-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2015; 5(3A): 6-9
doi:10.5923/s.health.201501.03
The Prevalence of Urticaria and Its Clinical Patterns in Makkah, Saudi Arabia
Mohammad I. Fatani1, Emad Bahashwan2, Khalid A. Alfif3, Abdulmajeed S. Khan3, Mohamed M. Cheikh4, Bakr B. Kalo5
1Hera Hospital, Makkah, KSA
2Umm alqura university, Makkah, KSA
3Hera General Hospital, Makkah, KSA
4Doctor Soliman Fakeeh Hospital, Jeddah, KSA
5Makkah, KSA
Correspondence to: Mohammad I. Fatani, Hera Hospital, Makkah, KSA.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
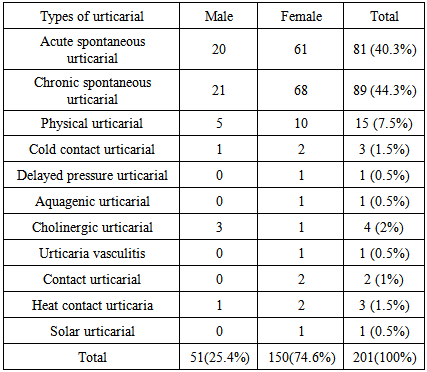
Background and Objectives: In spite of the frequency of urticaria, very few studies of its prevalence and clinical types from Saudi Arabia and Arab countries exist. The purpose of this study is to assess the prevalence and clinical types of patients with urticaria as well as the possible causes or associated (laboratory) findings and to understand the treatment modalities used in our patients. Design and setting: Retrospective review at secondary referral center.Methods: We retrospectively reviewed 201 cases of patients with urticaria who attended the Department of Dermatology, Hera General Hospital, during the period 2008–2012. Results: Of these 201 patients, 89 (44.3%) were diagnosed as having chronic spontaneous urticaria. Eighty-one patients (40.3%) had acute spontaneous urticaria, while 15 (7.5%) had physical urticaria. Atopic diseases and food allergy were present in 30.1% and 25.4% of patients, respectively. Other possible causes were thyroid diseases, drug use and collagen vascular diseases. The most common abnormal laboratory finding was the minimal elevation of the erythrocyte sedimentation rate (45%). Thyroid-stimulating hormone was normal in 80% of patients and high in only 17.6%. Disease duration was more than six months for 35.3%. Conclusions: Urticaria is a disease with significant morbidity, involves the heavy utilization of healthcare services and as such deserves more resources and attention.
Keywords: Prevalence, Urticaria, Clinical Patterns
Cite this paper: Mohammad I. Fatani, Emad Bahashwan, Khalid A. Alfif, Abdulmajeed S. Khan, Mohamed M. Cheikh, Bakr B. Kalo, The Prevalence of Urticaria and Its Clinical Patterns in Makkah, Saudi Arabia, Journal of Health Science, Vol. 5 No. 3A, 2015, pp. 6-9. doi: 10.5923/s.health.201501.03.
1. Introduction
- Urticaria is a common clinical condition representing a major concern for both physicians and patients. The term urticaria is used to describe an eruption of wheals. It is defined as a disease characterized by short-lived itchy wheals and angioedema, or both together. [1] Urticaria can be acutely disfiguring and a source of embarrassment for the sufferer, especially when it occurs on exposed parts of the body such as the face and hands. Although rarely life threatening, chronic urticaria may last for years or even decades, during which time it can severely impair the quality of life of the individual. [2, 3] Between 0.5% and 1% of the population have this condition at any particular time. [4] Women are affected twice as often as men are. [5, 6]Urticaria can be classified as spontaneous urticaria, physical urticaria and other types. Spontaneous urticaria includes acute urticaria (less than six weeks) and chronic urticaria (more than six weeks). Physical urticaria is defined as the urticarial response to specific physical stimuli, which includes cold contact urticaria, symptomatic dermographism, heat contact urticaria, solar urticaria, delayed pressure urticaria and vibratory urticaria. Other inducible urticaria includes cholinergic, aquagenic, contact and exercise-induced urticaria. [7]In the acute case of spontaneous urticaria, the cause is often clear. Most frequently, investigations (complete blood counts, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), helicobacter test, autologous serum test, antinuclear autoantibodies, thyroid gland autoantibodies) are only carried out in chronic urticaria if the duration and seriousness of the illness warrant a search for the cause. [8]The first-line treatment of urticaria is by using non-sedating second-generation antihistamines (if the trigger is identified, it should, of course, be avoided). The second level of treatment encompasses increasing the dose of modern non-sedating second-generation antihistamines. The third level adds a leukotriene antagonist or systemic steroids if the situation is exacerbated. [9]Because descriptive studies of urticaria are rarely reported from Saudi Arabia, our study focuses on the clinical patterns of urticaria and the medication used for urticaria patients.
2. Materials and Methods
- This study was conducted at the outpatient Department of Dermatology, Hera General Hospital, Makkah, Saudi Arabia. The ethical committee of Hera Hospital approved the study. We retrospectively reviewed 201 cases of patients who attended the clinic during the period 2008–2012. The following data were collected: demographic data, date of initial visit, frequency and distribution of the wheals, history of angioedema and itching, personal and family history of atopy, history of drug use and food allergy. Laboratory investigations included complete blood counts, ESR, CRP, and free T3, free T4 and thyroid-stimulating hormone (TSH). The treatment was non-sedating H1-antihistamines, sedating H1-antihistamines, H2-antihistamines and systemic steroids. Data were analyzed by conducting Chi-square tests and t-tests, using SPSS software. The results were considered to be significant at a p-value < 0.05.
3. Result
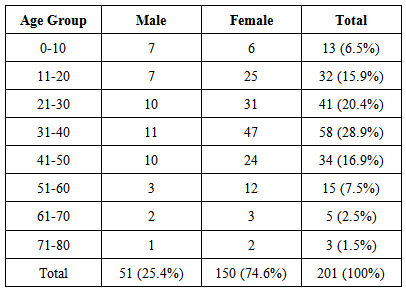
- The total number of patients (new and follow-up) who visited the dermatology clinic was 52,917 during 2008–2012. Urticaria was the diagnosis in 201 patients; 74.6% were women. The prevalence of urticaria among patients who attended the dermatology clinic was 0.4%.Their mean age was 32.9 years with a range of 1–76 years. Most urticaria patients (66.2%) were between 21 and 50 years. Table 1 presents the relation between the age group and sex of patients.
|
|
4. Discussion
- The aim of this study was to assess the clinical patterns of urticaria among patients at Hera General Hospital in Makkah, Saudi Arabia and to identify the medication used for urticaria patients. The prevalence of urticaria in our sample was found to be 0.4%, with the rate of chronic spontaneous urticaria 0.1%. [5, 10, 11]Urticaria tends to occur more frequently in children and in women between the ages of 30 to 60 years [12], although the chronic type is less common in children. In this study, we found that 72% of patients were aged between 20 to 50 years, while only 3.4% of patients with chronic spontaneous urticaria were between 0 and 10 years.We found a significantly higher incidence of urticaria in women compared with other studies. [13, 14] One possible explanation could be that 35–40% of autoimmune chronic urticaria occurs in women, which have a higher incidence of autoimmune diseases. [15]In total, 40.3% of our patients had acute spontaneous urticaria, which is more than a study conducted in Qatar (34.9%), [16] but comparable with other. [5] This finding could be explained by the fact that our patients received their treatment in outpatient services rather than in an emergency department. Chronic spontaneous urticaria occurred in 44.3% of cases, which was comparable with the study in Qatar (50.1%), [16] but lower than another study conducted in Thailand (75%). [13] The rates of physical urticaria, cold contact urticaria and delay pressure urticaria were also comparable with those of other studies. [13, 17]The prevalence of aquagenic urticaria, which occurred in 1% of our patients, was also similar to another study. [14] In Riyadh city in Saudi Arabia, the prevalence of bronchial asthma and allergic rhinitis is 11.4% and 12.7% compared with 15.5% and 4.2% in Madinah city, respectively. [18, 19] In our study, the personal history of bronchial asthma, allergic rhinitis and allergic conjunctivitis in patients with urticaria was 18.7%, 13.6% and 6.1%, respectively. These data imply no direct relationship between atopic diseases and urticaria, as the disease is prominent in Saudi Arabia.For chronic spontaneous urticaria, when we compared our patients with a history of bronchial asthma, we found that the relation is stronger in our study than that in the Thailand study (4.4%), while allergic rhinitis was less prevalent than ours in the same study (20%). [13]Altogether 25.4% of patients with urticaria had a food allergy in our study, which is more than that in other studies (range 16–19.7%). [13, 14] These variations could be related to the types of food eaten by different populations.In total, 19.7% of our patients had angioedema, which was lower than that found in other studies (30–40%). [13, 20, 21]We found that most patients had positive laboratory findings such as an increase in ESR, which was higher with chronic urticaria, but no clinical relevance or causes of urticaria could be identified.Combinations of first- and second-generation antihistamines and of an H2 antireceptor antihistamine with a first- or second-generation antihistamine were still used to treat chronic idiopathic urticaria in most of our patients. [22]Glucocorticosteroid treatment may be appropriate when antihistamines are ineffective. [23] These agents are helpful for controlling the inflammatory cell influx that can potentiate urticaria by the secondary release of histamine-releasing factors and cytokines. Managing physicians should explain the potential side effects associated with glucocorticosteroids. Recent guidelines recommend first-line symptomatic treatment of regular-dosed non-sedative antihistamines, followed by non-sedative antihistamines in high doses, which is not applicable in our practice. [24] Sedating antihistamines and systemic steroids, which can be considered to be obsolete, are still used by a meaningful number of physicians.Interestingly, the group of physicians who stated their familiarity with these guidelines were less likely to use sedating antihistamines and systemic steroids as a first- or second-line treatment, indicating that guideline recommendations may improve the quality of care. [25]
5. Conclusions
- The real-life therapeutic management of urticaria in daily practice is only partly in accordance with recent guidelines. The results of this study suggest that awareness of such guidelines may lead to an improvement in quality of care for urticaria patients.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML