-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Statistics and Applications
p-ISSN: 2168-5193 e-ISSN: 2168-5215
2015; 5(6A): 6-14
doi:10.5923/s.statistics.201501.02

Predictive Study of Psychological Variables Impact in Family Caregivers of Patients with Alzheimer
Manuela Leite , Vera Almeida , Maria Prazeres Gonçalves
CESPU, Institute for Research and Advanced Training in Health Sciences and Technologies, Gandra, Portugal
Correspondence to: Manuela Leite , CESPU, Institute for Research and Advanced Training in Health Sciences and Technologies, Gandra, Portugal.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study aimed to identify the predictor variables of: (1) Evaluation of Care; (2) Depression; (3) Anxiety; and (4) Stress - Impact variables in care of relatives with Alzheimer's dementia. The sample consists of 86 caregivers, 49 spouse caregivers and 37 children caregivers. Both groups are primary caregivers and care mostly for more than 3 years, 12 to 24 hours a day. It was used a Socio-demographic and clinical Questionnaire, the Scale of Caregiving Appraisal, Hospital Anxiety and Depression Scale - HADS, Stress Perception Scale, Social Support Scale - SSS, Ways of Coping, and the Barthel Index. 16 Multiple Regressions were performed, 8 for each group. The results obtained show us differences between groups with respect to predicted variables. It is evident the role of sex in the group of spouses and Social Support in the Children Group and the inability of coping strategies for the prediction of the variables in both groups.
Keywords: Alzheimer Disease, Caregivers, Depression, Anxiety, Stress
Cite this paper: Manuela Leite , Vera Almeida , Maria Prazeres Gonçalves , Predictive Study of Psychological Variables Impact in Family Caregivers of Patients with Alzheimer, International Journal of Statistics and Applications, Vol. 5 No. 6A, 2015, pp. 6-14. doi: 10.5923/s.statistics.201501.02.
Article Outline
1. Introduction
- Alzheimer's Dementia is the most common form of dementia in the elderly [1, 2], and it’s able of being the «epidemic of the century» [1], taking into account the association with senescence and the increasing aging of population. The progressive and disabling character of the disease, combined with cognitive and behavioral changes, loss of recognition of caregivers, among others, are stressful elements in care [3]. The negative impact of caring for these patients is widely documented in the literature, leading to worldwide recognition of caregiving as a «serious public health problem» [4]. The psychological distress, sleep fragmentation, reducing of social activities [5], increase the risk of physical morbidity [6-9] and psychological [4, 10-12]. Chronic exposure to the suffering of others [3, 4] has a negative impact on the mental health of the caregiver, with depression, anxiety, negative mood and psychiatric disorders being the emotional expression of this suffering [4]. The increase in liabilities [13]; co-residence, severity of illness, marital [14]; physical capacity, perceived social support [15], and the fact that the care of dementia patients involves a continuous process of adaptation [16], constitute as stressful and disturbing factors of mental health. The age and gender of the caregiver also play a leading role [15], as well as the number of hours in care [17], coping strategies [18] and perceived social support [19]. Taking into account all these factors and the "Caregiving and stress process Model» [20], this study aimed to identify the predictors of: (1) Evaluation of Care; (2) Depression; (3) Anxiety; and (4) Stress - Impact variables in the care of relatives with Alzheimer's dementia.
2. Method
2.1. Sample
- The sample consists of 86 family caregivers, divided into two groups: spouse caregivers - SG (n=49) and children caregivers - CG (n=37). As selection criteria for both groups was defined: (1) be the primary caregiver of a patient with Alzheimer's dementia; (2) provide care for at least six months; and (3) the patient is not institutionalized. The nature of the relationship defined the inclusion of each subjects in the group.The SG has an average age of 69.86 years old (DP=7.69), predominance of female gender (59.2%) and education at the primary level (67.3%) and 22.4% illiterate. 87.8% dedicate 12h to 24h to care, and most do it for more than three years. The CG has an average age of 48 years old (DP=19.10), and 89.2% female. All are literate, in which 35.1% have four years of education (primary education), distributing the remaining for the primary, secondary, and higher education. 81.1% also dedicate 12h to 24h to care and the majority (54.1%) cares for more than three years. As for the motivations underlying the care, most caregivers do it for love (81.6% SG, 89.2% CG). 59.2% of spouses and 54.1% of the children identify changes in patterns of relationship with patients, however, 81.6% of the spouses keep feelings of marital, and 51.4% of children, of membership. Both groups (57.1% SG, 67.6% CG) perceive changes in their life, from the provision of care, highlighting the loss of freedom and labor activity in CG.With regard to patients, in the SG there is an equitable distribution for the first and second phase of the Clinical Dementia Rating (CDR), with 38.8% in stage I (mild) and II (moderate), and 22.4% in Stage III (severe ). In CG there is a predominance of patients in Stage II (48.6%), followed by I (27%) and III (24.3%). Most patients have no aggressive behavior (61.2% SG, 67.6% CG), and still retains recognition of their caregiver (67.6% SG, 64.9% CG). The SG patients have lower level of dependence - Barthel Index (M=71.12, DP=26.03), compared to the CG (M=48.38, DP=34.12).
2.2. Instruments
- The Socio-demographic and Clinical Questionnaire, was aimed at collecting demographic data (e.g. age, gender), clinical (e.g. CDR, existence of aggressive behavior, caregiver recognition), and care (e.g. time of care, number of daily hours, changes in the relationship with the patient, changes in the life of the caregiver, underlying motivations to care).Scale of Caregiving Appraisal - SCA [21]. It is a scale composed of 13 questions. It consists of three factors: Factor 1 “Subjective Overload” - negative manifestation of caregiver stress; Factor 2 “Caregiver Satisfaction” - interpreted as the idea of benefits that the caregiver has for his efforts; Factor 3 “Impact of Care” - interruption in lifestyle of the caregiver. The count consists of the sum of the scores (1-5) for all items that make up each of the factors.Hospital Anxiety and Depression Scale – HADS [22]. The scale consists of 14 items, divided into two groups: 7 items concerning the assessment of depression and 7 to anxiety. These are shown alternately in the form of statements, to which the individual responds accordingly to how he has felt in the past week, in order to evaluate levels of anxiety and depression. Global Scale and sub-scale scores vary from 0 to 21 points, which represent a growing grading scale of depression and anxiety levels. According to the authors [23], the value 8 is regarded as a cut point, which lower values represent the absence of anxiety and depression. Amounts exceeding 8 suggest the presence of a disturbance. Thus, according to the score and the degree of severity of depression and anxiety, they propose the following classification: “normal” (0-7), “light” (8-10), “moderate” (11-15) and “severe” (16-21).Stress Perception Scale – SPS [24]. The scale consists of 14 questions that assess the intensity of feelings and thoughts experienced (or not) by the subject over the last month presented in the claims. The sum of the scores allows to obtain a total value that is evaluated in terms of its intensity: the higher the total score, the greater is the stress level at which the individual is subject.Scale of Social Support – SSS [25]. This is a scale composed of 16 claims, self-filling (as "Likert"), through which assesses the overall social support perceived in three dimensions that correspond to the three scale factors: Factor 1 - Informative support; Factor 2 - Emotional Support; and Factor 3 - Instrumental Support. The sum of the scores obtained on each item, allows to obtain a total for the scale and that gives us the sense of whether that person enjoys (or not) of social support, and simultaneously enables us to assess to what extent this support is more or less effective.Ways of Coping [26]. Rating scale of coping strategies, divided into 8 sub-scales: (1) Confrontational Coping; (2) Distancing; (3) Self-Control; (4) Social Support Seeking; (5) Accept Responsibility; (6) Escape-Avoidance; (7) Planned Resolution of Problem; and (8) Positive Reappraisal. The Scale is self-filling, through which the subject evaluates each of the coping strategies (items). Regarding the problem situation, this should be recent and in the research in question was partially defined by the investigator in the sense that it should be relate to the provision of care to family with AD. From this assumption one must then choose a particularly stressful situation and occurring preferably in the last week. Regarding the count, «we used the method of absolute scores (sum of the responses of the subjects to the items that make up the scale). This method summarizes the extent to which each type of coping has been used in a particular event.The Barthel Index, allows the assessment of the functional capacity of patients through the autonomous fulfillment capacity – “independent”, with “help” or “dependent” of a series of daily tasks (e.g. feeding, bathing, dressing, personal hygiene; using the bathroom, changing seat/bed; walking; urination capacity). The degree of autonomy vs. dependence is obtained through the sum of the values obtained in each of the tasks, ranging between 0 and 100, may be classified as: Grade I - Independent (100); Grade II - A little Dependent (50-100); and Grade III - Very Dependent (0-50).
2.3. Procedures
- The evaluation of the caregivers was mainly conducted in hospital context, in collaboration with the medical assistants who informed about the diagnosis and stage of disease (CDR). They were also recruited through the Portuguese Association of Family and Friends of Alzheimer's patients. The first step was the approval of the investigation by the Ethics Committees. After indication of medical or APFADA, caregivers who met inclusion criteria were duly informed and enlightened about the research and signed informed consent. The questionnaires were self-filled, except in cases where the caregiver was illiterate. In this situation, the questionnaires were read aloud and recorded the caregiver options.Data analysis was performed using the Statistical Package for the Social Sciences (SPSS) version 20.0. The predictive study of impact variables in care in the group of spouses and children was made through the Multiple Regression and Enter method, allowing us to predict the criterion variable (dependent) through a set of variables simultaneously. The criterion variables (predicted), are the Caregiving Appraisal (“SCA”), Depression (“HADS depression”), Anxiety (“HADS Anxiety”) and Stress (SPS). Aware of the size of our sample, the study we wanted to run (predictive study of these variables, but in both groups), and the high number of variables that could influence the care, there were a series of multiple regressions in order to determine the most important variables, and to be included in the “final” model of regression: model that allowed the determination of predictors of the criterion variables. The choice of variables to be included in different “multiple regression”, from now on designated Models (1, 2, 3 and 4) resulted in a systematic review of the literature which contributed the model of «Caregiving and stress process» [20], Multiple Regression Models: Demographic Variables, Objective, subjective, and modulating (Figure 1).
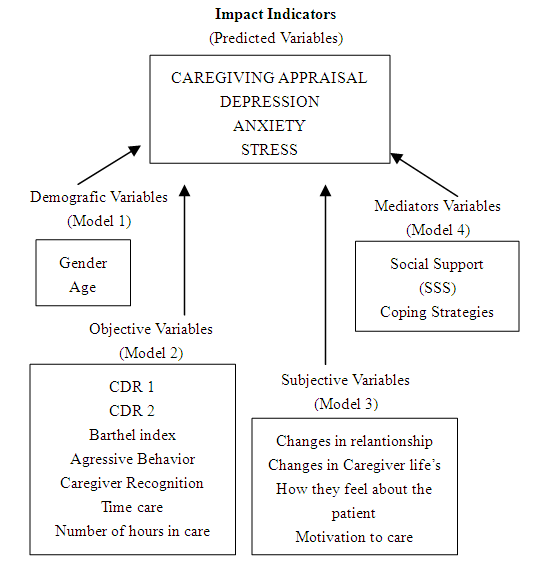 | Figure 1. Model underlying the various multiple regressions analyses |
3. Results
3.1. Multiple Regression Analysis using as dependent Variable the Caregiving Appraisal
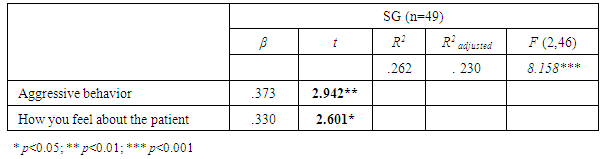
- Of the four regression models in the SG, only the third model is statistically significant (F(4.44)=2.538; p<.05), explaining 18.7% of the variance. However, a statistically significant variable and another near the significance level was identified to be included in the final regression model (Table 1): «Aggressive behavior» (t=2.671; p<.05), and «How do you feel about the patient» (t=1.880, p<.10). In CG, none of the models proved statistically significant, having however identified four statistically significant variables or near the significance to be included in the final regression model (Table 2): «Changes in the caregiver's life» (t = 2.319; p<.05); «How do you feel about the patient» (t=1.874, p<.10); Social support (SSS) (t=1.713, p<.10); and WOC Accepting responsibility (t=-2300; p<.05)
|
|
3.2. Multiple Regression Analysis using as Dependent Variable the Depression (HADS-Depression)
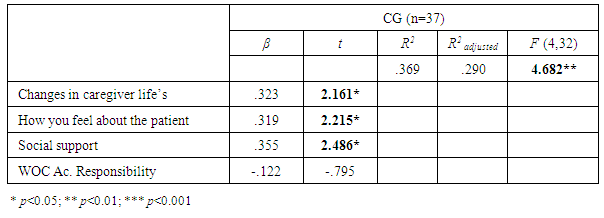
- With regard to depression, we found that, after four regressions for each of the groups, very few variables may have a predictive value existing, however, differences in each group. In this context, in the final regression model of the spouses will be considered only the «Caregiver gender» (t =-2542; p<.05) and their «recognition» by the patient (t=-2469; p<.05) (Table 3), whereas in children, it will be only tested the Social Support (t=-2777; p<.01) (Table 4).
|
|
3.3. Multiple Regression Analysis using as the Dependent Variable Anxiety (HADS-Anxiety)
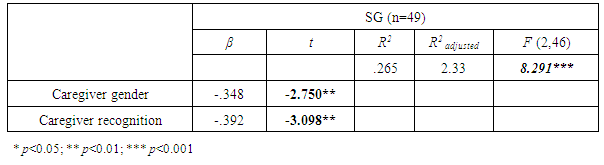
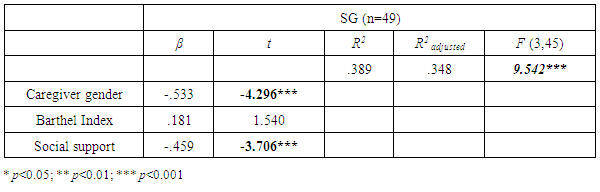
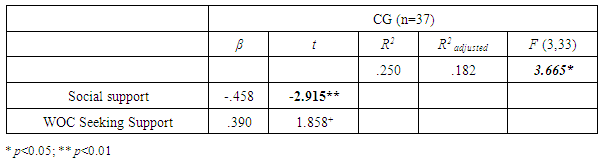
- With regard to Anxiety and, irrespective of statistical significance of each of the various models, they allow us to identify a set of variables to be included in the final regression models, given their possible predictive capability. Therefore, in the SG, we identified once again the Caregiver gender (t=-2.330; p<.05), the dependency level indicated by the "Barthel Index" (t=2.069, p<.05), and finally Social Support (SSS) (t=-2.218, p<.05). Regarding the group of children, we found that only Social Support (t=-2.591; p<.05), and «Seeking for Social Support» Coping (t=1.722, p<.05), will take a leading role in anxiety prediction. The final model found for SG (Table 5), is characterized by its predictive value and level of significance (F(3.45)=9,542, p<.001), allowing us to explain a reasonable percentage of total variance scale (38.9%). In respect of predictor variables, like depression, we find that female is highly associated with high levels of anxiety symptoms (t=-4.296; p<.001). The social support scale is also strongly correlated with anxiety (t=-3.706; p<.001), corresponding higher levels of anxiety to lower levels of social support. Finally, although in Model 2 the dependency level rise to a probable predictor, when we proceed to the final model, we found its inability to predict anxiety.
|
|
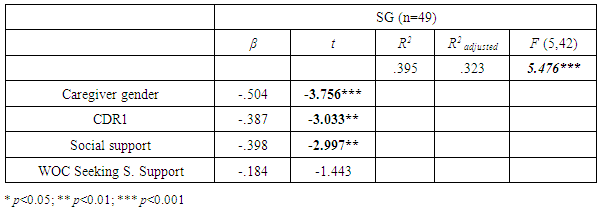
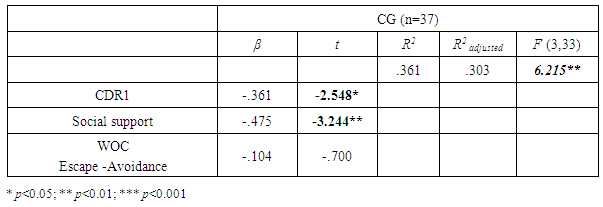
3.4. Multiple Regression Analysis using as the Dependent Variable Stress (SPS - Stress)
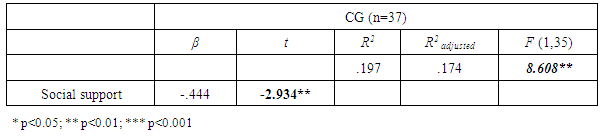
- With regard to stress, and as in previous models, neither models is significant, and only the Model 4 presents a considerable predictive value (spouses, 46%; Children, 66%). Regarding the selection of variables to be included in the final models, obviously we chose those correlated with the dependent variable in question. Therefore, at SG we found the caregiver gender (t=-470; p<.05), the «CDR1» (t=-1.414; p<.10), the Social Support (t=-1.804; p<. 10), and «Seeking for Social Support» Coping (t=-2.006; p<.10). At CG, the variables that significantly correlated with the dependent are: CDR1 (t=-1.814; p<.10), Social Support (t=-3.551; p<.01), and «Escape-avoidance» Coping (t=-1.848; p<.10).However, through Table 7, referring to the final regression model in SG, we found that when we put all of these variables in a single model, coping strategies lose their predictive power. However, there are other variables such as those relating to the stage of disease and social support, which take on a much higher level of significance.
|
|
4. Discussion
- The main objective of this study was to identify predictors of the “impact” of caring for relatives with Alzheimer's dementia, and is defined as dependent variables the four impact variables: Caregiving Appraisal, Depression, Anxiety and Stress. Please note that this derives from the comparative study between groups regarding dependent variables. Through the same, we found fairness of the results obtained by each group, and therefore an overall result that translates into an adjustment to the provision of care achieved by both groups. These results, denser the relevance of predictive study towards a greater understanding of intergroup results.In this sense, we conducted a vast set of multiple regressions, according to a model we have outlined, which consisted of grouping the variables into several “models” of regression (Model 1 to 4), aiming the selection of variables to be included in final regression models, according to their level of significance. Thus, resulted eight final models, two for each of the dependent variables, and for each of the groups (spouse and children) with a high level of significance of the final regressions models (p <0.01 and p <0.001).Regarding the caregiving appraisal, from the results obtained in the various multiple regressions performed for SG, we identified two possible predictors, “existence of aggressive behavior” and “how do you feel about against the patient”, and it is confirmed through the final regression model its predictive capabilities. Thus, the absence of aggressive behavior and the maintaining of marital relationship are two factors that influence the assessment that the spouse caregiver effects about caregiving. The harmful effect of aggressive behavior in care has been widely reported by several researchers [27-29], particularly in terms of caregivers mental health [30]. Spouses seem more exposed to this kind of problems compared to children caregivers, presenting less effective in responding to such behavior, perhaps due to the negative implications thereof at the level of marital intimacy [31].About the question “How do you feel about the patient?” the maintaining of marital relationship, as opposed to the adoption of the parent role, is one of the most significant predictors in the evaluation that spouse caregivers perform of care, and the impact on their lives. These results corroborate the other results [32], in which no significant changes in terms of marital closeness led some of the 50 interviewed wives to feel a huge bonus from the provision of care, compared to those who noticed changes. We note that, although 40.8% of spouses relate changes in the way to relate to the patient, 81.6% perpetuate marital and the feeling of spouse, accordingly to the percentage of patients who still retains the recognition of the caregiver as their spouse. Perhaps, this is one of the main factors underlying the resilient capacity of spouse caregivers.As for the CG, the multiple regressions allowed us to select four independent variables to be included in the final model: “change in the life of the caregiver”, “how do you feel about the patient”, Social Support and «assume responsibility» Coping. But when included together in the final model, we found that the coping strategy has lost its significance, and therefore their predictive ability.Regarding the question “How do you feel about the patient?”, we found that in this group the maintenance of the filial relationship pattern also plays a leading role, which is positively associated with a rise about the evaluate they effect of care. Like the previous group, 51.4% perpetuate the feeling and the parental relationship, while 64.9% of patients maintain recognition of their caregivers as simultaneously being their children.However, due to the nature of the filial relationship compared with marriage; the fact that their patients, belonging to the group of children, were older and more dependent, it makes it easy for children the perception of role reversal compared to the group consisting of spouses.Although there are no statistically significant differences between groups with respect to changes in the life of the caregiver from the provision of care, we found that the absence of changes at this level is a predictor of positive evaluation of care to the parent. The relevance of changes in the lives of children caregivers at the level of assessment they perform of care, it is understandable, considering the losses they referred to (e.g. freedom, occupation). Thus, lying still in a very active phase (middle-aged), at professional level or family, these losses may have a negative impact in the economic sphere, family, social and personal (self-esteem).Finally, and accordingly with the role of social support in adapting to care advocated by several authors [33, 34], we found that a greater perception of social support predicts a more positive assessment of care.Regarding the prediction of depression, although several authors profess a set of factors directly associated with the pathology in question (e.g. high number of hours in care, presentation of problematic behaviors) [17]; the severity of the disease [15]; the role of satisfaction with social support, among others [28], we find that in the group of spouses, only the “caregiver gender” and “recognition of the same”, have predictive power.In addition, and similar to what was reported by Teri [15], the female is a vulnerability factor, finding associated with more pessimistic assessments of care. These results represent the natural tendency in which women are at significantly higher risk than men [35].Loss of recognition by the patient of his caregiver as his spouse, is a definitive milestone in the impracticality of maintaining the marital relationship, and the inevitable return to individuality. Associated with the loss of relationship, we found especially the loss of intimacy (past and present), which is associated with depression symptoms [11].Regarding the CG, from various multiple regressions, the Social Support was the only variable to be included in the final model, proving the positive effects of social support on the mental health of caregivers [36, 37] and the negative relationship with depression [38]. In this group, higher levels of social support predict lower levels of depression.Regarding the prediction of anxiety, we identified in the SG, through the various models of regressions, three potential predictor variables: Caregiver gender, the level of patient dependency and Social Support. However, only the gender of caregiver and the social support have proved effective in predicting anxiety in this group. Taking into account the link between depression and anxiety, it’s easy to understand the vulnerability of women. With regard to Social Support, this is shown in the literature as a protector of mental health of caregivers, checking on the group in question its predictive capacity about anxiety, but not depression, unlike the group of children.In the group of children, there has been the inclusion of only two variables in the final model: Social Support and «Seeking social support» coping. However, and like other variables, we are witnessing a loss of predictive capability of coping strategies, confirming once again the positive effects on social support in this group, reducing the levels of depression and anxiety.Finally, the level of stress, we found that this was the predicted variable with the greatest number of factors to be included in the final model, either in the SG either in CG.Thus, in the group of spouses, we first verify the inclusion of coping strategies, specifically “Search for Social Support” Coping, although they cease their significance when included in the final model. To this were associated the caregiver gender, Social Support and the stage of the disease, appearing us for the first time as an impact predictor of caregiving.With regard to caregiver gender, it confirms the vulnerability of females to the level of stress, advocated by Chappell and Reid [39], and also according to literature that indicates women have higher stress levels than men, revealing more ineffective in controlling disturbing thoughts and experience more family conflicts [31]. The positive effect of social support (SSS) in reducing stress, had already been documented, regarding it as a «stress-protective factor» [40]. Regarding the stage of the disease, it is found that the CDR Phase II (moderate), predicts higher levels of stress on SG. This is due to the worsening of amnesia symptoms, disorientation, and emergence of apraxia, agnosia, aphasia, depersonalization, behavioral disturbances, gait, increased risk of escape and loss of recognition of their caregiver [41] implying by the caregiver an active and ongoing attitude of supervision.In GF, there is also the inclusion of the stage of the disease in the final model, as well as Social Support and «Seeking social support» coping. Once again, we see the inability of coping strategies, as a predictor variable. Nevertheless, we confirmed the pernicious effect of Stage II of the disease correlating with higher levels of stress as well the positive effect of social support, reducing stress levels.Figure 2 shows the final regression model in SG and Figure 3 in CG.
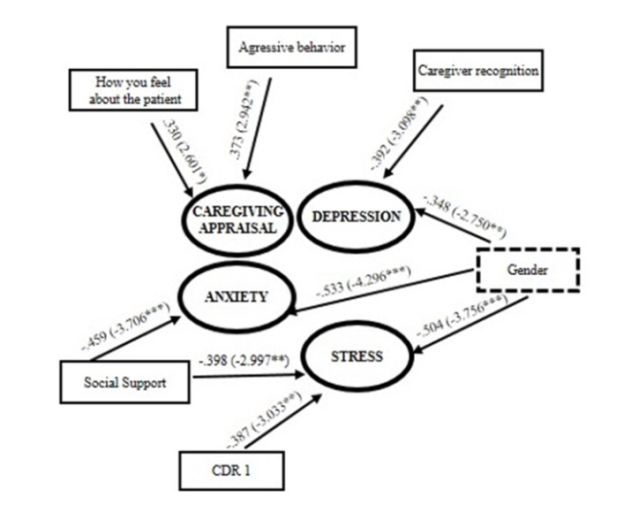 | Figure 2. Predictive Model of caregiving impact variables in Spouse Group |
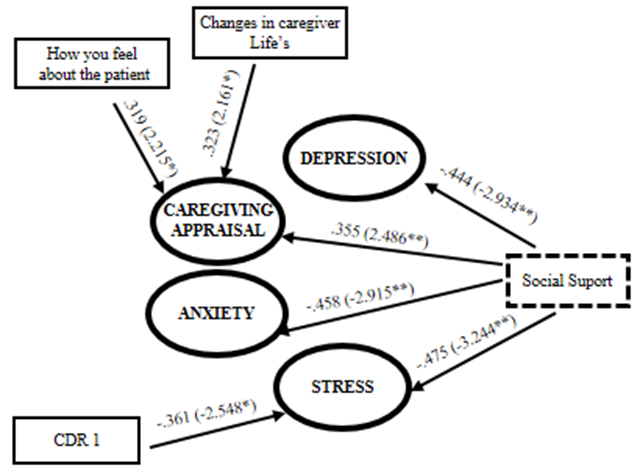 | Figure 3. Predictive Model of caregiving impact variables in Children Group |
5. Conclusions
- The global analysis of the various regressions performed in both groups, to determine predictors of the impact of caregiving (caregiving appraisal, depression, anxiety and stress), allows us to conclude that: (1) the predictors vary broadly according to the group of belonging, confirming that nature of the relationship plays an important role in providing care; (2) In the group of spouses, the female is undoubtedly a psychological vulnerability factor, associating with higher levels of depression, stress and anxiety; (3) The maintenance of premorbid relational patterns (conjugality and affiliation) are a good predictor for both groups, regarding the effecting evaluation of care, and therefore the level of the impact of caregiving; (4) Social support plays an important role in maintaining the mental health of caregivers, especially in the group of children; (5) The inability of coping strategies patents on the scale of “Ways of Coping” in predicting the impact of care, in both groups, although frequently mentioned in the literature as a modulating variable [20, 42, 43]. However, this failure may be related to the long durability of the stressor (mainly equal to or greater than three years at our sample), leading to a decrease of their efficacy [44]; (6) Problematic behaviors just predict the evaluation of care performed by SG, although referenced in the literature as constituting a major challenge in providing care [28], and having a negative impact in mental health of caregivers [30]; and (7) The time elapsed since the start of care; number of daily hours devoted to it; level of patient dependency as well as the physical health of caregivers, do not influence the impact of caregiving in our sample (whether the spouses or the children). In short, the results clarify the role played by the type of prior existing relationship between the caregiver and the patient and the impact of care, which should be taken into account in the delineation of intervention strategies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML