-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2022; 11(1): 1-5
doi:10.5923/j.surgery.20221101.01
Received: Feb. 28, 2022; Accepted: Mar. 11, 2022; Published: Mar. 24, 2022

Cryptorchidism: Diagnosis, Management and Outcomes at Albert Royer National Children’s Hospital Centre in Senegal
Papa Alassane Mbaye1, Ndeye Fatou Seck1, Ibrahima Bocar Wellé1, Souleymane Camara2, Lissoune Cissé1, Faty Balla Lo1, Florent Tshibwid A. Zeng1, Abdoulaye Fall1, Gabriel Ngom1
1Service of Pediatric Surgery, Albert Royer National Children’s Hospital Centre, Université Cheikh Anta Diop, Dakar, Code Postal, Senegal
2Service of Pediatric Surgery, Aristide Le Dantec University Teaching Hospital, Université Cheikh Anta Diop, Dakar, Code Postal, Senegal
Correspondence to: Papa Alassane Mbaye, Service of Pediatric Surgery, Albert Royer National Children’s Hospital Centre, Université Cheikh Anta Diop, Dakar, Code Postal, Senegal.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: Cryptorchidism is a common pathology in boys. The aim of our study is to report its diagnosis, management, and outcomes. Patients and Method: We conducted a 22-month study at the Albert Royer National Children’s Hospital Centre in Dakar, including patients treated in our pediatric surgery department. Results: Our study involved 63 patients. In 88.9% of cases, the parents initiated the consultation. Unilateral involvement was found in 76.2%, with a predominance on the left side (42.9%). In 61.8%, the undescended testis was palpable and associated abnormalities were found in 33.3% of cases. The mean age at surgery was 3.6 years (3 months – 13 years), with a median of 2 years. The inguinal position was noted in 87.2% and normal testicular volume was found in 66.7%. Patent vaginalis was reported in 26.9%, epididymo-testicular anomalies in 15.4%, and sufficient length of the spermatic pedicle in 89.7%. Single-stage orchidopexy was done in 95.2%, with dartos-pouch fixation in 93.3%. Over an average follow-up of 25 months, 44.4% of patients were lost to follow-up. No complications were found in 91.4%, while 5.7% of patients presented with vanishing testis and 2.9% with recurrence. Conclusion: In our settings, diagnosis of cryptorchidism is still delayed, and surgical treatment is made in all patients. The results are excellent, but many patients are still lost to follow-up. Long-term follow-up is imperative.
Keywords: Cryptorchidism, Undescended Testis, Outcomes, Senegal
Cite this paper: Papa Alassane Mbaye, Ndeye Fatou Seck, Ibrahima Bocar Wellé, Souleymane Camara, Lissoune Cissé, Faty Balla Lo, Florent Tshibwid A. Zeng, Abdoulaye Fall, Gabriel Ngom, Cryptorchidism: Diagnosis, Management and Outcomes at Albert Royer National Children’s Hospital Centre in Senegal, International Journal of Surgical Research, Vol. 11 No. 1, 2022, pp. 1-5. doi: 10.5923/j.surgery.20221101.01.
Article Outline
1. Introduction
- Cryptorchidism is the most common birth defect of the male reproductive system [1]. There are 3-5% of cases in full-term newborns compared to 20 to 30% in premature babies [2].The diagnosis is made after confirmation of the absence of testis in the scrotum during the clinical examination, either discovered in the delivery room by the gynecologist or the midwife, or by the parents or fortuitously during a school consultation. The testis can then be palpated at the level of the inguinal canal or not. In the latter case, ultrasound or better, magnetic resonance imaging (MRI) can help localize the nonpalpable testicle [3]. In recent decades, laparoscopy has become the gold standard for the diagnosis and management of non-palpable undescended testis [4]. However, in our centers, dartos-pouch orchidopexy by open surgery remains the most practiced technique [1,5-7].In our region, several studies have been conducted in recent years on this subject, evaluating its frequency in schools [5], its epidemiological, clinical, and therapeutic aspects [6,7], and finally, the contribution of laparoscopy in nonpalpable testis [7]. In sub-Saharan Africa, the diagnosis is generally late, resulting in a delay in management which jeopardizes the functional prognosis of the pathological gonad [1].The purpose of this study is to report the experience of the Albert Royer National Children’s Hospital Centre by studying the diagnostic, therapeutic, and especially evolutionary characteristics of cryptorchidism in our environment.
2. Patients and Method
- We conducted a retrospective cross-sectional descriptive study, which considered the periods from October 09, 2018, to April 01, 2019, and from November 27, 2019, to July 16, 2020, within the service of pediatric surgery of Albert Royer National Children’s Hospital Centre, in Dakar, Senegal.The patients included in our study are those whose diagnosis and management were both made in our service. Those whose care was provided in another hospital and/or whose medical records did not have sufficient information necessary for this study were excluded. Over the study period, 63 patients met the criteria.The data was collected from the patients' medical records as well as from the operating room report’s register. The various parameters studied were clinical, complementary investigations, management, and outcomes. The findings were encoded on a Microsoft Office 2016 Excel spreadsheet and analyzed with SPSS IBM software version 26.
3. Results
3.1. Diagnosis
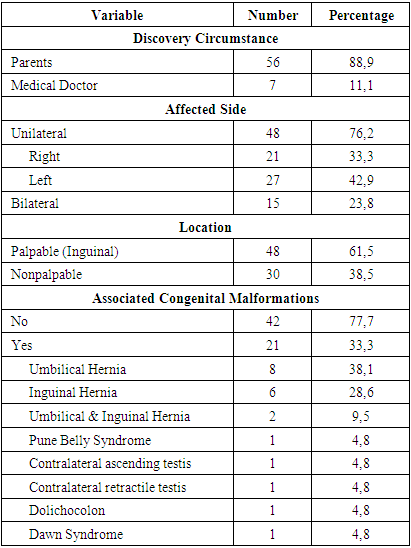
- The discovery was made by the parents in 56 of the 63 patients. Unilateral cryptorchidism was the most frequent with 51 of the 63 patients, with a predominance on the left in 27 patients. A total of 78 undescended testes were recorded in the 63 patients, of which 48 were palpable, all in the inguinal position. In 21 patients, congenital anomalies were associated. All of these clinical data are shown in Table 1.
|
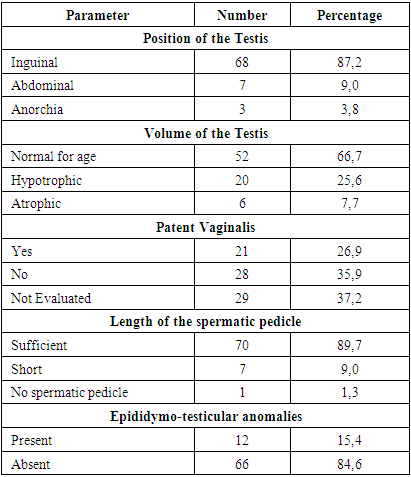
3.2. Treatment
- Among our patients, none received hormonal treatment. The surgery was performed on patients whose average age was 3.6 years, with extremes ranging from 3 months to 13 years and a median of 2 years. The different age groups are represented in Figure 1.
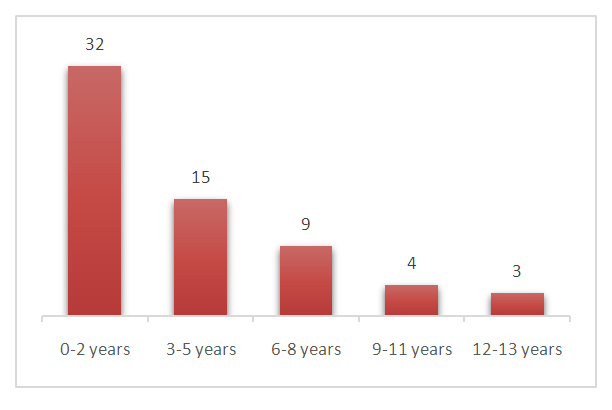 | Figure 1. Patients’ age at orchidopexy. Note the persisting important proportion above 2 years, with progressive decrement |
|
3.3. Outcomes
- In the short-term follow-up (1 month after orchidopexy), all patients had been reviewed, and no complications were reported.In the long-term follow-up, the average follow-up time was 25 months, with extremes of 16 to 38 months post orchidopexy. Of the 63 patients included, 28 (44.4%) were lost to follow-up. Of the remaining 35, 32 (91.4%) showed no particularity, two (5.7%) had vanishing testis, and one (2.9%) cryptorchidism recurrence.
4. Discussion
- Cryptorchidism is a congenital malformation; it is characterized by the absence of one or both testicles in the scrotum. It is a pathology whose diagnosis should be made in the delivery room, during the first examination of the newborn. However, in our series, it was mainly the parents who made the discovery, in 88.9% of cases. Our data are similar to those of other studies conducted in Sub-Saharan Africa, where parental discovery ranged from 66.4 to 76.4% [8,9]. Attention should be drawn to the quality of the clinical examination of the newborn in maternity wards, which will reduce the delay in diagnosis and improve the long-term functional outcome.Cryptorchidism occurs mostly unilaterally and the right side is particularly predominant because of later testicular descent compared to the left side. In our series, the left side was predominant, with 43% of cryptorchidism, which other studies have also reported, with a frequency ranging from 50 to 66.7% [10,11]. However, other authors have reported the generally observed trend with predominant right cryptorchidism representing between 36.4 and 66% [1,12,13]. These differences may be due to variability in recruitment. Bilateral cryptorchidism was noted in 24% in our series, which is within the reported frequency range of 9.5-30.3% [1,10-13].Within our study population, palpable undescended testicles accounted for 61.5%. This is within the range reported by other authors, with a frequency varying from 60.8 to 62% [8,12]. However, other authors have reported a much lower frequency, ranging from 27.6 to 34.5% [1,13]. These differences could be explained by two elements: the level of experience of the examiner and the lack of a preoperative examination, on the operating table, after induction of anesthesia. The muscle relaxation caused by the latter may promote easier palpation.Associated malformations are reported in varying proportions in the literature. In our series, cryptorchidism was associated with another malformation in 33.3% of cases. Among the malformations encountered, the umbilical hernia and the inguinal hernia were the most frequent, about 38 and 28.5% respectively. For other authors, the first associated malformation was the inguinal hernia, found in more than 80% of cases [1,8]. The umbilical hernia being clinically more detectable and the inguinal hernia not being systematically sought in our patients could explain our results. From where a well-provided interrogation and a complete clinical examination will make it possible to diagnose the associated clinically detectable abnormalities.The use of complementary examinations is not usual for undescended testes. In our series, only one patient benefited from an ultrasound that could not locate the nonpalpable testicle. In our department, the management protocol for nonpalpable undescended testis consists of performing an open surgical exploration or laparoscopy. This is related to the fact that current evidence indicates that ultrasound is not the examination of choice, locating the palpated testicle in only 18% of cases [14]. MRI would provide better precision, but its cost and unavailability make it not very usable in Sub-Saharan Africa, especially since its performance will not change the indication for surgery [15]. The gold standard is the use of laparoscopy, which apart from its sensitivity close to 100% in the location of the nonpalpable testis, allows the treatment [16,17]. In some studies, it was performed systematically [11,16,18] whereas in our case, only 3.2% of patients benefited from it. This could be explained on the one hand by the frequency of palpable testicles in our series and on the other hand by the lack of specialists in laparoscopy and the inaccessibility of laparoscopy in developing countries.In our series, no patient received medical treatment. Our treatment protocol does not include hormonal therapy. This is motivated by the fact that medical treatment is successful in 16 to 21% of cases [19] and in the long term, not to mention its cost for our populations. Currently, hormonal therapy is not recommended [15].Orchidopexy should ideally be performed between 6 and 18 months. This reduces the risk of subfertility and in the long term, the risk of malignancy [20]. In our study population, 49.1% of patients were treated after the age of 2 years. African studies report significant proportions of patients treated late, with 77.2% after 2 years [1] and 75.8% after 4 years [8]. Our study shows a younger age at surgery, however, efforts should be made to treat these patients within the ideal timeframe, involving midwives, doctors, and parents in early diagnosis.The inguinal approach was the most used in our series with 93.7%. Other African authors have reported its use for the entire sample [1,9,21]. This can be justified by the elements cited above, concerning the unavailability of laparoscopy in developing countries.The delay in management is responsible for testicular atrophy. In our study, its frequency was 6%, against 19% in an Egyptian study [22]. This difference could be attributable to the greater diagnostic delay in the second study. However, most other African studies have not consistently reported the presence of an atrophic testis discovered intraoperatively. Intraoperative confirmation of patent vaginalis was made in 27% of cases in our series. Other authors report it with a frequency ranging from 13 to 87% [23]. It should be noted that in our study, the presence of patent vaginalis was not evaluated in 37% of cases, this would explain the low frequency in our study. Epididymo-testicular abnormalities are frequently associated with cryptorchidism. In our series, they were noted in 15.9% of cases, which is in the interval of the various reported frequencies, ranging from 8 to 32% [21]. In addition to testicular atrophy, they would be the cause of subfertility [2,24].Dartos-pouch orchidopexy, a reliable technique allowing postoperative clinical monitoring of the treated testis, was used in 95% of our series, as with most authors, with a frequency ranging from 86.5 to 100% [1,8,9,12,21].The follow-up of patients who have undergone orchidopexy is crucial. In the short term, it evaluates the results of this delicate surgery. In our series, after an average follow-up of 25 months, 44.4% of patients were lost to follow-up. This percentage is high and reminds the need to explain to parents the need for medium and long-term monitoring, with the aim of evaluating the postoperative course. Of the 35 patients followed, 91.4% have a success, which is reported by other authors in 85 to 100% of cases [25]. Two cases of vanishing testis and one case of recurrence were reported. This further emphasizes the importance of the follow-up because these complications, often poorly reported by African studies, do exist.
5. Conclusions
- In our setting, cryptorchidism is still diagnosed late, at the instigation of the parents. Its treatment is resolutely surgical, by inguinal approach, laparoscopy being rarely used. The results are excellent, but many patients are still lost to follow-up. Long-term follow-up in adult patients to assess fertility and screen for malignancy is a moral and ethical imperative.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML