-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2015; 5(3A): 17-19
doi:10.5923/s.health.201501.06
Proliferating Trichilemmal Tumor (PPT): A Case Report and Review of Literature
Khalid Al Hawsawi1, Ali Alghamdi2, Nouf Almasry3, Mohammed Aldosari4
1Dermatology Consultant, King Abdul Aziz Hospital, Makkah, Saudi Arabia
2Consultant of Anesthesia, King Abdul Aziz Hospital, Makkah, Saudi Arabia
3Medical Intern, King Abdul Aziz Hospital, Makkah, Saudi Arabia
4Consultant anatomical pathologist, King Abdul Aziz Hospital, Makkah, Saudi Arabia
Correspondence to: Khalid Al Hawsawi, Dermatology Consultant, King Abdul Aziz Hospital, Makkah, Saudi Arabia.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Proliferating trichilemmal tumor (PTT) is a rare neoplasm arising from the isthmus region of the outer hair root sheath of the hair follicle. It is mostly a benign neoplasm and has potential for malignant transformation. Herein we present a 48 years old female who presented with 3 years history of recurrent painful skin lesions that sometimes get worse and become bigger and painful and are associated with purulent discharge. There is no similar case in the family. Skin examination revealed three subcutaneous skin colored nodules, two on the scalp and one on her upper back. Excisional skin biopsy of the upper back lesion showed intact epidermis with an underlying dermal epithelial tumor composed of lobulated expansile masses of squamous cells with non-lamellated trichilemmal keratinization, patchy micro calcification, minimal focal atypia and rare mitoses. Immunohistochemistry analysis revealed membrane positivity for CD34 in more than 60% of tumor cells and focal calretinin reactivity. Ki67 immunostaining revealed a relatively low immunoreactivity showing staining of less than 5% of the nuclei which was focal and present more toward the periphery of the lobules. P53 immunostaing was negative. On the basis of the above clinicopathological features, the diagnosis of benign PTT was made. The lesions were removed by surgical excision.
Keywords: Proliferating trichilemmal tumor, Proliferating pilar tumor, Proliferating trichilemmal cyst
Cite this paper: Khalid Al Hawsawi, Ali Alghamdi, Nouf Almasry, Mohammed Aldosari, Proliferating Trichilemmal Tumor (PPT): A Case Report and Review of Literature, Journal of Health Science, Vol. 5 No. 3A, 2015, pp. 17-19. doi: 10.5923/s.health.201501.06.
1. Introduction
- Proliferating trichilemmal tumor (PTT) is a rare neoplasm derived from the isthmus region of the outer hair root sheath of the hair follicle. A synonyms of this disease include, pilar tumor of the scalp, proliferating trichilemmal cyst, proliferating pilar tumor, giant hair matrix tumor, hydatidiform keratinous cyst, trichochlamydocarcinoma, and invasive hair matrix tumor. PTT was first described by Wilson and Jones in 1966 as 'proliferating epidermoid cyst. PPT was then distinguished from proliferating epidermoid cysts in 1995. [1]PTT is thought to be as a complication of trauma, irritation, or inflammation. They may be inherited in an autosomal-dominant mode, linked to chromosome 3. [1, 2] PPT most commonly occurs during the fourth to eighth decades of life and have a distinct predilection for white women. The scalp is the most common location (90%), other locations include, upper and lower arm, the face, neck, trunk, groin and gluteal region. [3, 4]An asymptomatic nodule is often present for months to years before a rapid increase occurs in the size of the lesion, yielding lobulated and variably exophytic mass that occasionally might ulcerate. [1-5] It is characterized by frequent local recurrence. [2]Most cases pursue a favorable clinical course and surgical excision is curative. A spectrum of transformation is hypothesized, which begins with a benign pilar cyst, proceeding to PPT. PPT generally behaves in a benign fashion, although, on occasion, aggressive local growth with recurrences and metastases has been observed. [1-6]Ye et al proposed histologic criteria that could predict behavior. [1]Ye et al proposed a stratification of PTTs into the following 3 groups: Group 1, circumscribed silhouettes with “pushing” margins, modest nuclear atypia, and an absence of pathologic mitoses, necrosis, and invasion of nerves or vessels; group 2, similar to type 1 but manifested irregular, locally invasive silhouettes with involvement of the deep dermis and subcutis; group 3, invasive growth patterns, marked nuclear atypia, pathologic mitotic forms, and geographic necrosis, with or without involvement of nerves or vascular structures. Group 1 is regarded as benign, group 2 as having the potential for locally aggressive growth, and group 3 as also having metastatic potential. The latter 2 categories might be equated with low and high grades of malignancy among PTTs, so in this situation, a periodic follow up with lymph node examination and distant metastasis are recommended. Whether PTT represents a variant of SCC is an area of controversy. [6-10] There have been cases of squamous cell carcinomas diagnosed within proliferating pilar tumors, with only one reported case of squamous cell carcinoma progressing to distant nodal metastasis and death. [6-10]
2. Case Report
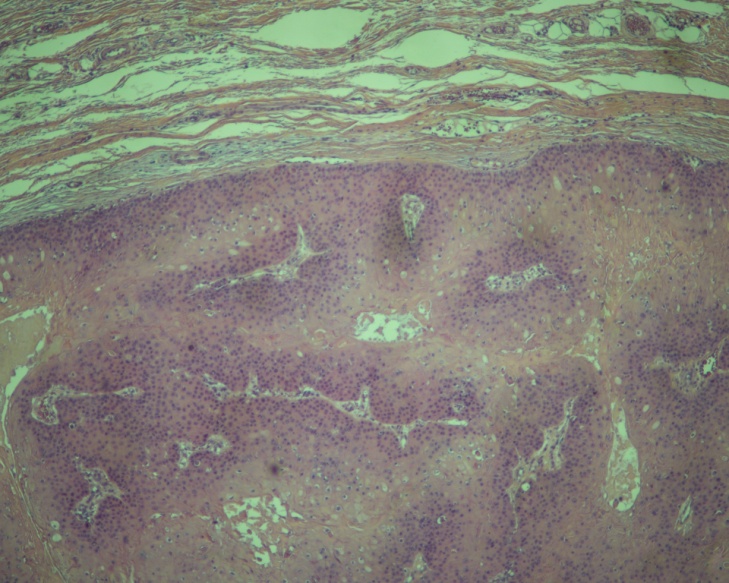
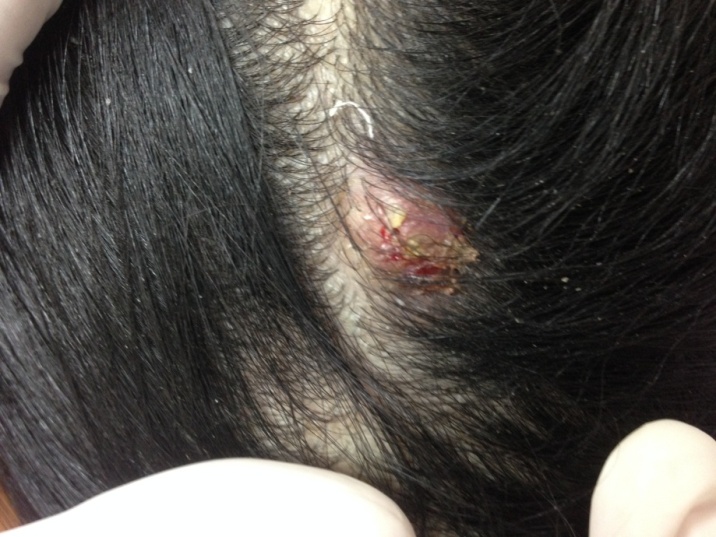
- 48 years old female is otherwise healthy presented with 3- year- history of recurrent painful skin lesions that started on her scalp and later on appeared on her upper back. The lesions sometimes get worse and become bigger and painful and are associated with purulent discharge. The lesions were removed surgically 2 years ago but one year after excision, the lesions recurred again. There is no similar case in the family. Skin examination revealed three subcutaneous nodules, two on her scalp, each measuring 3 X 3 cm and one on her upper back, measuring 7 X 7 cm. These nodules are erythematous with some erosions on the overlying skin (Figure 1). There is no lymphadenopathy. Excisional skin biopsy of the upper back lesion showed intact epidermis with an underlying dermal epithelial tumor composed of lobulated expansile masses of squamous cells with non-lamellated trichilemmal keratinization, patchy micro calcification, minimal focal atypia and rare mitoses. No invasion into the surrounding stroma. No lymphovascular or perineural invasion (Figure 2). Immunohistochemistry analysis revealed membrane positivity for CD34 in more than 60% of tumor cells and focal calretinin reactivity. Ki67 immunostaining revealed a relatively low immunoreactivity with staining of less than 5% of the nuclei which was focal and present more toward the periphery of the lobules. P53 immunostaing was negative.
 | Figure 1. Scalp of the patient showing erythematous subcutaneous nodule with some overlying erosions |
3. Discussion
- PTT classically occurs as a slow-growing nodule on the scalp of elderly women. Most tumors arise within a preexisting pilar cyst. [1-7] PTTs vary in size from a few millimeters to up to 25 cm in diameter. Lesion usually is single, painless nodule. However, multiple and painful lesions, like our case, have been reported very rarely. [1-9] Local recurrence, like our case, is not rare. The recurrence does not mean a malignant growth. [1-10] The differentiation between a benign or malignant process in these lesions can sometimes be difficult. Careful clinical and histological assessment is necessary for an accurate diagnosis. Features of malignant tumour include, non‐scalp locations, size >5 cm, and recent rapid increase in size. [3] In our patient, there was no history of rapid increase in size. Although our patient has non scalp location and the size of the tumor was >5 cm on her upper back, the histopathological diagnosis was in keeping with a benign tumor. These histopathological features include, trichilemmal keratinization, minimal focal atypia, rare mitosis and no invasion into the surrounding stroma, or lymphovascular or perineural invasion, the proliferation markers (Ki67 and p53) showed low Ki67 staining of less than 5% of the nuclei which was focal and present more toward the periphery of the lobules and lastly negative p53 staining. The positive CD34 along with calretinin immunopositivity favored outer root sheath origin of this pilar tumor over squamous-cell carcinoma.Mohs micrographic surgery, which ensures precise lesion margin control, can be performed to reduce the recurrence rate after tumor resection. [2]
4. Conclusions
- PPT is a rare neoplasm, it is more often benign and very rarely malignant. Since PTT has potential for malignant transformation, it is important to excise any mass on the scalp that has clinical characteristics of PTT.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML