-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2021; 11(11): 788-790
doi:10.5923/j.ajmms.20211111.09
Received: Sep. 25, 2021; Accepted: Oct. 23, 2021; Published: Nov. 15, 2021

Clinical Features of Ankylosing Spondilitis in Postcovidal Period
N. M. Abdurakhmanova, Kh. S. Akhmedov
Tashkent Medical Academy, Tashkent, Uzbekistan
Correspondence to: N. M. Abdurakhmanova, Tashkent Medical Academy, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the study of the assessment of the clinical and functional features of the course of ankylosing spondylitis in patients who have undergone COVID-19. The patients were divided into two groups: the first group of patients with ankylosing spondylitis who had undergone COVID-19, the second group of patients with ankylosing spondylitis who did not undergo COVID-19. All patients underwent in-depth clinical, laboratory and radiological examinations as well as testing using various scales. The clinical course of ankylosing spondylitis in patients who had undergone COVID-19 was characterized by a more pronounced disease activity, a high intensity of pain syndrome and more pronounced impairments in functional activity.
Keywords: Ankylosing spondylitis, COVID-19, BASDAI
Cite this paper: N. M. Abdurakhmanova, Kh. S. Akhmedov, Clinical Features of Ankylosing Spondilitis in Postcovidal Period, American Journal of Medicine and Medical Sciences, Vol. 11 No. 11, 2021, pp. 788-790. doi: 10.5923/j.ajmms.20211111.09.
Article Outline
1. Introduction
- Coronavirus infection, which began to spread since December 2019, has now covered almost all countries of the world and the number of cases has already exceeded 219 million, and the number of deaths is over 4.55 million people in the world. (https://covid-stat.com). It is well known that COVID-19 not only has a severe effect on the condition of patients, causing the development of postcovid syndrome, but also affects the course of those somatic diseases that were observed in patients in the premorbid period [4,7]. The effect of COVID-19 on the osteoarticular system with the development of postcovid articular syndrome is also indicated in the works of Gasparotto et al. Scientists noted that even patients who did not suffer from joint diseases before Covid-19 in the postcovid period developed arthralgia and oligoarthritis. At the same time, such authors note that in patients who have previously suffered from ankylosing spondylitis (AS), an increase in pain syndrome, a feeling of morning stiffness in the joints, and restriction of movement in them are noted in the postcovid period [5,15].Purpose of the study: In an open, comparative randomized study, to study the clinical and functional features of the course of AS in patients who have undergone COVID-19.
2. Materials and Research Methods
- In the period from 2020-2021, 44 patients with a diagnosis of AS were hospitalized in the 3-city clinical hospital of the city of Tashkent (Uzbekistan). The patients were divided into two groups: Group I - 20 patients with AS who had undergone COVID-19 and Group II of 24 patients who had no history of AS infection with COVID-19. The average age of patients in the first group was 32 ± 4.1 years, with the duration of the disease from 1 to 8 years (the average duration of the disease was 5.5 years). And the average age of patients in the second group was 36.5 ± 5.2 years with the duration of the disease from 1 to 7 years (the average duration of the disease was 4.2 years). All patients underwent in-depth clinical, laboratory and X-ray examinations as well as testing using various scales. Functional impairments were assessed using the BASFI index, disease activity using the BASDAI and ASDAS scales, the MASES scale was used to assess the pain and swelling of enthesis, pain was assessed using a numerical rating scale (NRS), peripheral joint damage was assessed by the presence of pain and swelling in 44 joints. All patients underwent PCR tests for the presence of acute coronavirus infection, as well as IHLA tests for the presence of antibodies to COVID-19.
3. Results
- Clinical examination of patients in both comparison groups showed the presence of major complaints, such as morning stiffness, which was observed in 100% of patients in both groups; nocturnal back pain was noted by 95% of patients in group I and 76% of patients in group II; swelling of the joints in 82% of the I group, in 65% of the II group. Clinical examination of the patients revealed the presence of pain in the spine, which was assessed using the RSP and in group I was 8.5 ± 1.2 points and 5.9 ± 2.3 points in patients of group II. Examination of peripheral joints showed an average number of painful joints (PJ) of 16.9 ± 3.2 in group I and 8.6 ± 2.7 in group II, the number of swollen joints (NPV) 8.8 ± 2.1 in group I and 4.2 ± 1.7 in group II. group. As can be seen from the above data, severe pain syndrome was noted in both groups, which was the reason for patients seeking hospital treatment, but in the first group, against the background of COVID-19, the severity of pain syndrome was undoubtedly higher.
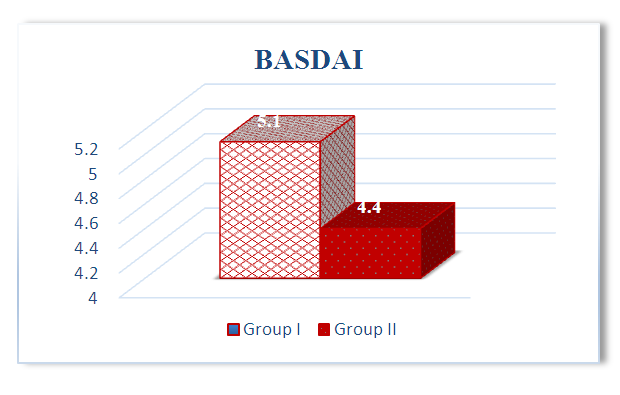 | Figure 1. AS activity according to the BASDAI scale in both groups |
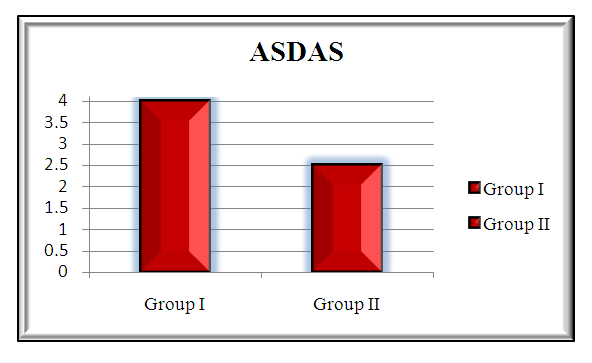 | Figure 2. Disease activity according to the ASDAS scale in both groups |
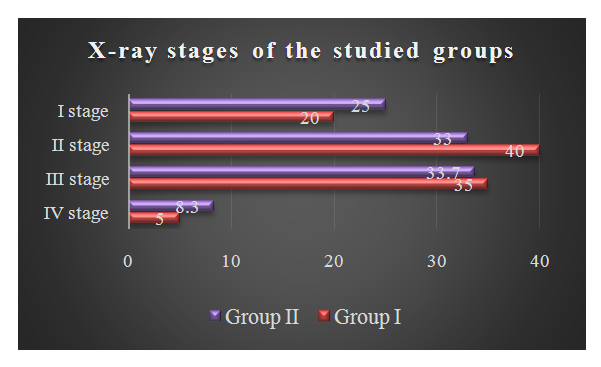 | Figure 3 |
4. Discussions
- Research has shown that COVID-19 infection has a global impact not only on target organs such as the lungs, brain and heart [1,7], but also has an effect on the osteoarticular system of the body [2,6,3]. At the same time, patients who had previously suffered from AS for many years were in a more vulnerable state in relation to patients who did not undergo COVID-19 [8,9,10]. It should be noted that the course of the disease in the postcovid period was aggravated by severe joint pain, decreased functional activity and high disease activity.
5. Conclusions
- 1. Covid infection aggravates the course of comorbid diseases, in particular AS, which apparently indicates the influence of this virus on the autoimmune mechanisms of the pathogenesis of damage to the osteoarticular system.2. The clinical course of AS in patients who have undergone COVID-19 is characterized by a more pronounced disease activity according to the BASDAI and ASDAS scales, a high intensity of pain syndrome according to a numerical rating scale - NRS and more pronounced functional disorders in the patient's daily activity according to the BASFI index.3. The results obtained must be taken into account when carrying out therapeutic and prophylactic measures for patients with AS proceeding against the background of the transferred COVID-19.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML