-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Statistics and Applications
p-ISSN: 2168-5193 e-ISSN: 2168-5215
2015; 5(6A): 1-5
doi:10.5923/s.statistics.201501.01

Mental Illness of the Oldest, Nutritional Status and Arterial Hypertension
Sotto Mayor Margarida 1, Pestana Helena 2, Reis Gorete 3, Santos José Manuel 4
1Centro de Formação Continua, Hospital Magalhães Lemos, Porto, Portugal
2Departamento de Métodos Quantitativos para a Gestão e Economia, ISCTE-Instituto Universitário de Lisboa, Lisboa, Portugal
3Escola Superior de Enfermagem de S. João de Deus, Universidade de Évora, Évora, Portugal
4Departamento da Saúde, Universidade Fernando Pessoa, Porto, Portugal
Correspondence to: Sotto Mayor Margarida , Centro de Formação Continua, Hospital Magalhães Lemos, Porto, Portugal.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Changes in nutritional status and high blood pressure are very common in elderly with mental disorders. Currently, the interest in knowing associated factors to those variables is to prevent morbidity and mortality risk. The study aim was to evaluate the relationship between mental disorders, nutritional status and blood pressure. It´s a cross-sectional study in a sample of 99 elderly living in community that had a psychiatric emergency episode. Data were collected from the initial evaluation form (IE). Results show multiple pathologies, cognitive deficits, high blood pressure and change in body mass index (BMI). Conclusions: In most of the sample BMI is associated with several co morbidities and co-exists with a temporal disorientation and arterial hypertension. Prevention is the key to maintaining health and well-being.
Keywords: Mental Illness, BMI, Arterial Hypertension, Dementia
Cite this paper: Sotto Mayor Margarida , Pestana Helena , Reis Gorete , Santos José Manuel , Mental Illness of the Oldest, Nutritional Status and Arterial Hypertension, International Journal of Statistics and Applications, Vol. 5 No. 6A, 2015, pp. 1-5. doi: 10.5923/s.statistics.201501.01.
Article Outline
1. Introduction
- The changes in body composition associated with the aging process are reflected in increased of fat body mass, at visceral level, and decreased of lean body mass expressed in sarcopenia, decreased of bone mass and decreased of water at the expense of intracellular sector [1]. Therefore, the nutrition and health of the elderly have to be framed in an enlarged perspective covering all his life. With aging, come upon changes in eating behavior, which will lead to major differences in the choice of food, influenced in turn by the interaction of several factors: biological, economic, psychological and social ones. The association of changes in Body Mass Index (BMI) with changes in blood pressure predispose the outbreak of severe pathological conditions such as coronary heart disease, heart failure, peripheral arterial disease and kidney failure [2], reasons which pro-active steps are needed. In developed countries, the obvious malnutrition can reach 5-10% of the elderly living in their homes and more than 50% in elderly patients and at the time of hospital discharge [1].As people live longer, the quality of longer life becomes a central issue for personal life and social well-being. Consequently, it is frequent multiple pathologies and also dementia. Dementia is commonly associated with alterations in the nutritional status of which weight loss is the most frequently described. The etiology of weight loss is not properly clarified. Several factors are involved and among them is the decrease in food intake, affecting cognitive function and functional capacity. This study aims to characterize the nutritional status of older people with mental illness who have had an episode of psychiatric emergency.
2. Methodology
2.1. Population / Sample
- This is a cross-sectional, descriptive and correlational study. The sample consisted of 99 elderly people involved in a psychiatric emergency episode in the biennium 2013/2014. They were respected all the ethical requirements of a work of this nature, and the study was approved by the Ethics Committee for Health of the hospital where the study was conducted.
2.2. Data Collection Instrument
- It was used the initial evaluation form (IE) set out in the clinical process where the records of sociodemographic, clinical and functional variables are. The following variables were used: Gender, Marital Status, Age, Hours of sleep a day, Type of humor, Reason for hospitalization, Personal history, Blood pressure values (BP), Body mass index (BMI), Mental state - Orientation (time / space / alo and auto) - and functionality (mobility and reliance on self-care). The objective of the study was to evaluate the relationship between mental disorders, nutritional status and hypertension in people with mental disorders and cognitive impairment, who have had an episode of psychiatric emergency.The main variables in the study are mental disorders, nutritional status and hypertension, registered in IE form. The nutritional status was evaluated by calculating the body mass index (kg/m2) using the formula weight/ height2 (kg/m2) and it was used as classification criteria the cutoff points adjusted to the elderly proposed by the Nutrition Screening Initiative: ≤24 kg/m2 (underweight); 24.1 to 27 kg/m2 (normoponderal); ≥27,1Kg / m2 (obese).
2.3. Procedures
- Data were collected from clinical record. The study took place in the biennium 2013/2014. The ethical principles governing research with clinical processes were respected, in particular the anonymity and confidentiality of data. Statistical analysis was descriptive and correlational with categorical analysis models [3]. We used "IBM SPSS Statistical 21 Software" for descriptive/correlational statistical analysis of the sample. It is considered statistically significant values of p<0.05.
3. Results
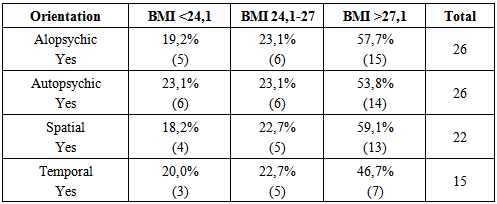
- The sample is mostly female (85%), widowed (41.7%), with a mean age of 72.4 years, and the mode of 77 years, autonomous (69.7%) and overweight (66.7%). With regard to gender, it turns out that men are more overweight than women in 19% of cases. Of the 99 persons in the sample, it was found that only 46 (46.5%) were filled in IE form the item related to body mass index (BMI), and from these 40 persons (87%) had hypertension, which differ significantly from those who do not. The ages of the persons suffering from hypertension vary between 65 and 97 years.
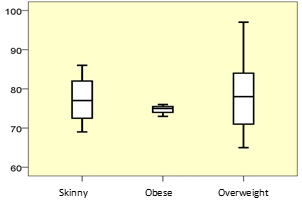 | Figure 1. Ages (years) and BMI |
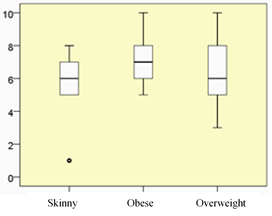 | Figure 2. Sleep (hours) and BMI |
|
4. Discussion
- A sample of community elderly who had an episode of psychiatric urgency was studied. It was addressed to mental disease associated with body mass index and hypertension to be two co morbidities strongly linked to high morbidity and mortality. Several authors have shown the benefits in prevention of cerebral vascular accident (stroke) and cardiovascular diseases [4, 5]. Hypertension is associated with an increased of cardiovascular morbidity and mortality in all age groups [1]. The blood pressure, either systolic (> 140 mmHg) or diastolic (> 90 mmHg), occurs in approximately half to two thirds of the population aged 65 years and 75% of the population aged 80 years of age or more [1] and data from this study corroborate this author.The study sample is derived from an aging population in most women, widow, autonomous, with cognitive deficits and with high BMI. In this study, on average, as you go older the BMI increases. The possibility of living alone, as in case of widowhood and divorce, seems to indicate a greater risk of hypertension and BMI of greater obesity; however, the authors did not report large changes in relation to marital status. The trend of increased BMI with gender privileges the male, which is consistent with other authors that indicate an accumulation of abdominal fat by men [6]. According to most authors, the pressure is increased in prevalence with age and this is associated with other co morbidities, including some structural changes and greater stiffness and aging organs and systems [7], coincident with the data found in this sample.The internment of people with high blood pressure and BMI ≥27,1Kg/m2 was primarily due to changes in behavior, depressive symptoms, anxiety and psychotic symptoms. Many disease processes in elderly course with confusional frames, which necessitates the distinction between multiple etiologies that lead people to the psychiatric emergency room. You have to look for history of alcoholism, fever, diabetes, head trauma, epilepsy, history of multiple surgeries and dementia processes. It is also important to doubt a state that settles too fast [8]. In situations of stress, and with any of these diagnoses, the patient may present some disorder that makes it socially inadequate, with limited control and that, therefore, need medical and nursing care. Sleep disturbance also present in this sample show that people with normoponderal BMI have a more regular sleep. It is known the change of sleep that follows on from morbid obesity processes and BMI increasing [6].In this study, people with normoponderal BMI sleep more hours per day, although the differences are not significant. Obesity is, of course, a multifactorial chronic disease very consistently influenced by lifestyles, and in this sample, most people did not mention any interest in any physical activity. Physical activity is now supported by a very robust body of knowledge that allows you to establish positive associations with the qualitative and quantitative dimensions of aging. Modifiable risk factors like dyslipidemia, hypertension, diabetes, excess of adipose tissue, pro coagulant state, pro inflammatory state, low cardiopulmonary fitness or inactivity, lack of knowledge, alone or more frequently in combination with each other, exponentially increase the risk of disease [9]. And anyone can have an episode of psychiatric urgency in the context of a mental sick, but bring with you to the hospital a number of diseases whose treatment is not negligible [10]. Epidemiological studies have shown a relationship between the state of malnutrition and changes in cognitive function, functional capacity and behavior [11]. Most people in this sample have high blood pressure and dementia, especially those who are overweight, and this is a high nutritional impact syndrome, where pictures of nutritional risk or even malnutrition can be installed quickly, which justifies the need for a nutritional and dietary early intervention. Vellas B. et al [12] showed that the weight loss can be progressive or severe, being a determinant of morbidity and mortality. The etiology of weight loss is multifactorial and various mechanisms seem to be involved, impairing cognitive function and functional capacity [13], may be present the dysfunction of complex of the regulation of body weight, increase in the basal metabolism and energy expenditure, hyperactivity, difficulty in feeding and decreased food intake. All these features exist in this population because a high percentage of people have dementia processes or suffer from other psychiatric disorders inducing some uncontrollable activity which often "escapes" to the technical verification, however, these diseases in this sample are not significantly associated with BMI.As regards to mobility, it is found that most people are independent, as verified by Christensen et al. [10] in their study in different countries, which found there seems to be an adjustment to the progressive increase of aging. This adjustment caused older people to remain functionally autonomous for more time, corresponding to an adaptive aspect of the population. The feeding behavior changes as a result of some sensory changes such as some loss of taste, lead to the use of more salt and that it worsen some pathological conditions associated with hypertension, producing new episodes of sick that articulate with other factors: biological, economic, psychological and social ones [2].With regard to mood changes, it appears that there is the same proportion of people with hypertension and mood problems. As the BMI increases, moving from one category to the next, decreases by 13% the likelihood of having mood problems. States of anxiety and fear of what might happen to them are some of the reasons for presenting this sample of high history of psychological disease and hypertension, which is in agreement with other authors that indicate anxiety as one of the factors that predispose to hypertension [14]. Most people in this sample have high blood pressure and dementia, especially those who are overweight. In this context, we take the values found in the variables of mental state. According to neuropsychology of orientation, temporospatial disorientation occurs generally in psycho-organic frameworks, while three brain areas are compromised, particularly in diffuse cortical lesions as in Alzheimer's disease, the mesial lesions as is known in Korsakoff syndrome and diseases that affect the brain stem and the ascending activating reticular system as in confusion states where there floating impaired consciousness [15]. These data are consistent with the data from this sample, which was tend to be more oriented towards themselves and the world around them than what happened to the time variable, since more than half of the people was disoriented, had hypertension and high body mass index.
5. Conclusions
- Factors associated with BMI indicate the likelihood of reflection on the importance of the field of intervention of the different technical health professionals across the life cycle. This sample living in the community, has a high risk factor to have the hypertension and high BMI as health reference, both shared with mental illness. Mental perspective, it is interesting to early assessment of disease processes that occur with cognitive impairment to intervene with nutritional supplements or balanced diets slowly allowing adequate BMI and simultaneously reducing the blood pressure values in itself harmful from a cardiovascular point of view and they also generators of mental illness, including dementia processes of vascular origin.
6. Implications for the Practice
- The older ages, the association of age with multiple co morbidities require an evaluation and disciplinary action that reflects what is known about the psychological, biological (nutritional) and social balance. Data collection at the time of initial evaluation is a precious support for the planning of the intervention. Future bet goes through implementation of global policies where it includes nutritional care, as well as the creation of "legal beacons" to marketing and investment in nutrition literacy, nutrition education and health promotion from an early age and throughout the life cycle.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML