Fazilova Makhshura Olimjanovna
Samarkand Branch of the Scientific Research Institute Obstetrics and Gynecology Mom and Child, Samarkand, Uzbekistan
Correspondence to: Fazilova Makhshura Olimjanovna, Samarkand Branch of the Scientific Research Institute Obstetrics and Gynecology Mom and Child, Samarkand, Uzbekistan.
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Abstract
The endometrium plays a key role in the reproductive function of a woman, as it is the site of implantation and development of the embryo [1,3,4]. A missed miscarriages pregnancy is often associated with changes in the endometrium, which can affect the possibility of conception and the normal development of pregnancy [2,5].
Keywords:
Missed miscarriages, Endometrium, Pulsation index
Cite this paper: Fazilova Makhshura Olimjanovna, Endometrial Condition in Women with a History of Missed Miscarriages, American Journal of Medicine and Medical Sciences, Vol. 14 No. 11, 2024, pp. 2723-2725. doi: 10.5923/j.ajmms.20241411.09.
1. Introduction
We analyzed the endometrium in women with a history of missed miscarriages to identify structural and functional changes that may contribute to an unfavorable pregnancy outcome, as well as to find out the possibility of using appropriate therapeutic measures. It is assumed that the study will identify structural and functional changes in the endometrium in women with missed miscarriages, as well as identify possible mechanisms of their impact on reproductive function. It is expected that the data obtained will help to better understand the pathogenesis of missed miscarriages and develop effective strategies for the prevention and treatment of this condition.Purpose: Study of the endometrium in women with a history missed miscarriage in order to identify pathological changes and possible mechanisms of their impact on reproductive function.
2. Research Methods
To study the state of the endometrium in women with a history of missed miscarriage, an ultrasound examination of the pelvic organs was performed.
3. Results and Discussion
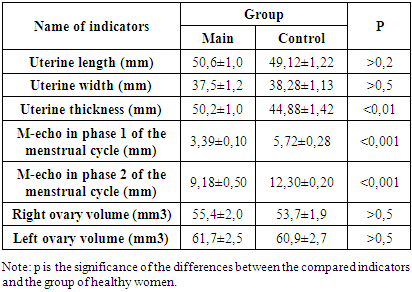
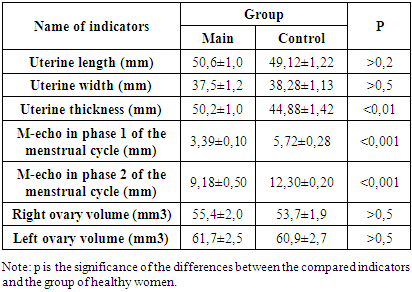
When examining the pelvic organs in the 1st phase of the menstrual cycle, the mean value of the length, thickness and width of the uterus in women with a missed miscarriage in anamnesis was 50.6±1.0 mm, 37.5±1.2 mm and 50.2±1.0 mm, respectively. In the control group, these values were 49.12±1.22 mm, 38.28±1.13 mm and 44.88±1.42 mm, respectively. No statistically significant differences between the groups were found (p>0.05 for all indicators) (Table 1).Таble 1. Uterine size in the examined groups of women
 |
| |
|
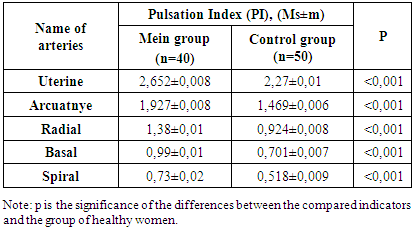
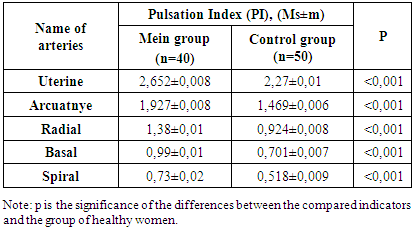
The mean M-echo in phase 1 of the menstrual cycle in women with a history of missed miscarriage was significantly lower: 3.39±0.10 compared to the control group, where it was 5.72±0.28 (χ2=36.5; p<0.001). Heterogeneous endometrial structure with hyperechogenic and punctate inclusions was revealed in 3.8% of women in the study group, while in the control group, the endometrial structure was homogeneous in all 100% of women.During the examination in the 2nd phase of the menstrual cycle, 38.8% of women in the study group had endometrial thickness less than 8 mm, and in 23.8% – more than 8 mm. The mean value of M-echo in the second phase of the menstrual cycle was significantly lower in women with a missed miscarriage in anamnesis: 9.18±2.30 compared to the control group, where it was 12.30±0.20 (χ2=59.4; p<0.001).Ultrasound assessment of ovarian volume revealed that the volume of the right ovary averaged 55.4±20.0 mm3, the left ovary was 61.7±3.5 mm3 in women of the study group, and did not differ statistically significantly from the control group. However, in women with non-developing pregnancies, cases of reduced ovarian reserve and small cysts have been revealed.The results of ultrasound examination indicate the presence of structural and functional changes in the endometrium in women with a history of missed miscarriage. These changes can have an impact on the possibility of conception and the development of pregnancy, which highlights the importance of further research and the development of clinical strategies to optimize women's reproductive health.The next objective of our study was to assess the features of blood flow in the uterine vessels of the studied women using Doppler to identify possible disorders that contribute to the development of NB. We evaluated the pulsatile index (PI), systolodiastolic ratio (LMS) and resistance index (IR) in the uterine, arcuate, radial, basal and spiral arteries in women with a history of missed miscarriage. The study was based on the analysis of data from Doppler studies of uterine vessels in 80 women. Of these, 40 women had a history of non-developing pregnancies (the study group) and the other 40 women (control group) had no history of obstetric abnormalities. As a result, it was found that the values of the pulsation index in the study group (n=40) and in the control group (n=40) differed. In the uterine arteries, the pulsation index in the study group was 2.652±0.008, while in the control group it was 2.27±0.01 (p≤0.05). In the arcuate arteries, the values were 1.927±0.008 and 1.469±0.006, respectively (p≤0.05). In the radial arteries, the pulsation index in the study group was 1.38±0.01, in the control group — 0.924±0.008 (p≤0.05). In the basal arteries, the indicators were 0.99±0.01 and 0.701±0.007, respectively. Finally, in the spiral arteries, the PI values were 0.73±0.02 in the study group and 0.518±0.009 in the control group (p≤0.05).These findings highlight differences in vascular resistance and blood flow between the study groups, which may be important for understanding physiological and possibly pathological changes in uterine blood supply (Table 2).Таble 2. Indicators of blood flow of uterine vessels (pulsation index) in the studied women
 |
| |
|
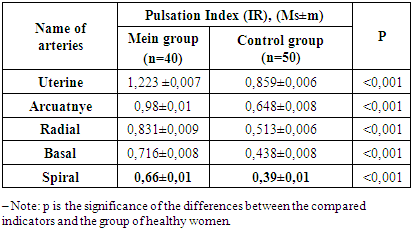
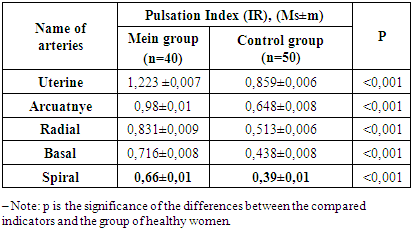
Analyzing Table 2, it should be noted that the confidence intervals for the resistance index (IR) in both groups indicate a clear separation between the study and control groups for all types of arteries. This indicates significant differences in IR values between groups. Uterine arteries: mean IR values differ significantly between the study (1.223) and control (0.859) groups. Confidence intervals do not overlap, which confirms the significance of the differences (p≤0.05). Artery arteries: Similarly, mean IR values differ between the baseline (0.98) and control (0.648) groups, with nonoverlapping confidence intervals (p≤0.05). Radial arteries: mean IR values in the study (0.831) and control (0.513) groups also differ significantly (p≤0.05). Basal arteries: there is a significant difference (p≤0.05) between the mean IR values in the study (0.716) and control (0.438) groups. Spiral arteries: differences between the main (0.66) and control (0.39) group.These results indicate significant differences in the index of uterine vascular resistance between the studied groups of women for all types of arteries (Table 3).Таble 3. Indicators of uterine vascular blood flow (resistance index) in the studied women
 |
| |
|
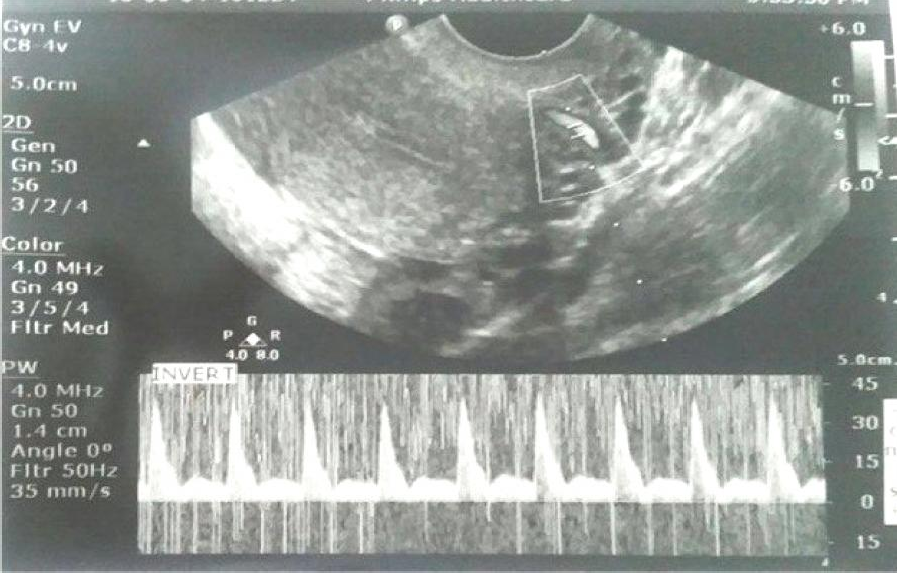
As an illustration of this section of the work, we give a clinical example: Patient N., 22 years old, has a history of 2 non-developing pregnancies. The figure shows a pulsation index of 2.61, i.e. there is an increase in the peripheral resistance of the uterine vessels. (Fig. 1). The pulsation index, a key parameter used to assess vascular resistance in the uterine arteries, is 2.61 in this image. 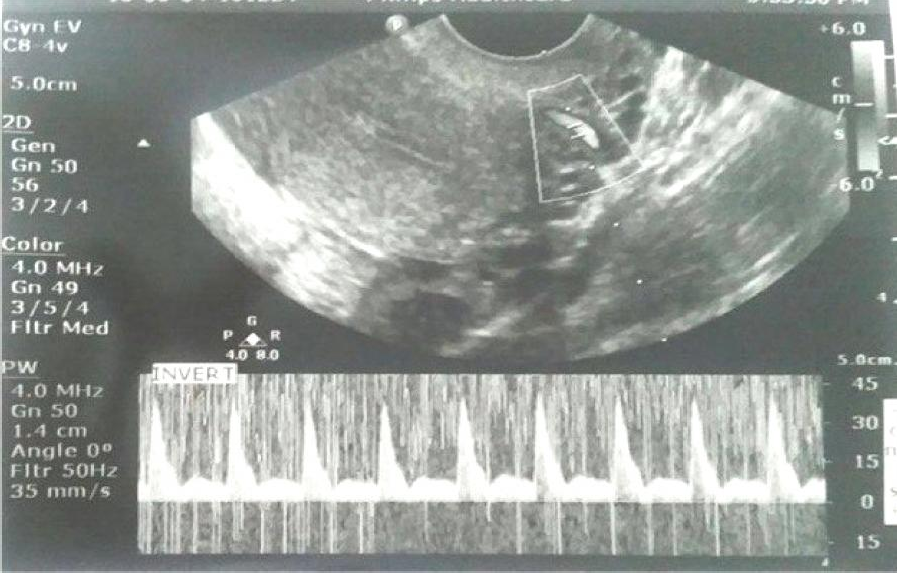 | Figure 1. Doppler sonography of the uterine vessels (pulsation index of the uterine artery). Patient N., born in 2002, card number No 57, with a history of 2 non-developing pregnancies (PI = 2.61) |
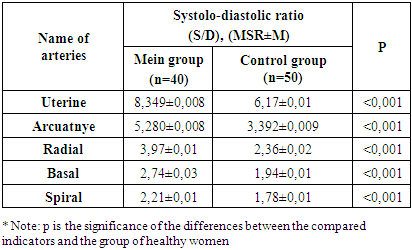
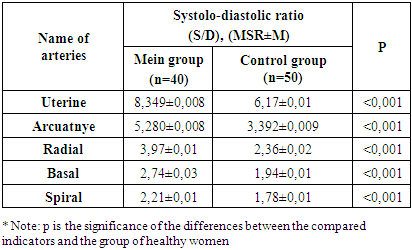
This value can be used to analyze blood flow and vascular permeability in the context of the patient's reproductive health history, including previous non-developing pregnancies.Differences in the systolo-diastolic ratio (S/D) between the study and control groups were also significant. The S/D ratio is an important indicator in assessing vascular blood flow, and changes in it may reflect different states of tissue blood supply, including changes in vascular resistance and perfusion (Table 4). Таble 4. Doppler examination of uterine vessels (systolo-diastolic relationship) in women of the study groups
 |
| |
|
The study analyzed five types of arteries: uterine, arcuate, radial, basal and spiral. The measurement results are presented as the mean value (Msp) and the standard error of the mean (m). The uterine arteries show a mean S/D ratio of 8.349±0.008 in the study group compared to 6.17±0.01 in the control group, indicating an increased ratio in the study group (p≤0.05). The arteries show a mean S/D ratio of 5.280±0.008 in the study group versus 3.392±0.009 in the control group, also reflecting higher values in the study group (p≤0.05). Radial arteries have a mean S/D ratio of 3.97±0.01 in the study group compared to 2.36±0.02 in the control group, confirming a trend towards higher values in the study group (p≤0.05). The basal arteries are represented with an average S/D ratio of 2.74±0.03 in the study group and 1.94±0.01 in the control group, which also indicates an increase in this indicator in the study group (p≤0.05). The spiral arteries show a mean S/D ratio of 2.21±0.01 in the study group versus 1.78±0.01 in the control group, showing a similar trend (p≤0.05).The results of the study highlight statistically significant differences in the systolo-diastolic relationship between the study and control groups for all arterial types studied. Higher values of the S/D ratio in the study group reflect differences in the hemodynamic characteristics of uterine vessels, which is important for understanding pathophysiological processes in the uterus and can be used to further study the influence of various factors on the state of the uterine vascular system.The study showed that uterine vascular Doppler detects blood flow disorders in women with a history of non-developing pregnancies, which in turn contributes to the development of individualized approaches to preventive and therapeutic measures to prevent the recurrence of this complication in the future.
References
| [1] | Arintseva A. A., Timoshkina A. S., Smirnova T. I. Missed miscarriage: causes and consequences. – 2021. – №. 2. – P. 46-48. |
| [2] | Clinical guidelines. Obstetrics and Gynecology. – 4th edition, revised and supplemented / Edited by V.N. Serov, G.T. Sukhikh. Moscow: GEOTAR-Media, 2014. – 1024 p. |
| [3] | Missed miscarriage: Guidelines of MARS (Interdisciplinary Association of Reproductive Medicine Specialists). Author- compiler V.E. Radzinsky et al. - Moscow: Editorial Board of the journal Status Praesens, 2015. |
| [4] | Fazilova M., Sultanov S. Assessment of the State of the Coagulation Link of Hemostasis in Women Who Terminated Non-Developing Early Pregnancy with Medication // Science and innovation. – 2022. – Т. 1. – №. D7. – С. 259-263. |
| [5] | Olimjanovna, F. M. "Glycadelin in Obstetrical Practice: Past, Present." Practice. J Regen Biol Med 4, no. 3 (2022): 1-8. |


 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML