-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Medicine and Medical Sciences
p-ISSN: 2165-901X e-ISSN: 2165-9036
2022; 12(10): 1034-1038
doi:10.5923/j.ajmms.20221210.05
Received: Sep. 8, 2022; Accepted: Oct. 2, 2022; Published: Oct. 14, 2022

Clinical-Immunological Methods of Clinical-Immunological Research of Atopic Dermatitis in Children Permanently Residing in the Area of Oil Refining Enterprises
Achilova Donokhon Nutfullayevna , Khushvaktova Madina Farkhodovna
Bukhara State Medical Institute Named after Abu Ali Ibn Sina, Uzbekistan
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

To date, a number of factors have been identified that aggravate the course of atopic dermatitis - food sensitivity, contact with pets, psychological discomfort and emotional stress, a history of intrauterine infections, skin colonization with Staphylococcus aureus. But the information received is not always reliable from the point of view of evidence-based medicine. However, an integrated one has not been developed; systems for predicting the nature of the disease in children. Accession of a secondary skin infection adversely affects the severity of the disease and the quality of life of patients; the frequency of complex forms of atopic dermatitis in children is on average 25-34%.
Keywords: Atopic dermatitis, Сhildren's age, Young child, Inflammation, Bifalak-Zinkum+S+D3, Prevention, Treatment
Cite this paper: Achilova Donokhon Nutfullayevna , Khushvaktova Madina Farkhodovna , Clinical-Immunological Methods of Clinical-Immunological Research of Atopic Dermatitis in Children Permanently Residing in the Area of Oil Refining Enterprises, American Journal of Medicine and Medical Sciences, Vol. 12 No. 10, 2022, pp. 1034-1038. doi: 10.5923/j.ajmms.20221210.05.
Article Outline
1. Introduction
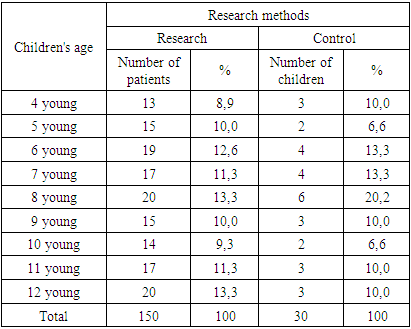
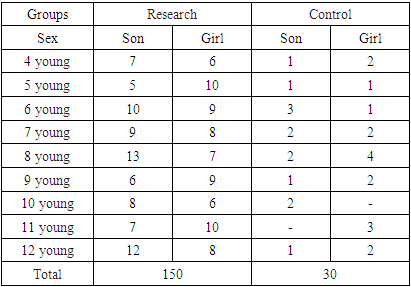
- Children from 4 to 12 years of age living in the territory of the Bukhara Oil Refinery, Karavulbazar District, Bukhara Region, were examined. During the research, according to the tasks, 180 children were under our control, 150 of them were children with atopic dermatitis and 30 were healthy children (Table 1).
|
|
|
2. Methods of General Examination of Children with Atopic Dermatitis
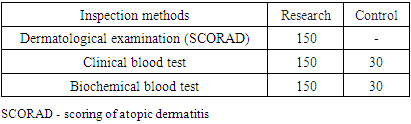
- Dermatologic Examination (SCORAD)The severity of atopic dermatitis was evaluated using the SCORAD scale (scoring of atopic dermatitis) during the study. When evaluating the SCORAD index, the objective characteristics of rashes, as well as the severity of itching and sleep disturbances are taken into account. Objective signs (erythema, edema / papules, crusting, excoriations / lichenification, pruritus, dry skin) were scored on a 4-point scale.The maximum spread of rashes is 100 points with common skin areas. Each subjective symptom was evaluated on a scale from 0 to 10 points. The maximum score for subjective marks is 20.The formula for calculating the SCORAD index:SCORAD=A/5+7B/2+Cwhere A is the area of skin damage,V is the sum of strength values of clinical signs of atopic dermatitis,C is the sum of the scores of subjective complaints on the visual analogue scale. The maximum value of the SCORAD index - 103 - is considered a severe form of atopic dermatitis.
3. Clinical Blood Test
- During the study, blood tests were performed at the same time under the same conditions, before meals. Blood for research was taken in a certain order: EChT, determination of hemoglobin, then - counting of leukocytes and erythrocytes.
4. Biochemical Examination of Blood
- Biochemical examination of blood during the study includes the study of the following indicators: total protein, albumin, total bilirubin, transaminases (AlAt and ACT), alkaline phosphatase, glucose, antistreptolysin-O, potassium magnesium, sodium, calcium. It was carried out on the "Konelab 30i" autoanalyzer (firmy Thermoelectron, Switzerland).
5. Clinical and Pharmacological Recommendations in Children with Atopic Dermatitis
- During the study, we divided the patient children into 3 parallel groups for all research groups. This was the main purpose of this study. Comparison of the effectiveness of basic therapy and therapy in combination with drugs that help to remove xenobiotics from the body of sick children.The therapy carried out in groups of sick children is the traditional therapy for the acute period of atopic dermatitis in groups 1 and 3: hypoallergenic diet, antihistamines, sedatives (pustirnik, valerian), local treatment (fucorcin solution, topical glucocorticosteroids). The duration of treatment in the acute period is on average 5-7 days. For three weeks, during this period, with the elimination of acute inflammatory events on the skin, the following were used: elimination measures to eliminate the causative allergens; antihistamines; external therapy (topical glucocorticosteroids of weak activity, the first 3-5 days, calcineurin inhibitors, then switching to active ointments or pastes). The duration of treatment during the period of agitation was from 10 to 20 days. In addition to the above therapy, all patient children in group 2 (n=64) are started. During the acute period, sorbents and antidotes are given.Bifalak-Zinkum+S+D3.,0.5g preparation was used as a sorbent.Bifalak-Zinkum+S+D3., consists of 0.5g of polyphane and lactulose. Polyphane is a complex natural organic compound, a product processed by hydrolysis, an enterosorbent. Due to its large surface area and developed system, it has a high resorption capacity and is able to remove toxins and pathogenic microflora from the body. Lactulose is a carbohydrate consisting of a galactose residue and a fructose residue. Lactulose is an ideal environment for the development of bifidobacteria and lactobacteria in the large intestine, it helps to normalize the metabolism of proteins, fats and carbohydrates, promotes the proper absorption of vitamins, macro- and microelements, and also stimulates non-specific immunity. Lactulose is not absorbed by the human body. Bifalak-Zinkum+S+D3.,0.5g has a dual effect: sorbent and probiotic. The choice of this drug is influenced by the fact that sorbents have a rough surface and, when ingested, often irritate the mucous membrane of the gastrointestinal tract and cause irritation and vomiting in children with pharyngeal reflexes. The form of Bifalak-Zinkum+S+D3.,0.5g provides the most convenient way of taking this sorbent.Bifalak-Zinkum+S+D3.,0.5g is taken 1-2 tablets 3 times a day for 2 weeks. The daily dose depends on the age and weight of patients:Children from 4 to 6 years old - 1 tablet, 3 times a day,Children from 7 to 12 years old, 3 tablet 3 times a day.Unitiol was selected as an antidote to remove heavy metal ions. The drug binds to thiol poisons and forms non-toxic compounds that can be excreted from the body through the kidneys. Blocked by heavy metals, sulfur-containing groups in enzymes and other biologically active proteins and cofactors are released, and this is the enzyme system that leads to the restoration of their activity. Unitiol is known to have activity against arsenic, mercury, chromium, bismuth, cadmium and other metal ions known as thiol poisons. Unitiol is also used in the treatment of diseases caused by an overdose of cardiac glycosides, and in the complex treatment of chronic alcoholism. Unitiol is administered orally to children with atopic dermatitis at the rate of 1 ml of a 5% solution per 10 kg of body weight per day for 10 days. The use of the drug is divided into three doses - taken 30 minutes before meals, with a small amount of water.The statistical analysis of the research results was carried out after selecting the central characteristics of the studied quantitative data and extracting their distribution form. We calculated the mean, standard deviation, and standard error. The normality criterion was tested using the one-sample Kolmogorov-Smirnov method. Student's t-test was used for parametric tests. As non-parametric methods, we chose Fisher's exact test. Using Pearson's correlation coefficient, the strongest relationship between the severity of microlosis and the SCORAD index was found in the group of children living near, Karavulbazar district, Bukhara region (correlation coefficient r=0.8 at the significance level of r<0.05).Information about sick children was entered into a special coder, which included clinical, laboratory data, dynamics of the SCORAD index, and indicators of micronutrient status. All calculations were made using the STAYISTICA mathematical package.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML