-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2019; 8(2): 15-17
doi:10.5923/j.surgery.20190802.01

Chronic Empyema Thoracic from Traumatic Bilothorax: Case Report and Review of Literature
Abubakar Umar1, Salisu Ismail2, Abdullahi Abdulkarim A.3
1Cardiothoracic Surgery Unit, Department of Surgery, Usmanu Danfodiyo University/Usmanu Danfodiyo University Teaching Hospital, Sokoto State, Nigeria
2Cardiothoracic Surgery Unit, Department of Surgery, Usmanu Danfodiyo University Teaching Hospital, Sokoto State, Nigeria
3Department of Anaesthesiology and Intensive Care, Usmanu Danfodiyo University/Usmanu Danfodiyo University Teaching Hospital, Sokoto State, Nigeria
Correspondence to: Abubakar Umar, Cardiothoracic Surgery Unit, Department of Surgery, Usmanu Danfodiyo University/Usmanu Danfodiyo University Teaching Hospital, Sokoto State, Nigeria.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Bilothorax is a defined as the presence of bile in the pleural space. Various aetiologies have been identified. Empyema thoracis occurring as a result of bilothorax is rare. We report a case of a 30-year old man that had blast injury to the right hypochondrion, subsequently developed right sided pleural fluid collection and jaundice. Thoracentesis yielded yellowish fluid. He had thoracotomy and decortication. Postoperative recovery was uneventful and patient was discharge.
Keywords: Empyema, Bilothorax, Thoracotomy, Decortication
Cite this paper: Abubakar Umar, Salisu Ismail, Abdullahi Abdulkarim A., Chronic Empyema Thoracic from Traumatic Bilothorax: Case Report and Review of Literature, International Journal of Surgical Research, Vol. 8 No. 2, 2019, pp. 15-17. doi: 10.5923/j.surgery.20190802.01.
1. Introduction
- Bilothorax is defined as presence of bile in the pleural space. It is said to occur as a result of hepatic trauma, subphrenic abscess, parasitic liver diseases and biliary obstruction. Iatrogenic causes include hepatic surgery, liver biopsy, cholecystectomy, biliary stent migration as well as percutaneous tranhepatic bilary drainage. An empyema thoracis is a collection of pus in pleural space which may be free-flowing or loculated [1-2]. Chronic empyema occurring as a result of bilothorax is not common. Our aim is to present a case of bilothorax causing chronic empyema thoracis and to review relevant literature.
2. Case Report
- A 30-year-old man who works in an oxygen cylinder shop. His main job is to refill oxygen cylinders. He was refilling a gas cylinder which exploded, and he sustained injuries on the right hypochondrion. He was rushed to a nearby hospital where his wounds were explored and closed. He subsequently developed jaundice (see fig. 1), right hypocondrial pain and difficulty in breathing as such was referred to our hospital. On examination on admission he was in respiratory distress, with a respiratory rate of 40cycles/minute, febrile, dehydrated and jaundiced. He had features suggestive of right sided pleural fluid collection. There was a scar on the right hypochondrion with minimal tenderness around the same region. Thoracocentesis yielded yellowish fluid and a chest drain was inserted and it drained yellowish effluent for about 2 weeks (see fig. 2). Analysis of the fluid yielded bilirubin. A diagnosis of bilothorax was made. Intravenous fluid Normal saline was used for resuscitation after which he was placed on Ringers lactate, he was also placed on intravenous cefuroxime and metronidazole. He had thoracotomy and decortication. Intraoperative findings were thick billous pleural effusion, thick cortex trapping the right lung, about 14cm tear in the right hemi-diaphragm with the right lobe of the liver herniating. There was liver injury (See fig. 3). Patient had decortication, repair of liver and diaphragmatic injuries, pleural cavity copiously irrigated with warm saline and chest was closed over a size 28F chest tube. Postoperative recovery was uneventful, drainage from chest tube gradually changed from yellowish to purulent and drain was converted to an ambulatory drain and patient was discharged home. He was followed up in the out-patient clinic until there was no drainage and significant lung re-expansion on chest X-ray. The ambulatory drain was removed.
 | Figure 1. Jaundice |
 | Figure 2. Billous effusion |
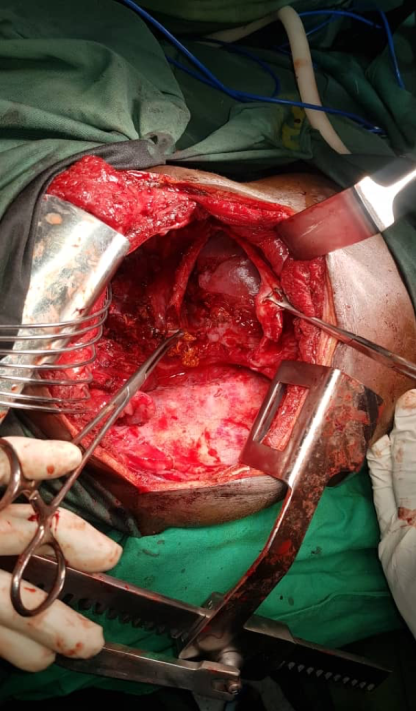 | Figure 3. Diaphragmatic Injury with liver Injury |
3. Discussion
- The term bilothorax was first coined by Williams in 1971 [3]. Since then other terms have been used to describe this condition which include cholethorax, bilithorax, pleurobilia and thoracobilia. Various mechanisms have been proposed in bilothorax formation which can either be direct extension of biloma through the diaphragm or through a congenital defect in the diaphragm or trauma to the diaphragm [4-5]. Spontaneous occurrence has also been reported [6-8]. Chronic empyema thoracis initially starts with sterile exudate in what is described as simple parapneumonic effusion and can gradually progress to become complicated. Majority of empyema thoracis result from extension from pulmonary infection, penetrating chest injury or postoperative surgical infection [9-10]. Transdiaphragmatic spread of abdominal infection has also been implicated [11-13]. Simple procedures in the pleural space like thoracocentesis, pleural or lung biopsy can also contribute to small number of cases of empyema thoracis [14]. There is an association between the presence of billous fluid in the pleural space and development of empyema thoracis. Oparah in 1978 reported in their series twelve out of their sixteen patients developed billous empyema [15]. Organisms that have been implicated in empyematous billous effusions are gastrointestinal tract organisms like Escherichia coli Enterobacter, Enterococcus faecalis, Klebsiella oxytoxa [16-18]. Infection is said to be caused by biliary obstruction. It is also a known fact that most of these gastrointestinal organisms are commensals in the gastrointestinal tract but become pathogenic once in the pleural cavity. Our patient presented to us about 2 weeks after the injury which is enough for infection to set-in. He initially had a chest tube inserted which kept on drained billous empyema and there was failure of lung expansion. A repeat CXR and a chest CT scan revealed a trapped lung with residual empyema. Based on these findings we opted for thoracotomy and decortication. Najjar et al reported thoracotomy in 7 patients in their series. Two had decortication on account of thick pleural cortex [20]. Oparah also did thoracotomy and decortication for two of their patients after chest tube drained failed [15]. Other authors have also reported successful outcome with thoracotomy and decortication in this patients [21-24]. Our patient had persistent drainage which was managed with open drainage and the drain was subsequently removed.
4. Conclusions
- Chronic empyema thoracis following bilothorax is rare. Right sided thoraco-abdominal trauma can cause liver and diaphragmatic injuries leading to herniation of the injured liver into the chest. This can result in bilothorax and infection in this setting may result in chronic empyema thoracis. Surgery remains the mainstay in this condition.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML