-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2021; 10(1): 1-8
doi:10.5923/j.surgery.20211001.01
Received: Aug. 31, 2021; Accepted: Sep. 15, 2021; Published: Sep. 26, 2021

Risk Factors and Rates of Cholecystectomy During 30-Day Hospital Readmission Following Bariatric Surgery
Amanda M. Marsh1, Joshua Parreco2, Kandace Kichler2, Sarah Yi1, Miguel Lopez-Viego1, 3, Jessica L. Buicko1, 3
1Florida Atlantic University Schmidt College of Medicine, Department of Surgery, Boca Raton, Florida, USA
2University of Miami Miller School of Medicine, Miami, Florida, USA
3Bethesda Memorial Hospital, Baptist Health System, Boynton Beach, Florida, USA
Correspondence to: Amanda M. Marsh, Florida Atlantic University Schmidt College of Medicine, Department of Surgery, Boca Raton, Florida, USA.
| Email: |  |
Copyright © 2021 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: Biliary disease is a well-established sequela of the rapid weight loss following bariatric surgery. With the increasing prevalence of obesity and the rise of bariatric surgery procedures being performed annually, quality metrics such as associated hospital readmission and related complications are of significant clinical interest. The aim of this study was to assess the rate of cholecystectomy performed during readmission within 30 days after bariatric surgery and to identify associated risk factors and comorbidities. Methods: The Nationwide Readmission Database from 2010-2015 was queried for patients who previously had bariatric surgery and underwent a cholecystectomy during hospital readmission. The primary outcome was non-elective readmission within 30 days. Multivariate logistic regression was used to determine the odds ratios (OR) for the outcomes of interest. Results: A total of 886,596 patients who had bariatric surgery were reviewed and of which, 5,390 patients (0.6%) had a cholecystectomy performed during 30-day hospital readmission. There were 1,240 patients (23.0%) who had a cholecystectomy performed at a different hospital. The majority of patients readmitted who underwent a cholecystectomy were female (84.5%) and had private insurance (65.7%). The comorbidities associated with the highest OR for cholecystectomy during readmission were metastatic cancer (OR 7.18, p<0.001), acquired immune deficiency syndrome (OR 5.0, p<0.001), chronic blood loss anemia (OR 2.11, p=0.007), diabetes with chronic complications (OR 1.86, p<0.001) and coagulopathy (OR 1.82, p<0.001). Patients ≥45 years of age, patients who underwent sleeve gastrectomy (OR 0.72, p<0.001) and patients with a CCI ≥2 (OR 0.83, p=0.002) were less likely to have a cholecystectomy during readmission. Conclusion: Less than 1% of patients who undergo bariatric surgery will develop symptomatic biliary disease requiring cholecystectomy during 30-day hospital readmission, even when accounting for readmissions across other hospitals. This study highlights those patients at higher risk for needing a cholecystectomy, however prophylactic cholecystectomy during bariatric surgery would not provide significant benefit or improve resource utilization.
Keywords: Bariatric surgery, Cholecystectomy, Hospital readmission, Risk factors, Obesity
Cite this paper: Amanda M. Marsh, Joshua Parreco, Kandace Kichler, Sarah Yi, Miguel Lopez-Viego, Jessica L. Buicko, Risk Factors and Rates of Cholecystectomy During 30-Day Hospital Readmission Following Bariatric Surgery, International Journal of Surgical Research, Vol. 10 No. 1, 2021, pp. 1-8. doi: 10.5923/j.surgery.20211001.01.
Article Outline
1. Introduction
- Symptomatic gallstone disease is a significant health problem affecting 10-15% of the adult population, making cholecystectomy one of the most commonly performed procedures in the United States [1-3]. Symptomatic gallstone disease is defined by symptoms of biliary colic or acute or chronic cholecystitis. Important risk factors for gallstone formation include ethnicity, genetics, advancing age and female gender. Other modifiable risk factors can lead to increased risk of gallstone formation such as obesity, metabolic syndrome, diabetes mellitus, dyslipidemia, rapid weight loss, fasting, sedentary lifestyle and certain medications [1,2,4]. The prevalence of obesity has increased significantly over the last decade, affecting more than one-third of the U.S. adult population (93.3 million people as of 2015-2016) [4,5]. Consistent with this trend, the incidence of bariatric surgery procedures also continues to rise. Bariatric surgery with rapid weight loss is associated with gallstone formation in 30-71% of patients, with up to 15% of patients experiencing symptomatic biliary sequelae after bariatric surgery which may require cholecystectomy [2,3]. The mechanism by which gallstones form after rapid weight loss includes biliary stasis from lower caloric intake and increased biliary saturation because of increased cholesterol mobilization. [6] The incidence of cholecystectomy is found to be highest within the first 6 months following bariatric surgery, specifically within the first 6 weeks when weight loss is the most profound [1-3]. Therefore, quality metrics such as associated hospital readmission and biliary complications has garnered significant clinical interest [4]. There has been considerable debate about performing prophylactic cholecystectomy concomitant with bariatric surgeries. This alternative has been studied but the results remain inconclusive. Conservative management with ursodiol prophylaxis to reduce stone formation and the potential need for subsequent cholecystectomy is also of clinical interest. The incidence and associated risk factors of cholecystectomy performed during post-bariatric surgery hospital readmission on a large national scale have yet to be identified. In order to improve patient outcomes as well as quality and cost of care, these clinical outcomes must be identified. The purpose of this study is to evaluate the incidence of cholecystectomy performed during readmission after bariatric surgery across the United States using the Nationwide Readmission Database and to identify risk factors that predict need for cholecystectomy during readmission.
2. Methods
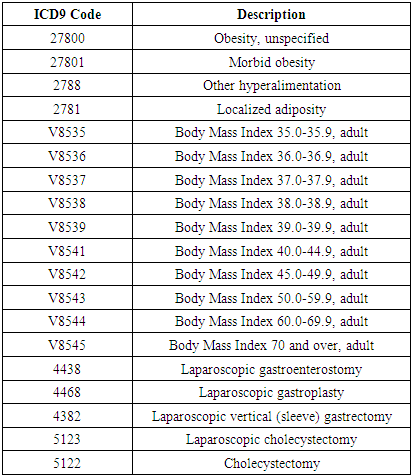
- The Nationwide Readmission Database (NRD) is an annual database released by the Agency for Healthcare Research and Quality as a part of the Healthcare Cost and Utilization Project (HCUP) [7]. The NRD is derived from the HCUP State Inpatient Databases, composed of 14 million admissions yearly across 22 states, representing 51.2% of the total United States population [7]. The NRD utilizes a unique identifier to track patients across admissions to different hospitals within a state. Data is provided for length of stay and time between admissions. In addition, this database takes into account transfers and same-day events by incorporating multiple records into one larger record, therefore discharges and admissions between different hospitals will be less likely to be counted as a readmission [8]. The 2010-2015 National Readmission Database was queried for all admissions with an International Classification of Diseases, 9th Revision (ICD-9) Clinical Modification diagnosis codes for unspecified obesity, morbid obesity, localized adiposity, other hyperalimentation and body mass index 35-70, as well as procedure codes for laparoscopic gastroenterostomy, laparoscopic gastroplasty, laparoscopic vertical sleeve gastrectomy, cholecystectomy and laparoscopic cholecystectomy (Appendix). The NRD was then queried for the first non-elective hospital readmission within 30 days after discharge from the hospital following bariatric surgery. The NRD assigns to each admission and readmission a principle ICD-9 diagnosis code, as well as an All Patient Refined Diagnosis Related Groups (APRDRG) code that more broadly categorizes the diagnosis. Readmission to the same or different hospital that bariatric services were provided by was tabulated from the database. Exclusion criteria included elective readmission within 30 days, death during initial admission, missing data for any patient, and readmission > 30 days after hospital discharge post-operatively from bariatric surgery. Independent predictors of readmission included in the analyses were age, gender, type of bariatric surgery, body mass index (BMI), insurance type, Charlson Comorbidity Index, and patient comorbidities. The Charlson Comorbidity Index (CCI) is a measurement of total comorbidity burden in a patient, reported as a score that can be converted to a 10-year survival rate. 10-year survival rate=0.983^(eCCIx0.9). Categorical variables were compared using chi-squared test. Statistical significance is defined by p-values < 0.05. Univariate binary logistic regression of all covariates for cholecystectomy on readmission post-bariatric surgery. Significant covariates were used to perform multivariate binary logistic regression. Odds ratios are reported with 95% confidence intervals. Statistical analysis was performed using IBM SPSS Statistics version 22 (International Business Machines Corp., Armonk, New York).
3. Results
3.1. Demographics for Patients Requiring Cholecystectomy Following Bariatric Surgery
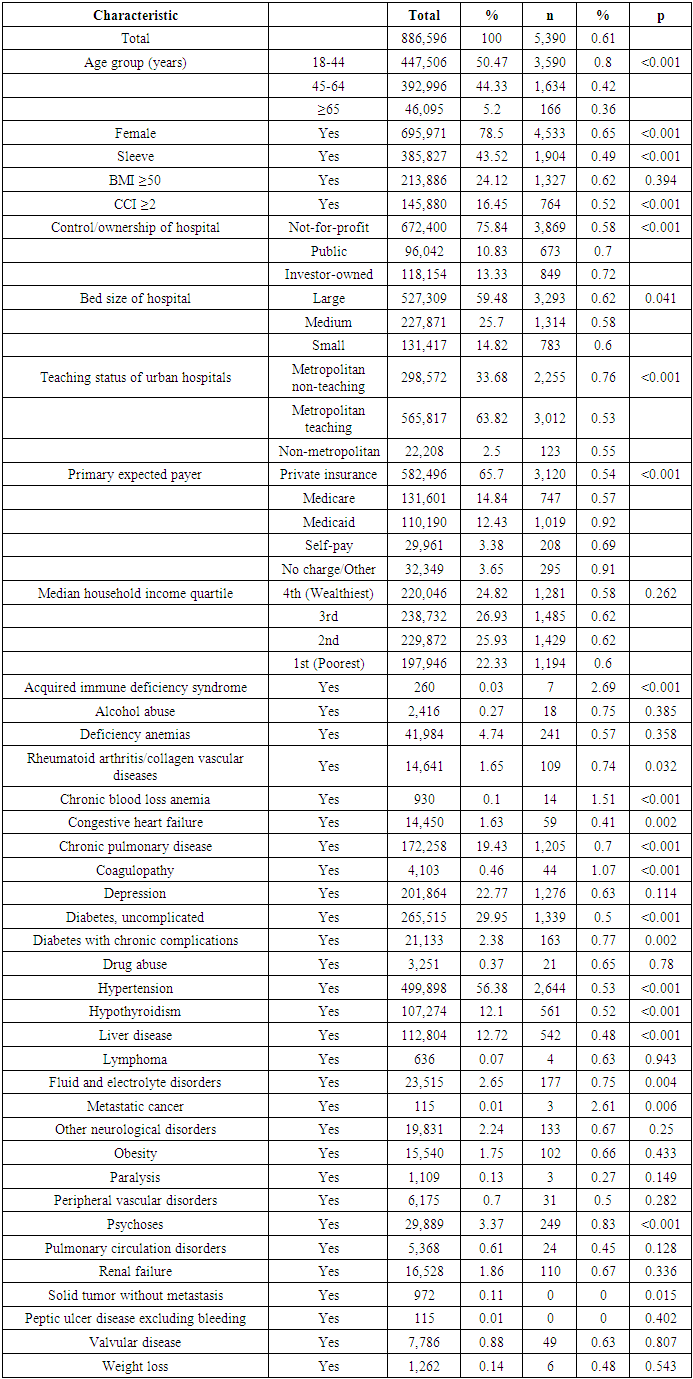
- During 2010 to 2015, a total of 886,596 patients underwent bariatric surgery, however 5,390 (0.6%) patients underwent cholecystectomy during 30-day hospital readmission following bariatric surgery. The majority of patients readmitted were female (84%) and between the ages of 18-64. A small portion of patients readmitted had a CCI ≥2 (14.1%). The most common comorbidities seen among patients requiring cholecystectomy included hypertension (49.1%), uncomplicated diabetes (24.8%), depression (23.7%), chronic pulmonary disease (22.4%), hypothyroidism (10.4%) and liver disease (10.1%). The majority of hospitals providing surgical services were not-for-profit, considered large by total beds available, and were considered metropolitan teaching hospitals. The mean household income for patients was evenly distributed between the 1st (poorest) and 4th (wealthiest) quartiles. Most patients were insured with either private insurance (65.7%), Medicare (14.8%) or Medicaid (12.4%).
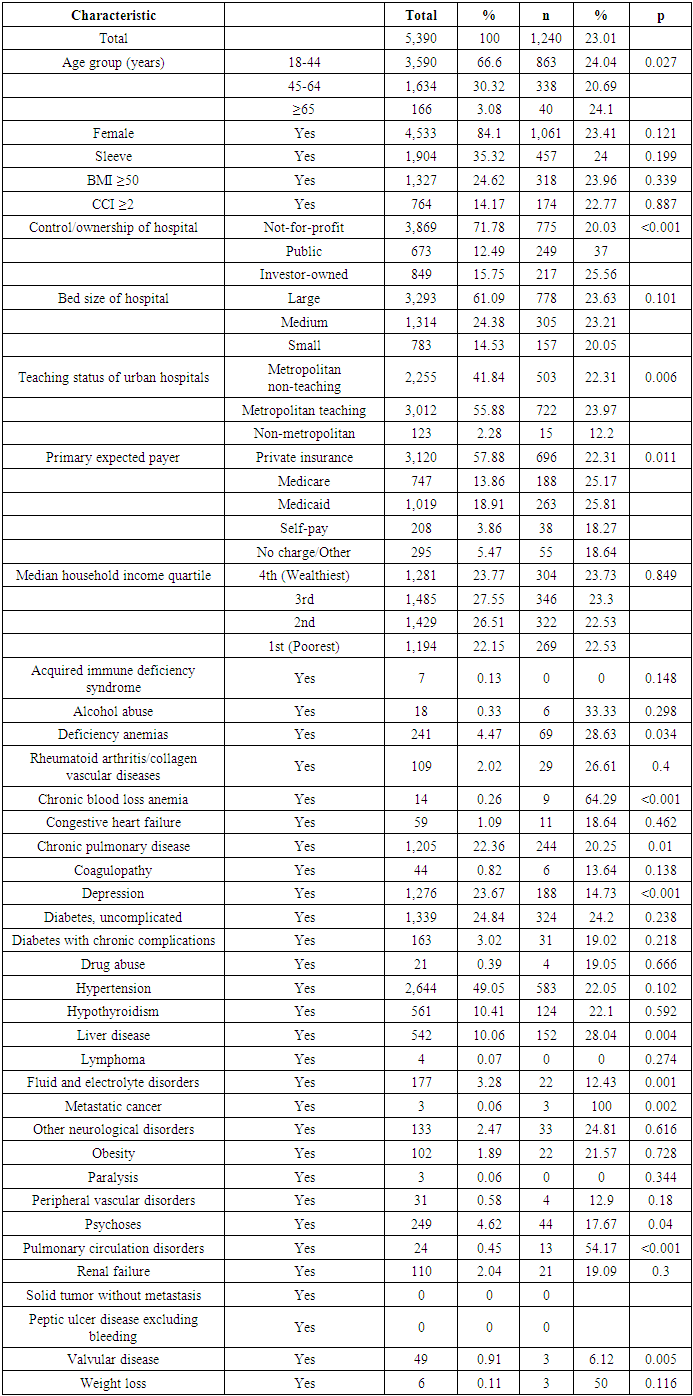
3.2. Demographics for Patients Requiring Cholecystectomy at Different Hospitals
- In total, 5,390 patients underwent cholecystectomy during 30-day hospital readmission for symptomatic biliary disease following bariatric surgery. However, 1,240 patients (23.0%) were readmitted at different hospitals from where the initial bariatric surgery was performed. There was no significant difference in gender or CCI ≥2 for patients seen at different hospitals (85.6% and 14.0%). The majority of patients seen at other hospitals for cholecystectomy were between the ages 18-44 (69.6%). Similarly, the most common comorbidities seen at different hospitals were hypertension (47.0%), uncomplicated diabetes (26.1%), chronic pulmonary disease (19.7%), depression (15.2%), liver disease (12.3%) and hypothyroidism (10.0%). The majority of these hospitals providing surgical services were also not-for-profit, considered large by total beds available, and were considered metropolitan teaching hospitals. The mean household income for patients was evenly distributed between the 1st (poorest) and 4th (wealthiest) quartiles. Most patients were insured with either private insurance (56.1%), Medicare (15.2%) or Medicaid (21.2%).
3.3. Adjusted Analysis
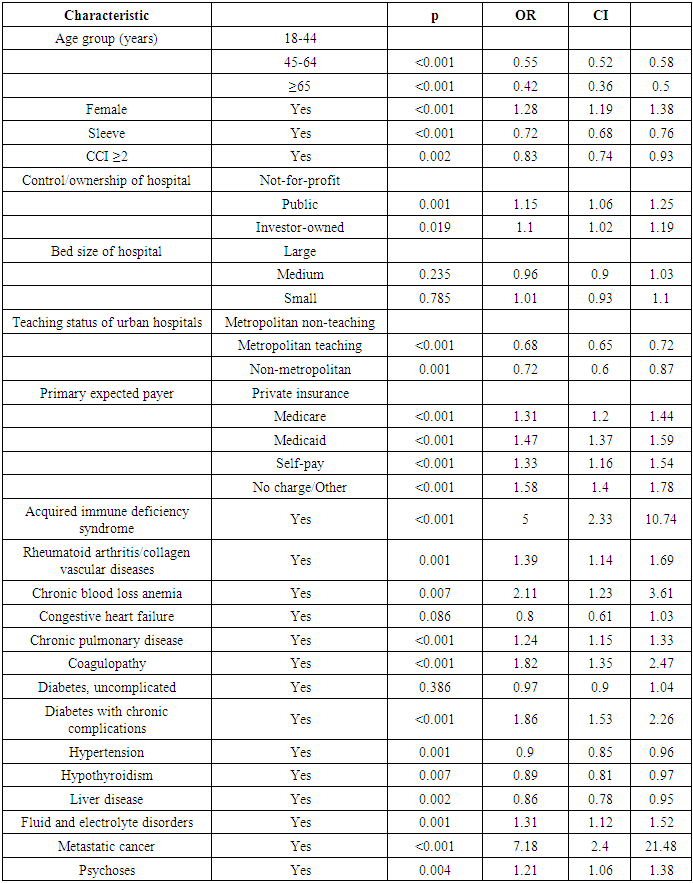
- Multivariate logistic regression was used to examine the relationship between risk factors and the odds ratio (OR) of hospital readmission after bariatric surgery. Females were more likely to require cholecystectomy for biliary disease (OR 1.28, p<0.001). Patients age ≥45 years were less likely to have cholecystectomy during hospital readmission (OR 0.55 for ages 45-64, OR 0.42 for ages ≥65). In addition, patients who underwent sleeve gastrectomy (OR 0.72, p<0.001) and patients with a CCI ≥2 (OR 0.83, p=0.002) were also less likely to have a cholecystectomy during readmission.The comorbidities associated with the highest odds ratio for cholecystectomy during 30-day hospital readmission following bariatric surgery were metastatic cancer (OR 7.18, p<0.001), acquired immune deficiency syndrome (OR 5.0, p<0.001), chronic blood loss anemia (OR 2.11, p=0.007), diabetes with chronic complications (OR 1.86, p<0.001), coagulopathy (OR 1.82, p<0.001), rheumatoid arthritis / collagen vascular disease (OR 1.39, p=0.001) and fluid and electrolytes disorders (OR 1.31, p=0.001). Interestingly, patients with hypertension (OR 0.90, p=0.001), hypothyroidism (OR 0.89, p=0.007), and liver disease (OR 0.86, p=0.002) had decreased odds of requiring a cholecystectomy during readmission following bariatric surgery.
4. Discussion
- As the prevalence of obesity continues to rise, the rate of bariatric procedures for weight loss also continues to increase. Bariatric surgery with rapid weight loss is associated with gallstone formation and patients experiencing symptomatic biliary sequelae after bariatric surgery may require cholecystectomy. It has been debated whether routine cholecystectomy should be performed at the time of the original bariatric surgery and there are currently no guidelines to support prophylactic cholecystectomy [2]. Since outcomes and readmission rates are being increasingly valued as hospital care quality metrics, it is crucial to identify trends in readmission and to recognize risk factors that predispose patients to the need for additional procedures [4,9]. This study examines data on a national level and tracks the incidence rate and risk factors for cholecystectomies performed during 30-day readmission after bariatric surgery across different hospitals. A study by Aman et. al. evaluated 36,042 bariatric surgery patients with a 30-day hospital readmission rate of 4.7% but did not specifically identify biliary causes [4]. Similarly, a study by Alteiri et. al. evaluated the rate of cholecystectomy after bariatric surgery to be 6.5% for laparoscopic adjustable gastric banding, 9.7% for Roux-en-Y gastric bypass and 10.1% for sleeve gastrectomy within 5 years following weight loss surgery [2]. However, during 2010-2015, we found that of the 886,596 patients who underwent bariatric surgery, less than 1% of patients underwent cholecystectomy during 30-day hospital readmission (0.6%). To our knowledge, this is the first study evaluating symptomatic biliary complications in the immediate post-operative period following bariatric surgery. According to the National Readmission Database, the majority of patients readmitted who underwent a cholecystectomy were female (84.5%) and between the ages of 18-44 years (67%). These results are consistent with a higher incidence of cholelithiasis and cholecystitis in females of reproductive age compared to males in the general population [1,10,11].These findings further support against performing prophylactic cholecystectomy as routine practice for bariatric surgery. While there is no guidlines to support performing prophylactic cholecystectomies, some argue it prevents the morbidity of symptomatic cholelithiasis, eliminates the diagnosis of atypical gastrointestinal symptoms, avoids technical difficulties especially in patients with Roux-en-Y bypass anatomy, and lowers overall healthcare costs [3,12,13]. Therefore, certain patients and risk factors may be considered on an individual case basis, such as patient’s undergoing Roux-en-Y bypass [14]. A meta-analysis by Tustumi et. al reviewed a cumulative 729,642 patients and demonstrated increased post-operative complications and length of operative time with concomitant cholecystectomy versus bariatric surgery alone [15]. Concomitant cholecystectomy during bariatric surgery may increase the rate of anastomotic leak or stricture, increased operative time, technical difficulties due to port placement, increased risk of converting to an open procedure, or bile duct injury [2,16]. However, the association between different types of bariatric procedures or the use of ursodiol to prevent gallstone formation needs to be evaluated in future studies. Given the rise in obesity and bariatric procedures performed annually in the United States, an understanding of risk factors for readmission in this population is important to improving post-operative management. We found that comorbidities with the highest odds ratio for requiring cholecystectomy within 30 days of bariatric surgery includes metastatic cancer, AIDS, chronic blood loss anemia, diabetes with chronic complications, coagulopathy, rheumatoid arthritis/collagen vascular disease and fluid and electrolytes disorders. Alternatively, patients age ≥45 years, sleeve gastrectomy patients, patients with CCI ≥2, and patients with hypertension, hypothyroidism or liver disease were less likely to have cholecystectomy within 30 days from bariatric surgery. These trends can be referenced as targets to improve readmission rates and decrease symptomatic biliary disease in the post-operative period following bariatric surgery. Both sleeve gastrectomy and Roux-en-Y bypass cause rapid weight loss which can lead to gallstone formation. The likely reason why gallstones and cholecystectomy rate is higher in post Roux-en-Y bypass versus sleeve gastrectomy though is because of both the supersaturation of bile with cholesterol secondary to a reduction in bile acid secretion because of the caloric restriction in addition to limited gallbladder contractility and emptying secondary to a reduction in the secretion of cholecystokinin due to the bypassed duodenum. [17]There are several limitations to this study which are largely inherent to the limitations of the National Readmission Database. The NRD is administrative in nature and hence is subjective to errors in data reporting. The NRD also does not collect information on race, and therefore we could not make conclusions on readmission rates and cholecystectomy risk factors based on race or ethnicity. In addition, the database does not specify reasons for readmission, and therefore we were unable to analyze patients readmitted for cholecystectomy and those readmitted for other reasons but received a cholecystectomy separately. Furthermore, certain clinical variables cannot be assessed with this data such as ursodiol administration to prevent gallstone formation and types of bariatric technique. Furthermore, this data set is limited to 30-day hospital readmissions and does not assess for overall rate of cholecystectomy following bariatric surgery. The strengths of this manuscript include a large national data set and the ability to assess for risk factors, which may reduce hospital readmission resulting in cholecystectomy after bariatric surgery.
|
|
|
5. Conclusions
- Biliary disease is a well-established sequela of the rapid weight loss following bariatric surgery. With the increasing prevalence of obesity and the rise of bariatric surgery procedures, prophylactic cholecystectomy has been debated. This study shows that less than 1% of patients who undergo bariatric surgery will develop symptomatic biliary disease requiring cholecystectomy during 30-day hospital readmission, even when accounting for readmissions across other hospitals. This study also identifies risk factors and comorbidities that put patients at increased risk for developing symptomatic biliary disease. Routine prophylactic cholecystectomy is not recommended, however bariatric surgery patients should be followed closely for risk of developing biliary complications.
Highlights
- • 0.6% of patients will undergo cholecystectomy within 30 days following bariatric surgery • Certain comorbidities may increase odds of developing symptomatic biliary disease after bariatric surgery • Age and type of bariatric procedure may influence requirement of cholecystectomy • Prophylactic cholecystectomy is not recommended prior to bariatric surgery procedures
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML