-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2015; 5(3A): 20-22
doi:10.5923/s.health.201501.07
Lichen Spinulosus: Case Report and Review of Literatures
Khalid Al Hawsawi1, Kholood Almehmadi2, Bushra Alraddadi3, Ohood Aljuhani2
1Dermatology Consultant, Head of Dermatology Department, King Abdul Aziz Hospital, Makkah, Saudi Arabia
2Medical intern, King Abdul Aziz Hospital, Makkah, Saudi Arabia
3Dermatology Resident, King Abdul Aziz Hospital, Makkah, Saudi Arabia
Correspondence to: Khalid Al Hawsawi, Dermatology Consultant, Head of Dermatology Department, King Abdul Aziz Hospital, Makkah, Saudi Arabia.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Lichen Spinulosus is a rare childhood disease. It is characterized by follicular hyperkeratotic papules that may coalesce into plaques. Individual lesion shows conical projection, hair like horny spine. The etiology is unknown but genetic predisposition has been suggested as a possible cause. It has a tendency to disappear spontaneously at puberty. Herein we present a 12-year-old boy presented with 6- month- history of persistent asymptomatic skin lesions. Skin examinations revealed multiple grouped scaly, hypopigmented tiny follicular papules with horny spines on his back. Soles showed planter keratoderma. Skin biopsy showed dilated hair follicle filled with keratin plugging. Diagnosis of LS associated with planter keratoderma was made. The patient responded well to topical lactic acid (12%), urea (20-30%), and betamethasone valerate (0.1%) preparations.
Keywords: Lichen Spinulosa, Lichen Spinulosus
Cite this paper: Khalid Al Hawsawi, Kholood Almehmadi, Bushra Alraddadi, Ohood Aljuhani, Lichen Spinulosus: Case Report and Review of Literatures, Journal of Health Science, Vol. 5 No. 3A, 2015, pp. 20-22. doi: 10.5923/s.health.201501.07.
1. Introduction
- Lichen spinulosus (LS) is a genetic disorder of keratinization of hair follicles. LS was first described by Adamson in 1908. [1] It is a member of the family of follicular keratotic disorders, which includes keratosis pilaris, keratosis pilaris atrophicans, erythromelanosis follicularis faciei, and phrynoderma. [1] The etiology is unknown. Genetic predisposition has been proposed to play a role. Other etiologies include atopy, HIV infection and lithium therapy [2, 3]. The pathogenesis shows a follicular hyperkeratosis that blocks the hair follicle. LS is slightly more common in boys than girls with no ethnical differences. It affects predominantly children though rarely adults. It appears suddenly and persists for weeks-months though rarely persists indefinitely. It is characterized by symmetrical asymptomatic, rarely pruritic, skin-coloured or hypopigmented crops of minute follicular papules with projecting keratinous spines without erythema that appear as nutmeg grater or sand paper texture or goose bumps like appearance. LS usually involves extensor surfaces of arms, trochanteric regions, neck, abdomen, buttocks, thigh, popliteal fossae, and knees. The histopathology of the lesion is not specific showing dilated hair follicle with keratin plugging.
2. Case Report
- 12-year-old boy presented with 6- month- history of persistent asymptomatic skin lesions. No personal or family history of atopy. No similar case in the family. Past medical history and review of systems were unremarkable. Skin examinations revealed multiple grouped follicular papules consisting of tiny, scaly, hypopigmented follicular papules with horny spines on his back. The soles showed planter keratoderma (Fig. 1). Skin biopsy showed dilated hair follicle with keratin plugging. The epidermis and dermis were normal. Laboratory work up was insignificant. On the basis of the above clinicopathological findings, a diagnosis of LS associated with planter keratoderma was made. Patient was reassured and treated with topical lactic acid (12%), urea (20-30%), and betamethasone valerate (0.1%) preparations with excellent improvement of both L.S and planter keratoderma.
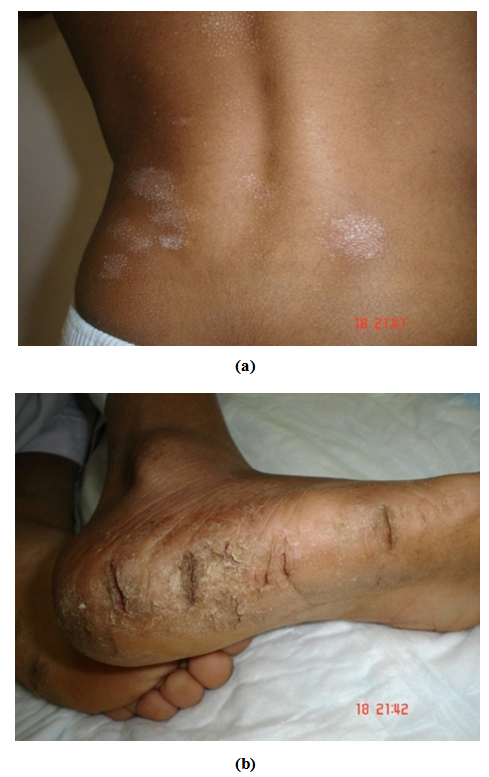 | Figure 1. Multiple grouped hypopigmented follicular papules with horny spines on the back of the patient (a), and planter keratoderma (b) |
3. Discussion
- LS appears predominantly in childhood as crops of minute follicular papules with a projecting keratinous spines without erythema. Some authors have regarded LS as a clinical variant of keratosis pilaris (K.P). The horny spine of LS can be removed, leaving behind a tiny funnel-like orifice, whereas in KP an entire individual lesion can be removed with the plug. [2, 3]Presence of spiny follicular projections is classic for LS. LS mimics keratosis circumscripta (KC). KC may be of historical interest as the most recent report was in 1979. KC is clinically similar to LS with or without palmoplanter keratosis but histologically is similar to psoriasis. [2] LS like lesions that are localized to the face has been reported with folliculodystrophy of immunosuppression (trichodysplasia spinulosa), demodicosis, follicular mucinosis, and multiple myloma. [4] LS has been also reported with Hodgkin disease, Crohn’s disease, Syphilis, seborrheic dermatitis, and following administration of omeprazole, thallium, gold, diphtheria toxin, and arsphenamine. These associations seem to be coincidental. [1-3]There are few reports of coexistence of LS with lichen nitidus. They showed the clinical and histological features of both diseases and they have been defined as“spinous follicular lichen nitidus”. [5, 6] There has been no previous report of palmoplanter keratoderma associated with LS. The presence of planter keratoderma in our patient could be a feature of LS or could be part of atopic eczema as this is the most common associated condition with LS especially the response of our patient to topical corticosteroid preparations. However, more case reports are needed to be more conclusive. Treatment of LS consists of keratolytics, emollients, and mid potency corticosteroid. Salicylic acid (3-6%), lactic acid (12%) and urea (20-40%) topical preparations are usually effective. One report of LS in a 59-year-old alcoholic patient showed improvement of the lesions within a week without any medications, only by abstention from alcohol and nutritional management with vitamin preparations. [7] Another report showed excellent response of LS to tretinoin gel at night and hydroactive adhesive application at morning for eight weeks after failure of keratolytic agents for six weeks. [8]
4. Conclusions
- LS is a rare skin disease that occurs predominantly in children though rarely in adults. Spiny follicular papules are the hallmark of the disease. Given presence of planter keratoderma as a new finding in our patient, and the fact that there are few similar conditions that mimics LS, we still need more case reports of LS to reach a more definite conclusions.
ACKNOWLEDGMENTS
- No sources of funding were used to assist in preparation of this manuscript. The authors have no conflicts of interest that are directly relevant to the content of this review.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML