-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Journal of Health Science
p-ISSN: 2166-5966 e-ISSN: 2166-5990
2015; 5(3A): 2-5
doi:10.5923/s.health.201501.02
Lichen Planus Pigmentosus Inversus
Iqbal A. Bukhari1, Fatmah Al Bader1, Abdulaziz Al Zahrani2
1Dermatology Department, College of Medicine, University of Dammam and King, Fahd Hospital of the University, Dammam, Saudi Arabia
2Internal Medicine Department, King Abdulaziz Hospital, Al Hassa, Saudi Arabia
Correspondence to: Iqbal A. Bukhari, Dermatology Department, College of Medicine, University of Dammam and King, Fahd Hospital of the University, Dammam, Saudi Arabia.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
Lichen planus pigmentosus inversus (LPPI) is a rare variant of lichen planus (LP) that presents as brown macules, papules, or reticulated hyperpigmentation in the the flexuaral and intertriginous areas. The lesions are usually asymptomatic. The differential diagnosis of LPPI includes ashy dermatosis, mycosis fungoides, occupational dermatoses and drug induced dermatoses. There is no specific treatment available for LPPI. Dermatologists should be familiar with this uncommon variant of LPP. As far as we know, there have been 27 cases reported internationally. In this report, we would like to present four more cases of this rare disorder in Arabic patients for the first time with a review of the literature.
Keywords: Lichen planus, Papulosquamous, Flexural, Lichenoid eruptions, Pigmentation
Cite this paper: Iqbal A. Bukhari, Fatmah Al Bader, Abdulaziz Al Zahrani, Lichen Planus Pigmentosus Inversus, Journal of Health Science, Vol. 5 No. 3A, 2015, pp. 2-5. doi: 10.5923/s.health.201501.02.
1. Introduction
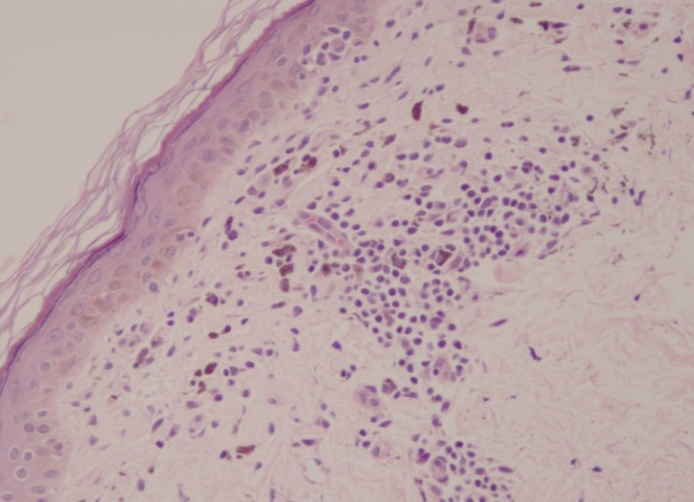
- Lichen planus pigmentosus inversus (LPPI) is a rare variant of lichen planus that affects flexuaral areas of the body. Approximately 27 cases are reported in the medical literature worldwide. Its pathogenesis is related to a T lymphocyte-mediated, cytotoxic activity against basal keratinocytes. [1, 2] It is characterized by asymptomatic hyperpigmented well defined macules located at the intertriginous areas, particularly axillae and groins. Mucosae, scalp, and palmoplantar areas are not affected by the disease. [2-4] Histologically, there is lichen planus pattern in regression, with slight hyperkeratosis and hypergranulosis and may be atrophic epidermis. [1-4]
2. The Case
- A 53-year-old Arabic female patient presented with asymptomatic brown macules in the axillary, submammary and inguinal areas associated with mild itching of 4 months duration. She denied the appearance of other cutaneous lesions or the use of any medications. On examination of the skin there was multiple dark brown flat macules and patches which were sharply demarcated smooth surfaced measuring 5 millimeters to 5 centimeters in diameter. There was no atrophy. Nails, scalp and mucus membranes were free of lesions. Systemic examination did not reveal any abnormalities. Initially, our differential diagnosis was discoid lupus erythrematosus, lichen planus pigmentosus, ashy dermatosis, fixed drug eruption, doweling-degos syndrome and post inflammatory hyperpigmentation. Laboratory tests including complete blood count, erythrocyte sedimentation rate, liver function tests, renal function tests, lipid profile, hepatitis serology, antinuclear antibodies, antidouble stranded DNA and urine analysis were within normal, skin punch biopsies were taken from the left axilla and inner right thigh which revealed thinned out flattened epidermis, basal cell liquefaction, pigmentary incontinence and dermal band-like and perivascular mononuclear inflammatory cell infiltrate. So our final diagnosis was lichen planus pigmentosus inversus. She was started on betamethasone valerate cream for 12 weeks with no improvement or worsening in the condition.
3. Case 2
- A 54-year-old Arabic female presented with hyperpigmented, non-pruritic macules and patches in the axillary and inguinal areas for 8 months. No other physical abnormalities were found. Complete blood investigations were within normal. Biopsy specimen from the lesion revealed similar pathological changes as in case 1, except for a more prominent lymphocyte infiltration in a band-like pattern in the upper dermis. So our final diagnosis was lichen planus pigmentosus inversus. Similarly she was started on betamethasone valerate cream for 12 weeks with no improvement or worsening in the condition.
4. Case 3
- A 49-year-old Arabic female presented to our dermatology clinic with brownish-black patches in the antecubital, neck flexure, submammary, axillary and inguinal areas for more than 2 years. She had mild pruritus. She had not received any prior treatment. There were no other skin and mucous membrane abnormalities. Complete blood investigations were within normal. The pathological changes were identical to those found in cases 1 and 2 and a final diagnosis of lichen planus pigmentosus inversus was given. She was started on mild topical steroid and bleaching agent for 8 weeks with no change in the condition so she decide to stop the treatment and be observed every 12 weeks.
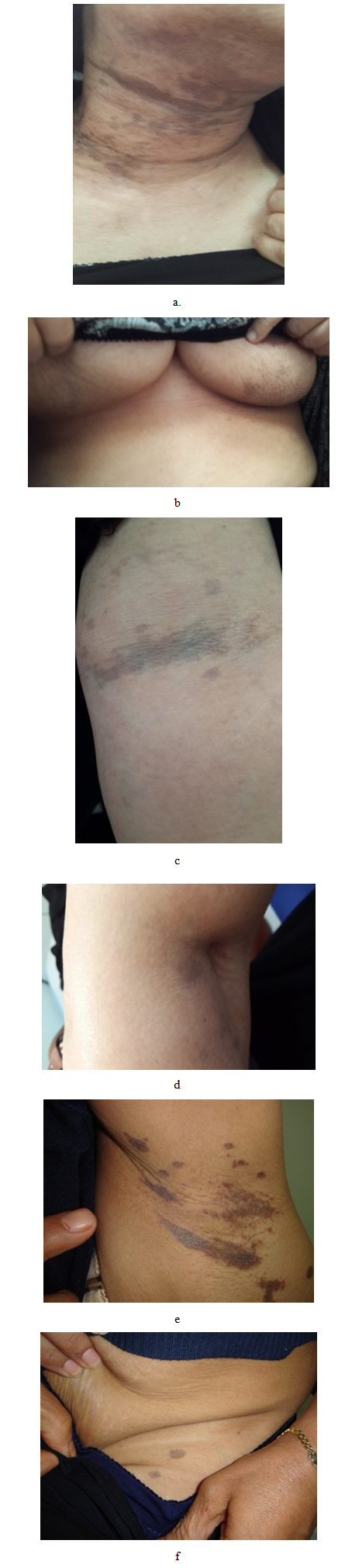 | Figure 1. Dark brown macules and patches in the a. neck, b. submammary area, c. antecubital, d. popliteal, e. axillary areas and f. groin |
5. Case 4
- A 47-year-old Arabic female presented with hyperpigmented, non-pruritic macules and patches in the neck flexure and the forehead since 5 years. There were no other skin and mucous membrane abnormalities. Routine laboratory tests were within normal values. The pathological changes were consistent with lichen planus pigmentosus inversus. She was started on betamethasone valerate cream for 10 weeks with no improvement or worsening in the condition.
6. Discussion
- LPP-inversus is a rare variant of lichen planus (LP) that presents as dark-brown hyperpigmented macules and patches predominantly located in the flexural areas and skin folds with slight pruritus. The axillae and groin seem to be the most commonly affected areas and tend to be bilateral in most cases. Other skin folds such as the neck, [6, 7] abdomen, [7] antecubital and popliteal areas, [6-10] submammary, [6, 7, 11] inner wrist, [1] and auricular sulci. [12] have been also involved. Most commonly, the macules and patches occur in multiple areas with no abnormalities of nail, hair and mucous membranes. There has been 27 reported cases in the medical literature. [6-18] Out of the 27 cases, 63% were more than 50 years old with almost equal sex distribution and the duration of the disease was within 6 months in 70% of the patients. On the contrary, our patients were Arabic females above the age of 47 years. The affected sites included axillary, submammary, inguinal, antecubital, neck flexure associated with mild itching in one case. The duration of the disease ranged between 4 months to 5 years.Reported biopsy findings are similar, showing an orthokeratotic, atrophic epidermis with lichenoid inflammation composed of lymphocytes and histiocytes. There is prominent pigmentary incontinence and melanophages in the upper dermis. The pathological features are in accordance with those in LPP. In our patients biopsy finding were similar to the reported findings. The cause and mechanism of LPPI is unclear. Pock et al. [11] hypothesized that an intensive lichenoid reaction could be occurring earlier than the compensatory increased proliferation of keratinocytes as in typical lichen planus with rapid transformation of papules into brown macules. Other studies postulated that T-cell and Langerhans cell-mediated immune responses also play a vital role in the pathogenesis of the disease. [9] However, there is no reasonable explanation for the isolated or exclusive distribution of hyperpigmented lesions in the intertriginous areas. Ohshima et al. [7] suggested that Koebner’s phenomenon may be operative in the etiology of LPPI, such as external mechanical stimuli to intertriginous areas. The differential diagnosis of LPPI include LPP, [19] and LP actinicus, [7] both of which affect dark-skinned races but produce lesions that are usually located in the sun-exposed areas. Besides, erythema dyschromicum perstans (ashy dermatosis), post-inflammatory hyperpigmentation, figurate erythema and fixed drug eruption should be considered. Treatment of LPPI include topical [6, 7, 14] and oral [8, 16, 17] steroids and topical tacrolimus. [14] In a few cases, the lesions improved or disappeared spontaneously after several months [6, 9, 16] Among two Japanese patients, discontinuation of wearing tight underclothes resulted in disappearance of the lesions. [17] In summary, in this report we are presenting four additional cases of LPPI in four Arabian females with minimum age of 47 years. The sites affected were mainly axillary, inguinal, submammary and neck flexures. There was no associated medical conditions. Response to treatment with topical steroids and bleaching agents was not satisfactory. The pateints are still followed up in our clinic.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML