-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2025; 15(4): 880-882
doi:10.5923/j.ajmms.20251504.06
Received: Mar. 7, 2025; Accepted: Mar. 29, 2025; Published: Apr. 6, 2025

Impact of Lymphocyte Apoptosis on the Development of Psoriasis
Alyavi Saidnairkhon
PhD, Associate Professor, Department of Dermatovenerology and Cosmetology, Tashkent State Dental Institute, Tashkent, Uzbekistan
Correspondence to: Alyavi Saidnairkhon, PhD, Associate Professor, Department of Dermatovenerology and Cosmetology, Tashkent State Dental Institute, Tashkent, Uzbekistan.
| Email: |  |
Copyright © 2025 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The aim of the present study was to investigate the role of markers of activation and apoptosis of lymphocyte subpopulations in psoriasis. Methods: The content of the lymphocyte population in peripheral blood was determined using monoclonal antibodies to markers CD3, CD4, CD8, CD16, CD20, CD25, CD95 in 112 patients with psoriasis. Results: Different types of psoriasis exhibit diverse changes in the expression of markers associated with both positive and negative lymphocyte activation. Conclusions: Examining these activation markers helps identify various lymphocyte subpopulations and determine their role in the development and progression of psoriasis. These markers are linked to cellular cycle processes, including activation (CD25) and apoptosis (CD95).
Keywords: Psoriasis, Immunology, Apoptosis
Cite this paper: Alyavi Saidnairkhon, Impact of Lymphocyte Apoptosis on the Development of Psoriasis, American Journal of Medicine and Medical Sciences, Vol. 15 No. 4, 2025, pp. 880-882. doi: 10.5923/j.ajmms.20251504.06.
1. Introduction
- Psoriasis is a lifelong immune-mediated inflammatory skin disease characterised by accelerated proliferation of epidermocytes and impairment of their differentiation [1,2].The problem of psoriasis continues to be one of the most pressing issues in modern dermatology. WHO has emphasised the need for a better understanding of the global burden of psoriasis. In response to this need, the Global Atlas of Psoriasis was created to conduct comprehensive studies of the global prevalence and incidence of psoriasis [3,4]. The problem is also due to the unknown etiology and incomplete concepts of psoriasis pathogenesis [5,6,7]. The pathogenesis of psoriasis involves complex interactions between genetic, immunological and environmental factors, resulting in dysregulation of immune responses and excessive keratinocyte proliferation [8,9]. To date, there are a large number of publications in the literature indicating serious shifts in the immune status of psoriasis patients from both immunoregulatory and immune effector links, allowing us to consider this problem from the point of view of immunopathology [1,10]. Disorders of innate and adaptive cutaneous immune responses are responsible for the development and maintenance of psoriatic inflammation [11,12]. Recent studies have shown that epigenetic factors, including dysregulation of DNA methylation levels, abnormal histone modification, and microRNA expression, are involved in the development of psoriasis. The interaction between immune cells and cytokines is another critical factor in the pathogenesis of psoriasis [13].The process of apoptosis (also called programmed cell death) is a basic, ordered physiological process that leads to cell death without induction of inflammation. Under conditions of homeostasis, it fulfils a regulatory function. It leads to the death of mutated, autoreactive or damaged cells in the body. The key role of apoptosis is to maintain internal tissue balance [14]. Apoptosis plays a crucial role in several physiological functions such as cell deletion during embryonic development, balancing the number of cells in continuously renewing tissues, and the development of the immune system [15]. The study of apoptosis has proven to be very productive in understanding a number of crucial phenomena and processes, including immune homeostasis. Apoptosis is used to remove unwanted or potentially harmful cells from the body, such as autoreactive T lymphocytes, tumour cells and virus-infected cells. Apoptosis is important in the termination of immune reactions [16].It is considered that apoptosis is realized through activation of expression on the lymphocytes of the superficial CD95 receptor (Fas/APO-1) and its connection with ligand FASL. Classical specific receptors for apoptosis induction belong to the TNF-alpha receptor superfamily. They include Fas/CD95, TNF-alpha receptor type 1 (TNFR1), DR3/WS1-1, DR4/TRAIL-R1, DR5/TRAIL-R2, DR6, containing “the domain of death” in the cytoplasmatic site providing activation of the caspase cascades. Fas/CD95 expresses on the hepatocytes and circulating T-cells of memory. CD95 is not induced on the “testing” T-cells CD45RA+ and is poorly induced on the B-lymphocytes. At cell activation CD95 expresses predominantly on the neutrophils, hepatocytes, T-lymphocytes CD4+, that characterizes their high sensitivity to FASL-induced apoptosis. FASL expresses actively on activated T-lymphocytes and, cooperating (as membrane-associated or soluble protein) with Fas/Cd95, it becomes the basic mechanism of apoptosis of the cell-targets in various diseases [17,18].The elucidation of the mechanisms of lymphocyte apoptosis disorders in psoriasis allows not only deeper understanding of pathogenesis of this dermatosis, but also planning new ways and approaches to immune correcting therapy.
2. Materials and Methods
- The study included 112 patients with psoriasis. From heparinized peripheral blood of the patients on the 3% gelatin there were isolated intact lymphocytes. Blood samples obtaining was carried out before and after ending of the treatment.The content of the lymphocyte population in the peripheral blood was determined with the help of monoclonal antibodies to markers CD3 (T-lymphocytes), CD4 (T-helpers/inducers), CD8 (T-suppressors/cytotoxic), CD16 (natural killers), CD20 (B-lymphocytes), CD25 (lymphocytes with receptor to IL-2), CD95 (lymphocytes with receptor to apoptosis) with indirect plaque assay. The principle of a method consists of attachment of human erythrocytes, sensibilized with monoclonal antibodies LT3, LT20, LT4, LT8, LT16, LT25, LT95, and LT HLA-DR on the surface of lymphocytes.The group of comparison (n=54) included healthy people of the same age, as the studied patients.
3. Results and Discussion
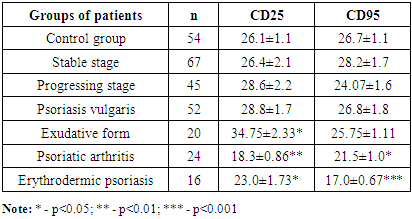
- Study of activation markers enables defining various lymphocyte subpopulations, establishing their role in development and progress of psoriasis, as they characterize the processes of activation (CD25) and apoptosis (CD95) connected with the cellular cycle.
|
4. Conclusions
- Thus, at the various forms of psoriasis there are observed multidirectional changes of the expression of markers of lymphocyte positive and negative activation. Psoriasis induces changes of qualitative and functional parameters of cellular immunity that results in proliferation and predifferentiation of lymphocytes. Study of activation markers allows identifying the different lymphocyte subpopulations, establishing their role in development and progressing of psoriasis. At activation of T lymphocytes the cytokine IL-2 and its receptors play a key role in development, maturing and regulation of immune response supporting proliferation of activated T and B lymphocytes.The study of the role of markers of activation and apoptosis in psoriasis seems to be significant because the results received will promote understanding of the complex mechanisms of the pathogenesis of disease and improvement of the methods of diagnosis and therapy.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML