methods of investigation, computed tomography and radiopaque angiography were performed. All this allowed to determine the level and length of the occlusive-stenotic process, the nature and morphology of the atherosclerotic plaque and to determine the appropriate treatment tactics. Determination of the degree of chronic limb ischemia in all patients was carried out in accordance with the classification of A.V. Pokrovsky (1979). At the same time, 64 (67.2%) patients had stage III ischemia, and 41 (32.8%) patients had stage IV.Multi-store lesions of the of the lower limbs vessels were revealed in all patients (Tab. 1).
|
|
3. Results
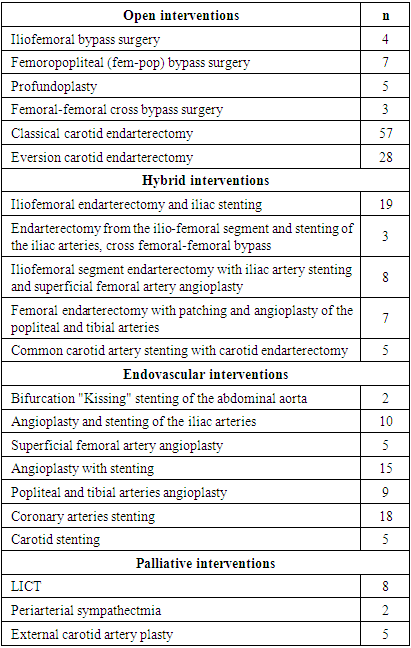
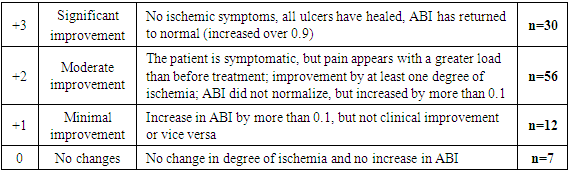
- Evaluation of the immediate results of patients’ surgical treatment was carried out according to the following criteria: preservation of the operated limb, patency of the reconstruction zone, regression of critical ischemia of the lower limbs.41 patients with CLI were performed endovascular intervention in the first stage. Among them, stenting of the coronary arteries was performed in 14 patients with ischemic heart disease, exertional angina pectoris of II-IV degree. Another 5 patients with hemadynamically significant stenoses were carried out stenting of the carotid arteries. Hybrid interventions were performed in 37 patients; the largest percentage of these interventions was performed in patients with lesions of the ilio-femoral segment. At extended occlusions of the iliac artery, stenting of the common iliac artery with open and looped endarterectomy from the common femoral and external iliac artery was performed in 19 cases. Three patients with bilateral occlusive-stenotic lesions of the iliac arteries underwent stenting and endarterectomy of the ilio-femoral segment, that is, the patency of one side of the ilio-femoral segment was restored and then the operation was supplemented with cross femoral-femoral bypass grafting. 5 patients with common carotid artery (CCA) occlusion underwent stenting of the proximal CCA, endarterectomy from the distal CCA of the ICA orifice with patching. A good hemodynamic effect was obtained in all cases.In 19 cases open reconstruction of the lower limb arteries was performed. At the same time, in 4 patients with coronary pathology presenting with unstable angina pectoris, the first stage was stenting of the coronary arteries. In other group of 6 patients with hemodynamically significant ICA stenosis with embolic plaque the first stage was carotid reconstruction, followed by reconstruction of the lower limb arteries on days 7-8. Important criteria for evaluating the efficiency of the performed surgery are the frequency of critical ischemia recurrence symptoms and the percentage of limb preservation. 10 patients underwent LICT in the presence of CLI, but when it was impossible to perform reconstructive interventions. The catheter was inserted according to the clinically developed method for LICT. The efficiency of therapy was determined based on the dynamics of improving blood flow in the lower limbs. At the same time, the initial ankle-brachial index (ABI) in these patients was 0.27 ± 0.1, on days 3-4 of LICT it increased to 0.51 ± 0.1 (t = 2.1. P <0.05). There was a significant increase in oxygen saturation in the tissues of the limb which indicates a significant improvement in the blood supply to the lower limbs. SpO2 (oxygen saturation in tissues) from the initial, which was 82.3 ± 2.4%, after treatment rose to 91.0 ± 3.4% (t = 2.07. p <0.05). It should be noted that a low ABI (ABI <0.4) index after treatment predicted a poor outcome. In the immediate postoperative period (3-4 days), 3 patients were performed high primary amputation of the limb due to CLI progression.Patients (n = 95) who underwent endovascular, hybrid and open reconstructions on the arteries of the lower limbs noted a significant improvement in clinical status associated with a decrease or disappearance of pain at rest, an increase in the distance without painful walking, a decrease in symptoms such as numbness, cold snap, and others.In the immediate postoperative period (up to 30 days), hemodynamic improvement was observed in almost all patients; on average, ABI in those patients increased from the initial 0.39 ± 0.2 to 0.79 ± 0.2 (t = 2.6. p <0.05). SpO2 from the baseline (83.1±1.9%) after treatment rose to 95.0±1.4% (t=2.2. p<0.05). When evaluating the immediate treatment results, the majority of patients showed a significant and moderate improvement (Tab. 3).
|
4. Discussion
- Analysis of surgical treatment immediate results showed that a high rate of clinical success when all three methods of direct revascularization of the peripheral bed of the lower limb arteries were used. In a number of cases, relapse of CLI symptoms could be stopped by using adequate conservative therapy. However, more often we had to perform high amputation. The frequency of amputations did not depend on the chosen technique. The cause of death of patients in the immediate postoperative period was mainly complications of the cardiovascular system. If we analyze the results separately, depending on the intervention performed, then the number of deaths was lower in the group of patients who underwent hybrid and endovascular surgery.Long-term treatment results of the examined patients were studied in 76 patients in the period from 6 to 36 months after the surgery. Disease progression (critical ischemia) was observed in 17 (22.3%) patients. At the same time, stroke developed in 4 (5.2%) patients, acute myocardial infarction in 4 (5.2%) patients, high amputations were performed in 12 (15.8%) patients. Mortality from stroke and myocardial infarction amounted 3.9% in general. Analyzing the results of our study, we came to the conclusion that the results of the studied methods of surgical treatment (open, closed and hybrid) CLI turned out to be very similar in their closest indicators. An obvious advantage of the open technique is the ability to determine the state of the vessel wall, the nature of the atherosclerotic plaque, and the assessment of retrograde blood flow. The endovascular technique is the least aggressive for the patient's body. However, the completeness of revascularization and the duration of the functioning of the reconstruction zone when using it are somewhat doubtful and limited. The hybrid technique, combining the advantages of "open" and "endovascular" technologies, simultaneously increases the duration and volume of surgical treatment, which in some cases can negatively affect the degree of operational risk. But the advantage of the method is the possibility of simultaneous restoration of the inflow and outflow paths.
5. Conclusions
- Taking into account the severity of the initial condition of patients with multifocal atherosclerotic lesion, the choice of the stage, volume and type of intervention should be individual. We prefer and recommend stage-by-stage interventions in the treatment of multifocal atherosclerosis.At the same time, the priority is a sparing approach to the choice of reconstructive interventions, namely, an increase in the proportion of hybrid and endovascular surgeries.Our experience shows that an adequate choice of the volume and stage of the intervention, as well as the widespread use of hybrid technologies hemodynamically and clinically gives the result no worse than open reconstructions and the number of complications and deaths is much less.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML