-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2024; 12(1): 1-8
doi:10.5923/j.surgery.20241201.01
Received: Mar. 5, 2024; Accepted: Apr. 1, 2024; Published: Apr. 10, 2024

Gastric Volvulus in Adulthood About 2 Observations. Literature Review
M. Habarek, A. Bentabet, S. Merzouki, S. Ait Hamadouche, A. Matmar, A. Aissat
Department of General Surgery Tizi Ouzou, Teaching Hospital, Faculty of Medicine, University Mouloud Mammeri of Tizi Ouzou Algeria, Algeria
Correspondence to: M. Habarek, Department of General Surgery Tizi Ouzou, Teaching Hospital, Faculty of Medicine, University Mouloud Mammeri of Tizi Ouzou Algeria, Algeria.
| Email: |  |
Copyright © 2024 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Gastric volvulus (GV) is a rare clinical entity that is difficult to diagnose and can be fatal in the acute scenario. It is an uncommon disorder and can present either in the acute or chronic setting with variable symptoms. In adults, G.V. is a diagnostic and therapeutic emergency that can lead in acute forms to strangulation with a risk of ischemia and gastric necrosis. The etiology is dominated by hiatus hernia, while the main contributing factor is ligament laxity. The diagnosis is suspected on the chest x-ray while standing in front of the presence of an intrathoracic hydro-aeric level. The CT scan is a reliable examination and makes it possible to make the diagnosis of G.V., to draw up the thoracic lesion assessment and finally to study the vitality of the stomach. The aim of this study is to report two new observations of gastric volvulus (GV) in adults and to review the literature. Methods: For 20 years, two adult patients were carriers of G.V. one of which was unrecognized, until the onset of a complication (posterior perforation of the stomach). After a light medical preparation, the surgical indication was made. The intervention is carried out by a median umbilical laparotomy. The surgical procedures performed were: gastric detorsion, suture of the posterior gastric perforation and closure of the hiatus orifice by bringing the two diaphragmatic pillars together for the first case, and reintroducing these digestive structures intra-abdominally, and construction of a posterior Toupet-type hemi-valve after release of the large gastric tuberosity for the second case. Results: All our patients were symptomatic. They presented with vomiting and chest/epigastric pain. Computed tomography confirmed the existence of gastric volvulus. Average operating time was 173 minutes [150 – 195mn] and average hospital length of stay was 10 days [8 – 12days]. There were no complications and both patients were pleased with their results. Conclusion: Gastric volvulus is a diagnostic and therapeutic emergency whatever its form. The diagnosis of G.V. must be evoked in the face of digestive, respiratory or mixed symptoms and thus give the indication for surgery at the appropriate time.
Keywords: Stomach, Volvulus, Hernia, Diagnostic, Treatment
Cite this paper: M. Habarek, A. Bentabet, S. Merzouki, S. Ait Hamadouche, A. Matmar, A. Aissat, Gastric Volvulus in Adulthood About 2 Observations. Literature Review, International Journal of Surgical Research, Vol. 12 No. 1, 2024, pp. 1-8. doi: 10.5923/j.surgery.20241201.01.
Article Outline
1. Introduction
- Gastric volvulus (G.V) is defined as an abnormal rotation greater than 180 ° of all or part of the stomach around one of its axes, vertical or horizontal [1–5]. Taking into account the axis of rotation, we will differentiate between organo-axial volvulus and mesenterico-axial volvulus. It is a rare disease, often underdiagnosed and unrecognized, which can lead to serious complications such as upper digestive obstruction but especially strangulation with ischemia and necrosis of the stomach [5]. GV thus constitutes a diagnostic and therapeutic emergency [5]. Gastric volvulus was first described by Ambroise Paré in 1957 in a patient with a traumatic diaphragmatic rupture. It was not until the 19th century that this pathology began to be clearly individualized, in particular thanks to the work of Berti et al. [6]. At the beginning of the 20th century, several definitions were proposed based on the angle of rotation of the stomach and on etiological factors [7]. It was not until Hilleman's work in 1955 [8] that the most complete definition of gastric volvulus emerged and is still in use to this day. This condition is most often favored by a defect in the gastric fixation ligaments. The ligament abnormality may be either primary or secondary to other congenital malformations, the most common of which is herniation of the diaphragmatic domes [2,3]. The clinical symptoms are often atypical. Abdominal tomodensitometry and oeso-gastro-duodenal transit, confirm the diagnosis. The treatment of choice remains surgical. The aim of this work was to report two cases of gastric volvulus in adults and to review the literature.
2. Material and Methods
- Two patients were treated for gastric volvulus in the General Surgery Department of Tizi Ouzou University Hospital, Algeria over a period of 20 years from October 2003 to December 2023. The first patient was 55-year-old women had a clinical syndrome of acute perforated gastric volvulus. The second patient was 33-year-old woman with acute painful abdominal syndrome, early vomiting and cessation of materials and gas. In both cases the diagnosis was made on computed tomography scan, which showed gastric volvulus and a hiatus hernia. The clinical signs have been noted. Therapeutic methods and short- and long-term results were noted. The surgical indication and the choice of the type of surgical treatment, on the basis of the immediate results are also under discussion.
3. Results
- All our patients were symptomatic. In the first observation, the patient consulted for acute epigastralgia on sudden onset, associated with liquid vomiting and an arrest of digestive transit. In his antecedents, we found a notion of undocumented epigastralgia, hypertension under treatment and stroke 2 months ago. On physical examination, we noted a fairly good general condition, a temperature at 38.8°C, a tachycardia at 140 beats / min, a blood pressure of 140/90 mm Hg, a tender abdomen as a whole with a contracture generalized abdominal, an empty rectal bulb. The rest of the exam was unremarkable. The nasogastric tube could not be inserted. Biologically, a predominantly neutrophilic hyperleukocytosis was noted at 25170 leucocytes / mm3. The prothrombin (PT) level was 65%. Frontal radiography of the abdomen without preparation (ASP) and telethorax (TLT), demonstrated an interhepato-diaphragmatic gas crescent, hydro-aeric levels in the left hypochondrium, diffuse grayness, absence of digestive gas in the rest of the abdomen and a slight deviation of the heart silhouette to the right (Figure 1).
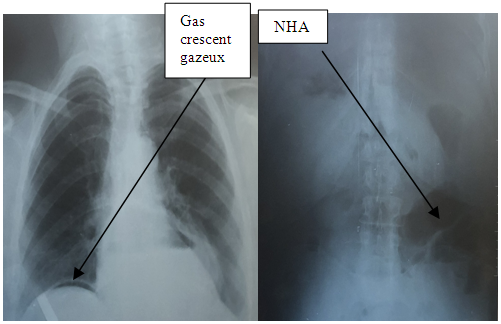 | Figure 1. Inter-hepato-diaphragmatic gas crescent, air fluid level in the left hypochondrium, diffuse grayness |
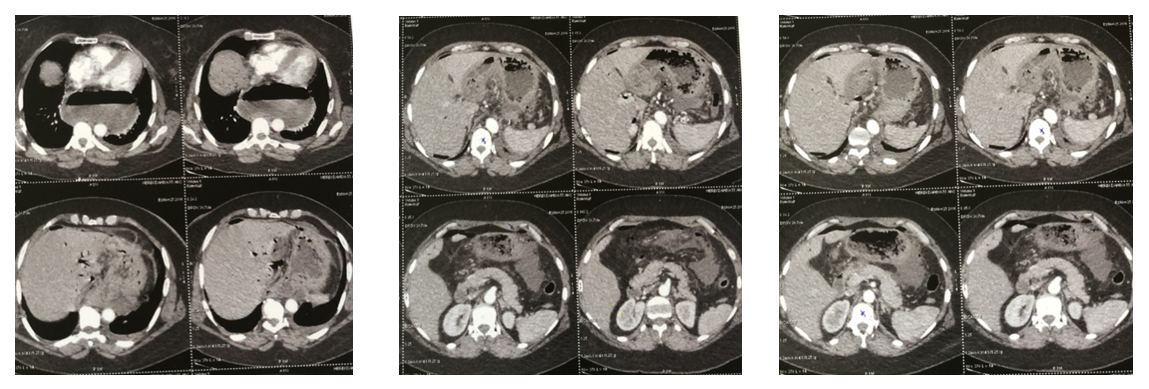 | Figure 2. Computed tomography: Gastric volvulus with pneumoperitoneum associated with fluid effusion, presence of a large hiatus hernia and parietal pneumatosis gastric |
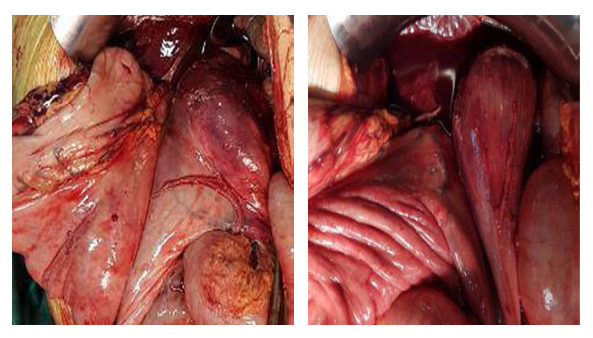 | Figure 3. Operative view showing gastric volvulus organo-axial |
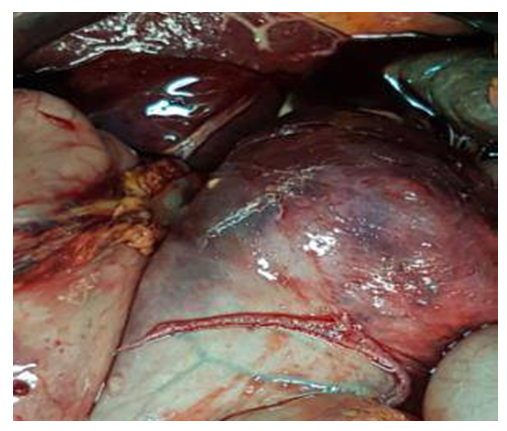 | Figure 4. Operative view showing ischemic necrosis of the stomach |
 | Figure 5. X-ray of the lungs: large gastric air bag |
 | Figure 6. Abdomen without preparation: hydro aeric level |
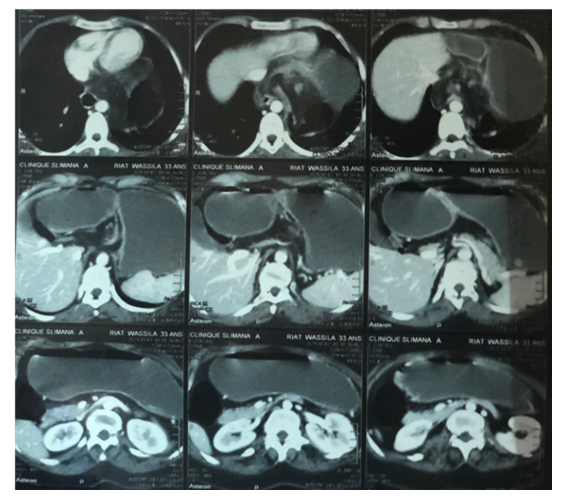 | Figure 7. Computed tomography confirmed the existence of gastric volvulus within a hiatus hernia without signs of ischemia gastric parietal |
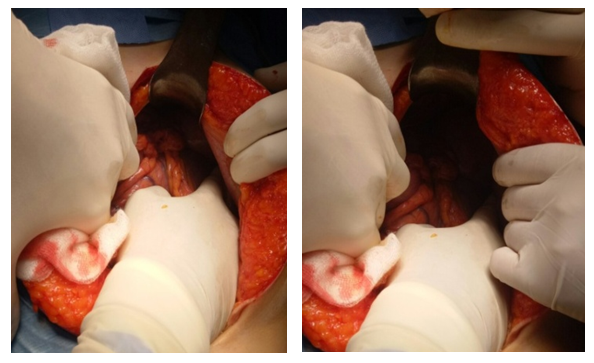 | Figure 8. Operative view showing gastric volvulus mesenterico-axial |
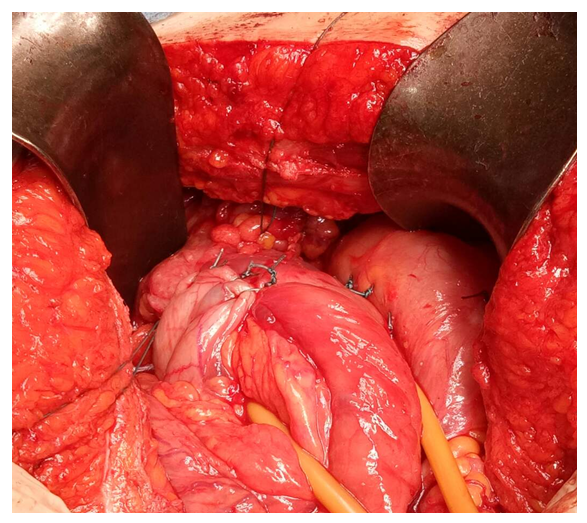 | Figure 9. Operative view showing the Nissen fundoplication |
4. Discussion
- Gastric volvulus is defined by an abnormal rotation of the whole or part of the stomach with respect to one of its axes, thus creating the conditions for a high occlusion with gastric dilation and risk of strangulation. From 1985 to the 2000s, 757 cases of gastric volvulus were published worldwide. The largest series included 44 cases [9]. In our institution, we have collected only two cases over the past 20 years, which testifies to the rarity of this entity. Gastric volvulus is a little-known surgical emergency. This condition is especially the prerogative of elderly subjects with a peak frequency around the age of fifty [10] as in our two observations. The two patients in this work, aged 33 to 55, had gastric volvulus confirmed by the operative findings and the absence of thoracoabdominal trauma that could suggest a diaphragmatic rupture. Cases of young adults have been reported in which the etiopathogenesis was dominated by traumatic diaphragmatic lesions [11,12]. Gastric volvulus also affects children, accounting for 45% of published cases and whose etiopathogenesis is dominated by congenital diaphragmatic abnormalities or rarely asplenia [13,14]. Regarding sex, there does not seem to be any predilection [9], however, a slight female predominance has been reported by some authors [10,15].Several anatomopathological classifications have been proposed, the most complete of which is that proposed by Von Haberer and Singleton modified by Carter in 1978 [16]. It takes into account respectively the axis of rotation, the extent of the organ involved in the rotation, the direction of rotation and finally the cause of gastric volvulus.Four anatomical forms of gastric torsion along the axis of rotation have been reported, two of which are the main ones. In the first, called organoaxial, initially described by Payer in 1909 [17], the rotation of the stomach takes place around a longitudinal axis passing through the cardia and the pylorus so that the greater curvature is found at the top, and the posterior face of the stomach is then placed in front as shown by our 1st observation (figure 10). This is the most common form, accounting for about 60% of cases [11]. It often occurs in a paraesophageal or diaphragmatic hiatus hernia and is frequently complicated by strangulation [18,19].
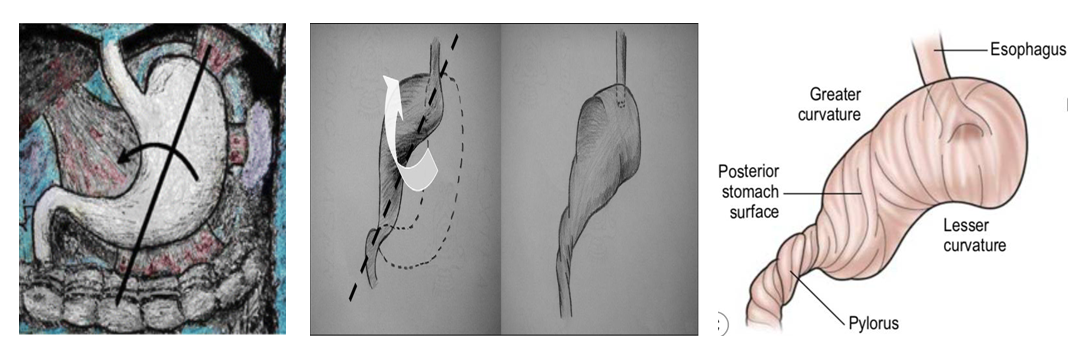 | Figure 10. Organo-axial gastricvolvulus |
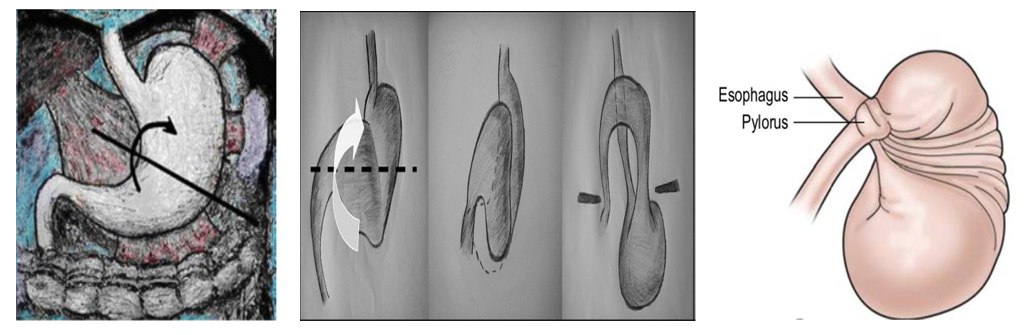 | Figure 11. Mesenterico-axial gastric volvulus |
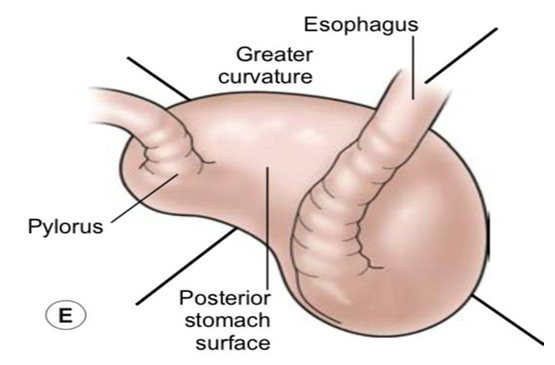 | Figure 12. Mixed volvulus |
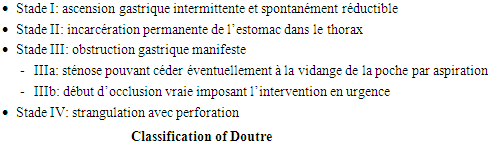 Vascular damage can range from simple mucosal venous congestion with sheet hemorrhage, to ischemia of the wall with necrosis and perforation. These consequences are especially the prerogative of acute intrathoracic gastric volvulus with strangulation through a diaphragmatic opening. Thanks to the blood supply to the stomach, necrosis is only partial. On the other hand, necrosis is rare in cases of pure intra-abdominal gastric volvulus, the ischemic lesions of which are essentially inherent in gastric distension which would lead to a defect in parietal capillary perfusion. In chronic volvulus, repeated ischemia often involves the neck area of neck, which may be the site of an ulcer that may bleed.Ascension of the stomach into the thorax can lead to cardiac compression with rhythm disturbances such as alternating QRS [27], syncope [28] and restrictive respiratory syndrome.Due to the multiplicity of clinical signs, their nonspecific nature and the rarity of LV in adults, the diagnosis of LV cannot be based on clinical alone and requires imaging tests. On the images without preparation (the chest x-ray, the abdomen without preparation) a LV can result in the presence of intra-thoracic hydro-aeric levels at 2 interfaces of different height and retro cardiac [29] as in the 1st observation, a large air bubble in the right hypochondrium [11] as in the second observation or even the absence of a gastric air pocket. In addition, they make it possible to highlight a pneumoperitoneum in the event of perforation as in the 1st observation.Esogastroduodenal transit is the essential test for the diagnosis of gastric volvulus. It is performed in the absence of cardiorespiratory shock, peritonitis or mediastinitis where the surgical indication is not debatable. It makes it possible to study the reducibility of gastric volvulus, its position, its mesenterico-axial or organo-axial anatomical shape and the antropyloric evacuation of the contrast product [10,30,31]. False negatives are rare and can be explained by the intermittent nature of gastric volvulus.Computed Tomography is an examination of a great interest in the positive diagnosis, allowing both to recognize the torsion of the stomach, to eliminate another abdominal pathology (in particular a cecal volvulus in front of an image of massive gas distension of a structure digestion cavity of the left hypochondrium discovered on the abdomen images without preparation) and guide, depending on the severity of the clinical condition, a possible surgical procedure.Typical signs of a herniated stomach on a CT scan involve distension marked gastric hydro-aeric and a zone of tissue thickening, with vascular congestion, separating a purely aeric gastric contingent and another water contingent, which is crossed by the nasogastric tube, the course of which is well followed on the successive cut levels [23,32,33].Magnetic resonance imaging appears to provide the same benefits as computed tomography at a higher cost [32].Abdominal ultrasound is of no diagnostic value but helps to detect other associated pathologies.Gastroscopy is not of a great diagnostic interest but above all makes it possible to search for an etiology such as a hiatus hernia and to study the state of the gastric mucosa. It is contraindicated in the presence of signs of gastric necrosis or perforation. Unfortunately, this exploration is often incomplete due to gastric torsion which hinders the progression of the endoscope [30,34]. Some authors have reported a therapeutic interest in gastroscopy, which allows endoscopic detorsion or even endoscopic guidance of percutaneous gastropexy [30,35,36].The clinical symptoms depend mainly on the acute or chronic nature of the LV, the degree of gastric rotation and obstruction and the above or sub diaphragmatic site. The clinical picture is sometimes suggestive when it carries out a characteristic triad (triad of Borchardt [23,37,38]) associating a major epigastric pain with irradiations in the back and / or the hypochondrium or the left hemithorax, efforts of ineffective vomiting, absolute food intolerance with difficulty or impossibility of insertion of a gastric tube as in our 1st case. The concomitant presence of these 3 signs is found in 70% [39]. However, the clinical picture remains nonspecific, most often abdominal pain, occlusive syndrome… [23,29,38] As in our second case. In addition, in 5% of cases of acute gastric volvulus, a complication may reveal gastric volvulus. This complication may be digestive hemorrhage, peritonitis or extremely severe mediastinitis, heart rhythm disturbance or even myocardial infarction lesions on the electrocardiogram without enzymatic disturbance [13]. Exceptionally, tamponade [40] or retentional jaundice due to bile duct plication [41] may be indicative of gastric volvulus.Surgery is the treatment of choice for gastric volvulus. It is indicated, in particular in the event of general repercussions, of hyperalgesic pain syndrome, and of tomodensitometric signs of gastric parietal ischemia. The surgical procedure includes the reduction of the hernia after gastric emptying and the performance of a gastropexy and / or the cure of an associated lesion if the general condition of the patient allows it [23].Currently, laparoscopic surgery is used more and more. It makes it possible to make the diagnosis and treat the pathology [23,37,42].Devolvulation or gastropexy under endoscopic guidance is only conceivable in the absence of signs of gastric necrosis or perforation [30].As in our two observations, the prognosis is often excellent in the forms treated and operated on early.
Vascular damage can range from simple mucosal venous congestion with sheet hemorrhage, to ischemia of the wall with necrosis and perforation. These consequences are especially the prerogative of acute intrathoracic gastric volvulus with strangulation through a diaphragmatic opening. Thanks to the blood supply to the stomach, necrosis is only partial. On the other hand, necrosis is rare in cases of pure intra-abdominal gastric volvulus, the ischemic lesions of which are essentially inherent in gastric distension which would lead to a defect in parietal capillary perfusion. In chronic volvulus, repeated ischemia often involves the neck area of neck, which may be the site of an ulcer that may bleed.Ascension of the stomach into the thorax can lead to cardiac compression with rhythm disturbances such as alternating QRS [27], syncope [28] and restrictive respiratory syndrome.Due to the multiplicity of clinical signs, their nonspecific nature and the rarity of LV in adults, the diagnosis of LV cannot be based on clinical alone and requires imaging tests. On the images without preparation (the chest x-ray, the abdomen without preparation) a LV can result in the presence of intra-thoracic hydro-aeric levels at 2 interfaces of different height and retro cardiac [29] as in the 1st observation, a large air bubble in the right hypochondrium [11] as in the second observation or even the absence of a gastric air pocket. In addition, they make it possible to highlight a pneumoperitoneum in the event of perforation as in the 1st observation.Esogastroduodenal transit is the essential test for the diagnosis of gastric volvulus. It is performed in the absence of cardiorespiratory shock, peritonitis or mediastinitis where the surgical indication is not debatable. It makes it possible to study the reducibility of gastric volvulus, its position, its mesenterico-axial or organo-axial anatomical shape and the antropyloric evacuation of the contrast product [10,30,31]. False negatives are rare and can be explained by the intermittent nature of gastric volvulus.Computed Tomography is an examination of a great interest in the positive diagnosis, allowing both to recognize the torsion of the stomach, to eliminate another abdominal pathology (in particular a cecal volvulus in front of an image of massive gas distension of a structure digestion cavity of the left hypochondrium discovered on the abdomen images without preparation) and guide, depending on the severity of the clinical condition, a possible surgical procedure.Typical signs of a herniated stomach on a CT scan involve distension marked gastric hydro-aeric and a zone of tissue thickening, with vascular congestion, separating a purely aeric gastric contingent and another water contingent, which is crossed by the nasogastric tube, the course of which is well followed on the successive cut levels [23,32,33].Magnetic resonance imaging appears to provide the same benefits as computed tomography at a higher cost [32].Abdominal ultrasound is of no diagnostic value but helps to detect other associated pathologies.Gastroscopy is not of a great diagnostic interest but above all makes it possible to search for an etiology such as a hiatus hernia and to study the state of the gastric mucosa. It is contraindicated in the presence of signs of gastric necrosis or perforation. Unfortunately, this exploration is often incomplete due to gastric torsion which hinders the progression of the endoscope [30,34]. Some authors have reported a therapeutic interest in gastroscopy, which allows endoscopic detorsion or even endoscopic guidance of percutaneous gastropexy [30,35,36].The clinical symptoms depend mainly on the acute or chronic nature of the LV, the degree of gastric rotation and obstruction and the above or sub diaphragmatic site. The clinical picture is sometimes suggestive when it carries out a characteristic triad (triad of Borchardt [23,37,38]) associating a major epigastric pain with irradiations in the back and / or the hypochondrium or the left hemithorax, efforts of ineffective vomiting, absolute food intolerance with difficulty or impossibility of insertion of a gastric tube as in our 1st case. The concomitant presence of these 3 signs is found in 70% [39]. However, the clinical picture remains nonspecific, most often abdominal pain, occlusive syndrome… [23,29,38] As in our second case. In addition, in 5% of cases of acute gastric volvulus, a complication may reveal gastric volvulus. This complication may be digestive hemorrhage, peritonitis or extremely severe mediastinitis, heart rhythm disturbance or even myocardial infarction lesions on the electrocardiogram without enzymatic disturbance [13]. Exceptionally, tamponade [40] or retentional jaundice due to bile duct plication [41] may be indicative of gastric volvulus.Surgery is the treatment of choice for gastric volvulus. It is indicated, in particular in the event of general repercussions, of hyperalgesic pain syndrome, and of tomodensitometric signs of gastric parietal ischemia. The surgical procedure includes the reduction of the hernia after gastric emptying and the performance of a gastropexy and / or the cure of an associated lesion if the general condition of the patient allows it [23].Currently, laparoscopic surgery is used more and more. It makes it possible to make the diagnosis and treat the pathology [23,37,42].Devolvulation or gastropexy under endoscopic guidance is only conceivable in the absence of signs of gastric necrosis or perforation [30].As in our two observations, the prognosis is often excellent in the forms treated and operated on early.5. Conclusions
- Gastric volvulus is a rare condition, the course of which can be extremely serious. Computed tomography is the first-line imaging test when this pathology is suggested. It makes it possible to establish the thoracic lesion assessment and to study the vitality of the stomach. The treatment of choice remains surgical.
Study Limitation
- The Study had a limited sample size, because it’s a rare pathology.
Conflicts of Interest
- None of the authors have any conflicts of interest (financial or otherwise) to disclose.
Funding
- The authors received no financial support for the research, authorship, and/or publication of this article.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML