-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2020; 9(1): 9-16
doi:10.5923/j.surgery.20200901.02
Received: Aug. 22, 2020; Accepted: Sep. 12, 2020; Published: Sep. 26, 2020

Apache II Score as a Predictor of Hospital Mortality in COVID-19 Patients
Deepan Karthick1, M. Divahar2, Sathik1, Rajmohan1, J. A. Jayalal3
1Assistant Professors, Department of Surgery, Tirunelveli Medical College, TN, India
2Postgraduate Resident, Department of Surgery, Tirunelveli Medical College, TN, India
3Professor of Surgery, Tirunelveli Medical College, TN, India
Correspondence to: J. A. Jayalal, Professor of Surgery, Tirunelveli Medical College, TN, India.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Introduction: SARS-COV-2 disease 2019 has emerged as a major global health threat with a great number of deaths in the world amounting to nearly 8 lakhs. In this study we looked for the association between Acute Physiology and Chronic Health Evaluation II score and hospital mortality in patients with coronavirus disease 2019, and to assess the predictive ability of Acute Physiology and Chronic Health Evaluation II score. Method: It is a Retrospective observational cohort study carried out in a teaching hospital Tirunelveli medical college a teaching hospital in Tamilnadu, COVID care ward. 100 Confirmed patients with coronavirus disease -2019 as decided by the RTPCR testing and hospitalized in the COVID care unit with moderate to severe infection were included in the study. Results: Of these 100 potentially eligible patients with symptoms of coronavirus disease -2019, 14 patients died and rest 86 were cured with intensive care treatments. The Mean Acute Physiology and Chronic Health Evaluation II score (22.21 ± 6.05) calculated was relatively higher in patients who were succumbed to death with the mean Acute Physiology and Chronic Health Evaluation II score of 9.87 ± 4.40 in patients who have survived the infections (p < 0.001). Acute Physiology and Chronic Health Evaluation II score has shown independent association with the resultant hospital mortality (adjusted hazard ratio, 1.07; 95% CI, 1.01-1.13) and have demonstrated better discriminative ability (area under the curve, 0.966; 95% CI, 0.942-0.990). With the cut-off value of above 17, Acute Physiology and Chronic Health Evaluation score could predict the death of the patients with COVID -19 with a sensitivity of 96.15% and specificity of 86.27%. The survival probability of patients with coronavirus disease- 2019 with Acute Physiology and Chronic Health Evaluation II score less than 17 was notably higher (p < 0.001). Conclusions: For effective clinical prediction of hospital mortality in patients with coronavirus disease -2019, Acute Physiology and Chronic Health Evaluation II score can be used and when the score is greater than or equal to 17, it is an early warning indicator of death and will prompt the physicians to upgrade the treatment protocol.
Keywords: SARS-CoV-2, APACHE-11 Score, Hospital mortality
Cite this paper: Deepan Karthick, M. Divahar, Sathik, Rajmohan, J. A. Jayalal, Apache II Score as a Predictor of Hospital Mortality in COVID-19 Patients, International Journal of Surgical Research, Vol. 9 No. 1, 2020, pp. 9-16. doi: 10.5923/j.surgery.20200901.02.
Article Outline
1. Introduction
- Global world-wide pandemic was declared following the wide spread outbreak of coronavirus disease 2019 (COVID-19) caused by severe acute respiratory coronavirus 2 (SARS-CoV-2) by the WHO. [1] From its origin from the WUHAN, the disease has spread rapidly across the continents and as on the date 19 August 2020, there have been 21,938,207 confirmed cases of COVID-19, including 775,582 deaths, reported to WHO. [2].. Multivariant trial therapies, such as remdesivir and favipiravir, are under investigation and use, but the antiviral efficacy of these drugs is not yet fully known. This high grade viral infection with the available limited treatment strategies are resulting in a rapid progression from isolated pulmonary infection to multiple organ dysfunction (shock, acute respiratory distress syndrome [ARDS], cardiac injury, and acute kidney injury [AKI]), which manifest as extraordinary high mortality in such critically ill COVID-19 patients [3].Several descriptive cohort studies have previously reported citing the epidemiological, demographic, and clinical characteristics of COVID-19 patients, as well as severe cases. The advanced age, dyspnea, anorexia, and underlying comorbidities are more common in critically ill patients, [4,5] the risk factors contributing to the mortality of critically ill COVID-19 have not been fully identified.As the COVID 19 is gripping the world with its rapid spread, it is imperative to have a scoring system to categorize the patients on the basis of severity to prevent the mortality in a densely populated country like INDIA.Acute Physiology and Chronic Health Evaluation II score was proposed by Knauss WA, Draper EA, et all as a severity of disease classification system" in 1985. [6]. The score is calculated within 24 hours of admission of a patient to an intensive care unit (ICU and in this scoring score from 0 to 71 is computed based on several measurements.Various other scoring systems are also available such as A-DROP, CURB-65, PSI, SMART-COP, NEWS2, CRB-65 and qSOFA. In a study conducted by Guohui Fan.From Chinses Academy of Medical Sciences, in China With 654 patients enrolled, 133 patients died and 521 were discharged demonstrated Areas of under curves (AUCs) of A-DROP, CURB-65, PSI, SMART-COP, NEWS2, CRB-65 and qSOFA in the prediction of in-hospital death were 0.87, 0.85, 0.85, 0.84, 0.81, 0.80 and 0.73 respectively. [7]However as the researcher had used APACHE-11 Score by virtue of their use routinely in the surgical ICU and its reliability and accurate. Calculation.
2. Method of Collection of Data
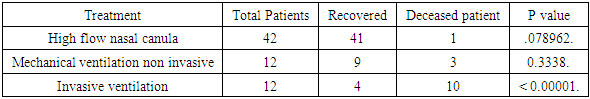
- This Retrospective study from May 2020 to July 2020 involved 100 cases who were randomly selected by using Purposive Sampling technique. For the enrolled patients the demographic profile, clinical symptoms and presentation details were collected on the day of admission using standard format. The laboratory values were obtained and APACHE-11 scoring done with in 24 hours. The associated comorbid conditions and treatment history were collected from the patients and validated with the records and attenders. The length of hospital stay, treatments offered and outcome were recorded.The patients were divided in to two groups based on the cut-off point value of APACHE II score as shown in the Figure 1 with the low risk values as less than 17 and the high-risk values as greater than or equal to 17.
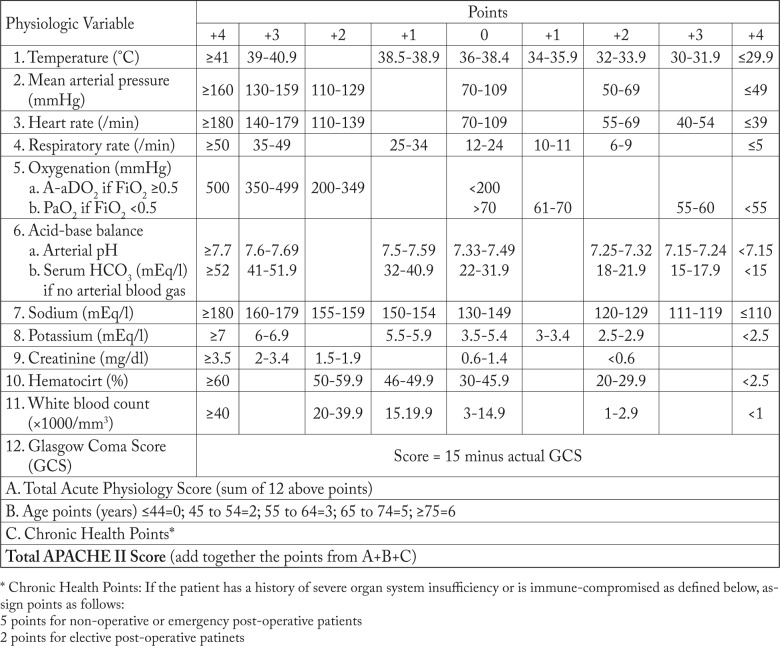 | Figure 1. Acute Physiology and Chronic Health Evaluation II score was proposed by Knaus WA |
3. Results
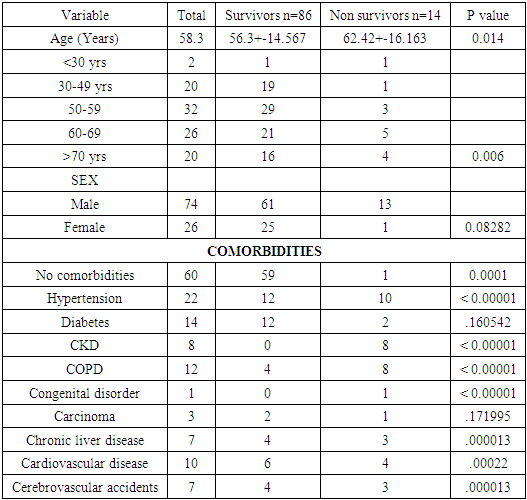
- Demographic and clinical factorsThe study population included a total of 100 admitted patients with confirmed COVID-19 infection from April to June 2020. The median age was 58.7(+-15.67) years. In those who recovered from the infection it was 56.3+-14.567 and in those who have succumbed it was 62.42+-16.163, it was statistically significant. P< 0.014.In our study out of 100 participants 74% were male and rest were female. 86(86%) patients recovered from the illness and 14 (14%) patients succumbed to the disease. Among the 14 deceased patients 13(92.8%) were male and 1(7.2%) patient were female. The recovery in the female patients were excellent and out of 26 female patients 25(96%) patients recovered and in male out of 74 patients only 61 (82.4) patients recovered.The numbers of patients with COVID-19 below the age of 30 years, between 30-49 years, 50-59 years, 60-69 years and above 70 years were 2 (2%), 20 (20%), 32(32%), 26 (26%) and 20 (20%) respectively. (Table 1). (Figure 2.)
|
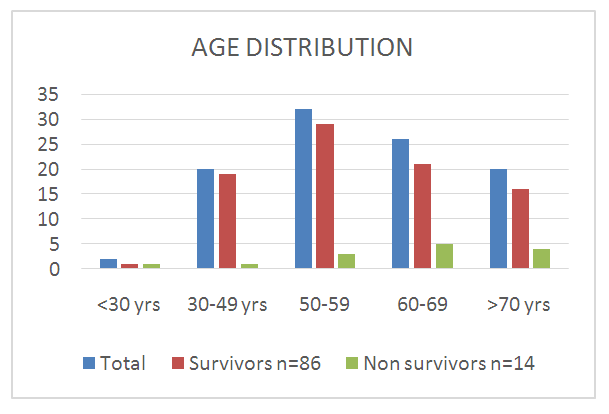 | Figure 2. Age Distribution |
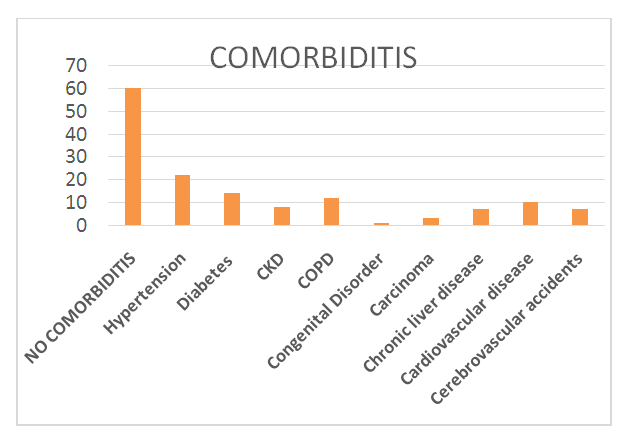 | Figure 3. Associated co morbidities |
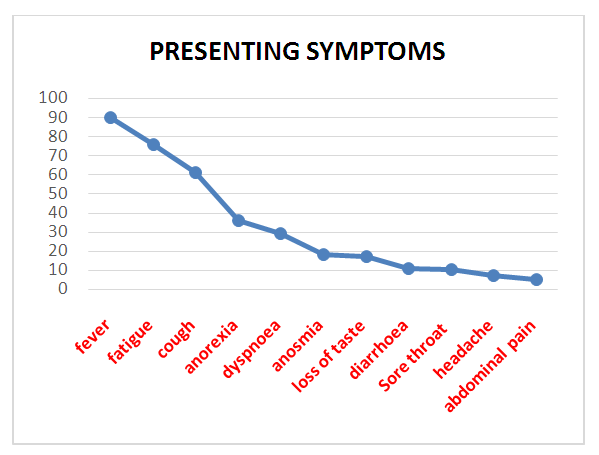 | Figure 4. Presenting symptoms |
|
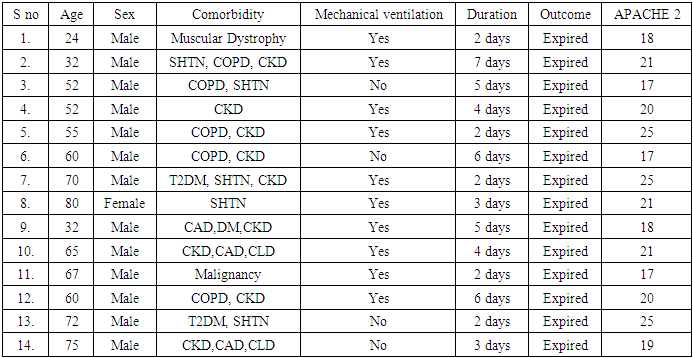
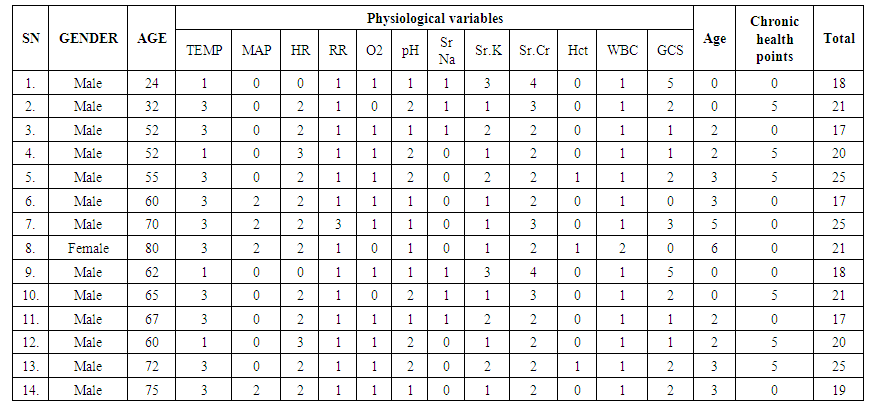 | Table 3. APACHE-11 Score of deceased patients |
|
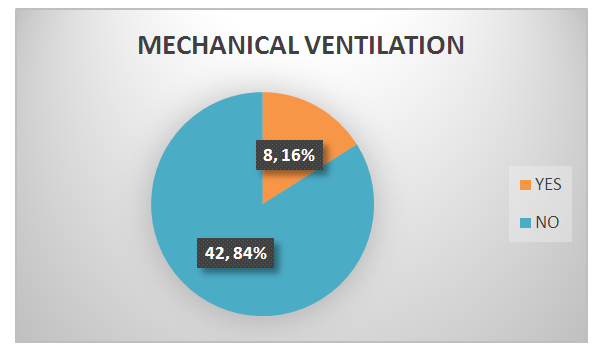 | Figure 5. Number of people on ventilation |
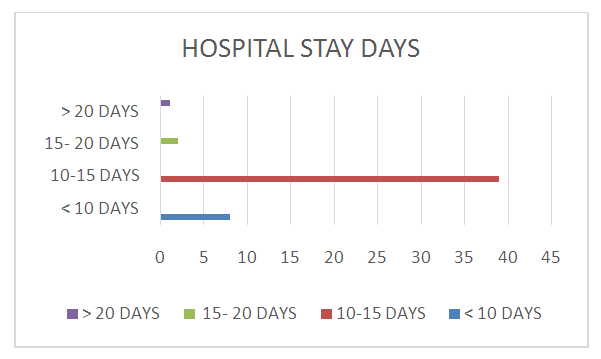 | Figure 6. Duration of hospital stay |
 | Figure 7. The fever chart |
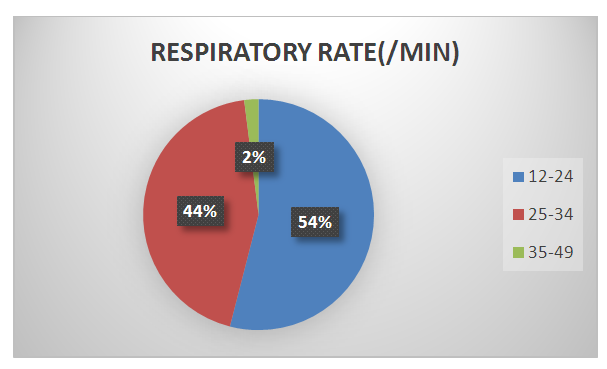 | Figure 8. The Respiratory rates of the patients |
4. Discussions
- In our study most patients (74, 74%) were men, and 26 patients were female. Liu X and Huang C in their respective reported studies also reported male preponderance in corona infections. [4,5] In our study out of 100 COVID-19 positive patients, 86 patients responded to treatment and 14 patient died due to associated comorbid conditions and aggressive progression of the disease. In a series of twenty-four observational studies including 10,150 patients from centres across Asia, Europe and North America, R. A. Armstrong have reported mortalities ranging from 0 to 84.6%. [8]All our patients were treated with PALM regimen including Prone position, Azithromycin, Low molecular weight heparin and methyl prednisolone. When patients had breathing difficulty non-invasive to invasive ventilator supports were given. Total 43 (72.9%) patients treated with non-invasive Mechanical ventilation and 16 (16.0%) with invasive mechanical ventilation. Once the patients required the treatment with mechanical ventilation and/or vasoconstrictive agents, it reflected serious condition of patients, which predicted poor clinical outcomes of the patients. Based on a metanalysis of 123 studies on use of ventilators in corona infected persons Schünemann HJ has concluded, indirect and low-certainty evidence suggests that use of non-invasive ventilation, similar to invasive mechanical ventilation, probably reduces mortality. However it may increase the risk for transmission of COVID-19 to health care workers. [9]According to a multicentre study published in JAMA Paediatrics based on the USA hospital, it is reported eighteen (38%) of 48 COVID-19 patients who were younger than 17 years hospitalized in 14 pediatric intensive care units (PICUs) required mechanical ventilation, but all but 2 survived. [10]Our data showed that the patients aged >70 years, with treatment delay, severe lymphopenia and thrombocytopenia, elevated interleukin 6, with acute kidney injury, cardiac injury, and arrhythmia, were at high risk of death. Among these factors, being over 70 years of age, with comorbidities of Cardiovascular disease and APACHE -11 score above 17 were identified as independent risk factors for mortality of patients in multi-variant regression analysis. Older age has been reported as an important independent predictor of mortality in SARS and MERS. [11]. In our study Twenty (20%) patients were aged over 70 years, which was an independent risk factor for death (HR=3.323, 95% CI=1.124–9.823). In those who recovered from the infection the age was 56.3+-14.567 and in those who have succumbed it was 62.42+-16.163, it was statistically significant. P< 0.014.SARS-CoV-2, has spike protein and it has a high degree of homology and have strong binding affinity to human angiotensin-converting enzyme 2 (ACE2). [12,13]. Angiotensin-converting enzyme 2 (ACE2) is a homolog of ACE which plays an important role in counterbalancing the actions of angiotensin (AT)II and promotes vasodilatation. The ACE2 is the main portal of entry of the virus to invade the body and enhances increase viral replications and infection. Wentao Ni, Xie et al in their studies demonstrated that ACE2 expression is relatively higher in young people than in elderly individuals and it is higher in females than in males. [14,15]. ACE2 has a protective role in acute lung injury and when there is lack of functional ACE2 in the lung it will lead on to the pathogenesis of lung injury. [12,13,14]. This is presumed to be a reason for the severe affection in the elderly male.It is noted in the pathogenesis of SARS-CoV-2 infections, ACE2 catalyzes the angiotensin II conversion to angiotensin-(1–7), the resultant ACE2/angiotensin-(1–7)/MAS axis helps in counteracting s the ill effects of the renin-angiotensin system (RAS), responsible for the balance between pathophysiology and physiology. The downregulation of ACE2 and the alteration in the balance between the Renin-angiotensin system and ACE2/angiotensin-(1–7)/MAS is the main contributory factor for the development of multiple organ injury in COVID-19. Based on this fact many trials are on in the process of developing the drugs and vaccine based on this SARS-CoV-2 spike glycoprotein, which binds to ACE2. It is also reporting by ensuring and correcting this imbalance due to the infection between the RAS and ACE2/angiotensin-(1–7)/MAS will enable to attenuate organ injuries. [16]One more symptom which was seen to be present more on the non survivors were diarrhoea. The manifestation of diarrhoea was more frequent in the people who succumbed to the disease than people who recovered, though the difference was not statistically significant (P>0.05). [17] Fan Y et al have shown in their study, Diarrhoea can be common symptom in coronavirus infections, presenting in 30% of patients with MERS and 10.6% of patients with SARS. [18]. It is also suggested as the ACE2 mRNA expression levels were high in the intestinal epithelium, faecal–oral transmission can acts as a super spreader. In our study 11 percentage of students gave history of diarrhoea as the presenting symptoms and in which 60% patients succumbed to disease.SARS-CoV-2 can cause myocardial injury, as assessed by increased troponin I level accompanying increased cardiovascular symptoms in COVID-19 patients. [3,19]. However there is dilemma in concluding whether cardiac injury is directly caused by viral infection or it is due to the secondary effects of hypoxia and associated systemic inflammation. The potent SARS-CoV-2 receptor, ACE2, is seen in cardiomyocytes and mural cells, particularly pericytes, which can induce Cardiac arrhythmias. It is also observed in our study due to this effect majority of COVID-19 patients had sinus tachycardia (72%) and sinus bradycardia in 14.9%. and the same thing was reported by Kochi AN in their study. [20]. It is also observed in our study that arrhythmia is an independent risk factor for mortality of critically ill patients with COVID-19 pneumonia. However who will get arrythmia and who will not be couldn’t be predicted. [21]Comorbidities plays a major role in predicting the outcome of the disease. Assessing the status of comorbid condition will alter treatment protocols. 40% of our patients had comorbid conditions and with comorbidity the mortality rate was shown markedly increased. Hypertension and Diabetes were the most common condition associated with cardiac, renal, liver and cerebral chronic disease. [22] Sanyaolu A, et al. in their study report on Comorbidity and its Impact on Patients with COVID-19 have stated, patients who have comorbidities, such as hypertension or diabetes mellitus, are more likely to develop a more severe course and progression of the disease when they are infected with COVID-19 infection. [23]APACHE II score have been widely used to predict the outcome of many critically ill patients especially pancreatitis patients. APACHE 11 score can not only predict which patients are likely to develop sepsis but also to predict which patients can survive sepsis or not. This will guide the physicians to plan and execute augmented care to the potential patients. [24]After calculating and assessing the APACHE -11 SCORE, based on that we could demonstrate that APACHE II scores were significantly higher in non-survivors than survivors (P<0.05). X Zou in their study reported from china, Mean Acute Physiology and Chronic Health Evaluation II score (23.23 ± 6.05) was much higher in deaths compared with the mean Acute Physiology and Chronic Health Evaluation II score of 10.87 ± 4.40 in survivors (p <.001). [25]
5. Limitations of the Study
- • Study had limited sample size, because only one hospital was included in this study. • It was a retrospective study as a result all patients were not having all the desired laboratory testing.• There is no rigid rule of treatment protocol followed in all patients and there was varied delay in the time of presentation to the concerned unit.
6. Conclusions
- SARS-CoV infections is spreading fast to infects millions of people. The risk stratifications and early identifications of the vulnerable sick patients and ensuring appropriate treatment protocols for them will be the way to make death as an exception rather than rule. Various scoring systems are proposed. APACHE-11 score (Acute Physiology and Chronic Health Evaluation II score) is a predictable and feasible scoring method to assess and segregate the potential severe grade patients. By calculating the APACHE-11 Score, when it is above 17, the patient will be a potential patient for aggressive management to prevent mortality. With the limited availability of resources, these patients after triage can be subjected to intensive therapy and mortality can be averted. The scoring system is a practically easier one with more optimum predictive value.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML