-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(10): 1039-1043
doi:10.5923/j.ajmms.20221210.06
Received: Sep. 22, 2022; Accepted: Oct. 8, 2022; Published: Oct. 14, 2022

Application of Reflexotherapy and Traditional Oriental Gymnastics at the Outpatient Stage of Rehabilitation of Patients after COVID-19 Complicated by Psychoneurological Disorders
Muminova N. Kh. , Visogortseva O. N.
Tashkent Medical Academy, Tashkent, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The article is devoted to the development of individual rehabilitation programs for patients who have undergone COVID-19, complicated by neuropsychiatric disorders, using the methods of exercise therapy, physiotherapy and traditional oriental medicine at the outpatient stage.
Keywords: COVID-19, Neuropsychiatric disorders, Medical rehabilitation, Physiotherapy, Reflexology, Traditional oriental gymnastics
Cite this paper: Muminova N. Kh. , Visogortseva O. N. , Application of Reflexotherapy and Traditional Oriental Gymnastics at the Outpatient Stage of Rehabilitation of Patients after COVID-19 Complicated by Psychoneurological Disorders, American Journal of Medicine and Medical Sciences, Vol. 12 No. 10, 2022, pp. 1039-1043. doi: 10.5923/j.ajmms.20221210.06.
1. Introduction
- Initially, COVID-19 was assumed to be an acute infection with complete resolution of mild to moderate forms within 2-3 weeks. However, over time, there is increasing evidence that clinical manifestations can persist for more than 6 months [2,19,21,23]. In September 2020, the International Classification of Diseases, 10th revision, introduced a separate code to describe post-COVID-19 syndrome: "U09.9 - condition after COVID-19" [6,20]. It turned out that most patients who had a new coronavirus infection needed medical rehabilitation measures.Currently, there is a situation in the world in which there is insufficient
 information on medical̆ rehabilitation care for patients with COVID-19 because the disease is new. Given the unusual nature of the pandemic situation itself and the specific pathogenesis of the disease caused by SARS-CoV-2, the formulaic use of conventional methods of rehabilitation after respiratory illness may be unsafe or ineffective [8]. Persistent or re-emerging symptoms, and COVID-19-related functional impairment in ≥50% of cases, according to questionnaires and analysis of disease outcomes in hospitals and clinics, negatively affect the quality of life, mobility, and independence of patients seeking medical care [14-18]. Development of individual programs of medical rehabilitation (MR) of patients with the post-COVID-19 syndrome with the use of methods of therapeutic physical training, physical therapy, reflexotherapy and other non-medicamental methods at the outpatient stage remains a topical problem. At the same time, non-drug methods of MR are aimed at the activation of adaptive reserves of an organism taking into account peculiarities of pathogenesis and clinical manifestations of post-COVID-19.Medical rehabilitation (MR) of patients with the post-COVID-19 syndrome at the outpatient stage has the following objectives: restoration of cardiorespiratory system functions, alignment of arousal and inhibition processes in the central nervous system (CNS), improvement of psycho-emotional tone and sleep quality, combating muscle pain syndrome, restoration of muscle strength, increasing tolerance to physical exertion [3,5,9,13].Following the goal set and objectives, the rehabilitation program includes therapeutic exercise (TE) and physical factors with sedative, psychotonic, analgesic, and trophostimulating effects [4,7,10,11,12].A promising and relevant direction is the possibility of broader use of methods of traditional oriental medicine: reflexology, manual therapy, and traditional gymnastics (yoga, tai chi, Qigong therapy) [24]. At the present stage, an integrated approach using both empirical provisions of ancient oriental theories, methods of traditional Chinese medicine, and neurophysiological concepts of modern acupuncture, using up-to-date modifications of exposure to acupuncture points, is the most optimal [22,24].The study aimed to develop a comprehensive rehabilitation program for patients with COVID-19 complicated by neuropsychiatric disorders at the outpatient stage using methods of traditional oriental medicine and evaluate its effectiveness.
information on medical̆ rehabilitation care for patients with COVID-19 because the disease is new. Given the unusual nature of the pandemic situation itself and the specific pathogenesis of the disease caused by SARS-CoV-2, the formulaic use of conventional methods of rehabilitation after respiratory illness may be unsafe or ineffective [8]. Persistent or re-emerging symptoms, and COVID-19-related functional impairment in ≥50% of cases, according to questionnaires and analysis of disease outcomes in hospitals and clinics, negatively affect the quality of life, mobility, and independence of patients seeking medical care [14-18]. Development of individual programs of medical rehabilitation (MR) of patients with the post-COVID-19 syndrome with the use of methods of therapeutic physical training, physical therapy, reflexotherapy and other non-medicamental methods at the outpatient stage remains a topical problem. At the same time, non-drug methods of MR are aimed at the activation of adaptive reserves of an organism taking into account peculiarities of pathogenesis and clinical manifestations of post-COVID-19.Medical rehabilitation (MR) of patients with the post-COVID-19 syndrome at the outpatient stage has the following objectives: restoration of cardiorespiratory system functions, alignment of arousal and inhibition processes in the central nervous system (CNS), improvement of psycho-emotional tone and sleep quality, combating muscle pain syndrome, restoration of muscle strength, increasing tolerance to physical exertion [3,5,9,13].Following the goal set and objectives, the rehabilitation program includes therapeutic exercise (TE) and physical factors with sedative, psychotonic, analgesic, and trophostimulating effects [4,7,10,11,12].A promising and relevant direction is the possibility of broader use of methods of traditional oriental medicine: reflexology, manual therapy, and traditional gymnastics (yoga, tai chi, Qigong therapy) [24]. At the present stage, an integrated approach using both empirical provisions of ancient oriental theories, methods of traditional Chinese medicine, and neurophysiological concepts of modern acupuncture, using up-to-date modifications of exposure to acupuncture points, is the most optimal [22,24].The study aimed to develop a comprehensive rehabilitation program for patients with COVID-19 complicated by neuropsychiatric disorders at the outpatient stage using methods of traditional oriental medicine and evaluate its effectiveness.2. Research Methods and Materials
- The study was conducted in the Center for Oriental Medicine at the Korean International Cooperation Agency (KOICA) in Uzbekistan and the Republican Clinical Hospital (RCH) No.2, Health Center No.2 in Tashkent. We observed 166 patients with coronavirus infection who had signs of nervous system damage. The patients underwent outpatient rehabilitation in the period 2020-2022, 4 weeks after the end of treatment for the main disease.The study was characterised as an open, prospective observational research. The study design was meant to include men and women aged 30 to 65 years who were diagnosed with an anxiety disorder (AD) with an anxiety score of at least 17 on the Hamilton Scale. This scale allows the detection of not only affective but also psychosomatic disorders [1]. All patients signed informed consent to participate in the study.The multidisciplinary rehabilitation team included a neurologist, a rehabilitologist, a reflexologist, an instructor of physical therapy, a masseur, and a nurse from the physical therapy department.Depending on the medical rehabilitation program, the patients were divided into 4 groups, comparable with each other in terms of age and sex characteristics and clinical and functional state of the body.Group I (n=38) consisted of patients who exercised independently at home every day for 10-15 minutes of morning exercises and 30-40 minutes of evening walks.Group II (n=40) patients received massage and physical therapy procedures (magnetic therapy of the collar zone or pain area) for 10 days.In Group III (n=42), the rehabilitation program included reflexotherapy procedures.Group IV (n=46) included patients whose rehabilitation program included reflexotherapy procedures and physical therapy sessions with the elements of traditional oriental gymnastics (qigong, yoga with meditation elements). Magnetotherapy procedures were conducted on the apparatus "Polyus-1" with the assistance of round inductors or solenoids; the intensity of the alternating magnetic field was 30 mT, 15 minutes per field, after the course of 10 procedures was made according to the classical method.Reflexotherapy was carried out by acupuncture therapy (Zhen, ART); it is a method of treating diseases by applying acupuncture needles to biologically active points. Several needle insertion techniques were carried out, which provided excitatory, inhibitory, and harmonizing influence techniques, depending on the syndromic acupuncture and clinical diagnoses. The number of needles inserted varied from 5 to 15. The duration of the session ranged from 15 to 60 minutes. The course of treatment was from 10 to 20 sessions.In the IV observation group, in addition to ART, the patients were engaged in therapeutic gymnastics according to the developed method with the inclusion of elements of traditional oriental gymnastics Qigong and yoga. A sample set of exercises is given in Appendix 1.The patients underwent a comprehensive examination before the MR program, at the end of the course of procedures, as well as after 1, 3 and 6 months from the beginning of the program. The criteria for the effectiveness of the rehabilitation measures were:- neurological status;- visual analogue pain scale (VAS);- assessment of SpO2 at rest and during physical activity,- evaluation of physical activity tolerance according to the Borg Scale,- assessment of dyspnea on MRC scale (dyspnea),- assessment of muscle strength on the MRC scale (muscles),- assessment of the intensity of anxiety and depression on the Hospital Anxiety and Depression Scale (HADS);- assessment of quality of life according to the results of the European Quality of Life Questionnaire EQ-5 in dynamics.Statistical data processing was performed using Excel and SPSS application programs. Descriptive statistics criteria w used to characterize the data obtained: arithmetic mean, standard deviation. We assessed the differences in the average indices for the 2 groups using Student's test. The difference was considered statistically significant if p < 0.05.
3. Results
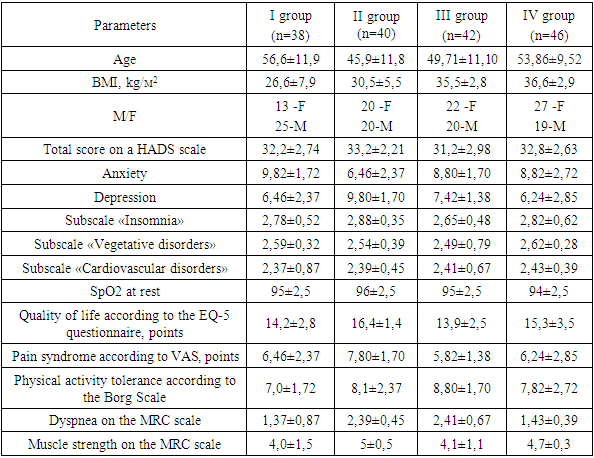
- When patients were evaluated at the time of referral to an outpatient health centre, 31% (51 patients) had 1-2 symptoms, and 59% (115 patients) had three or more symptoms. Quality of life deterioration was observed in 45.7% (76 people) of patients. The most frequent symptoms seen one month after COVID-19 infection included: fatigue (65%), insomnia (24%), anxiety and depression (26%), hair loss (23%), anosmia (9%), joint pain (12%), palpitations (11%), decreased appetite (9%), taste disorder (8%), dizziness (5%), diarrhoea and vomiting (3%), chest pain or tightness (7%), sore throat (3%), skin rash (2%), headache (4%), myalgia (4%). The clinical and functional characteristics of patients on admission for MR are shown in Table 1.
|
|
4. Conclusions
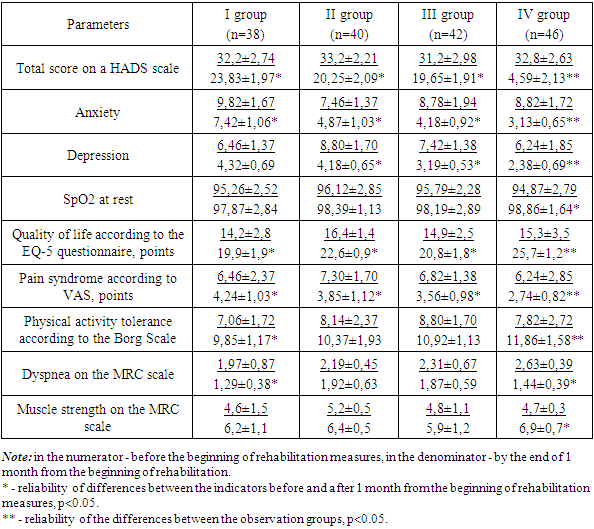
- Neurotropism of SARS-CoV-2 coronavirus leads to neurological disorders of varying severity, which can persist for a long time in the post-COVID-19 period. High attendance for anxiety disorders, sleep disorders, pain syndrome, persisting dyspnea and asthenia, their significant severity long after the end of the acute period of the disease, and reduced ability to work require special rehabilitation measures.The application of physical factors and modified complexes of physical exercises contributes to the alignment of excitation and inhibition processes in the CNS, as well as the development of psychotonic, analgesic and trophostimulating effects.The program that included the use of reflexotherapy and a complex of physical exercises with elements of traditional oriental gymnastics (qigong, yoga with meditation) proved to be the most effective. This is evident from a greater increase in PC (physical capability) indices, better dynamics of pain reduction, dyspnea, increase in muscle strength indicators, quality of life and psycho-emotional status. Patients without additional training and ART showed the smallest increase in the indicated indices.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML