-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2019; 8(1): 5-10
doi:10.5923/j.surgery.20190801.02

Evaluation of Methylene Blue in Difficult Laparoscopic Cholecystectomy
Omnia M. Rabie
Lecturer of General Surgery, Department of G. Sug, Faculty of Medicine, AL-Azhar University, Cairo, Egypt
Correspondence to: Omnia M. Rabie, Lecturer of General Surgery, Department of G. Sug, Faculty of Medicine, AL-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2019 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

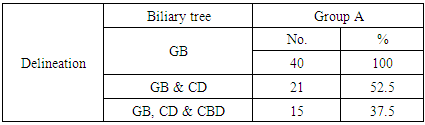
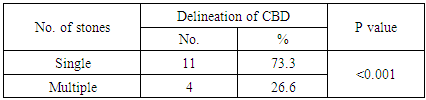
Background: Gallstone disease is very common & laparoscopic cholecystectomy is one of the most surgical procedures all over the world. There are many factors which make laparoscopic cholecystectomy difficult. These difficulties increase the risk of biliary injuries, open conversion, prolonged operative time & hospital study. Many procedures as intraoperative cholangiography & laparoscopic ultrasound were used to decrease complications of laparoscopic cholecystectomy in difficult cases. An attempt was made to compare the outcome & complications of laparoscopic cholecystectomy with & without methylene blue injection in gall bladder in difficult laparoscopic cholecystectomy. In addition, delineation of the different part of the biliary system was evaluated. Patients & methods: Eighty patients have symptomatic cholelithiasis with a risk factor for difficult laparoscopic cholecystectomyadmitted for laparoscopic cholecystectomy. They were randomly divided into two groups, (A) with methylene blue injection in gall bladder during laparoscopic cholecystectomy & (B) traditional method without methylene blue injection. Conversion to open cholecystectomy, operative time, hospital stay & postoperative complications were recorded. Results: The result showed that mean operation time 65.5 ±8.7 & 70 ±12.7 in group A & B respectively, hospital stay was one day in group A & 1-2 days in group B. Conversion open cholecystectomy were one case group A & three cases group B. No biliary leakage or stricture in both group. Stone spillage one case in group B. As regrade group A two cases of extravasation of dye, one case urine discoloration, 100% gall bladder delineation, gall bladder & cystic duct 52.5% delineation & gall bladder, cystic duct &common bile duct delineation was 37.5%. Conclusion: methylene blue injection in gall bladder during difficult LC may help to decrease operative time, hospital stay & avoid complications of biliary injury.
Keywords: Difficult cholecystectomy, Methylene blue, LC
Cite this paper: Omnia M. Rabie, Evaluation of Methylene Blue in Difficult Laparoscopic Cholecystectomy, International Journal of Surgical Research, Vol. 8 No. 1, 2019, pp. 5-10. doi: 10.5923/j.surgery.20190801.02.
Article Outline
1. Introduction
- Gallstone disease is the most frequent disease after coronary heart disease and diabetes mellitus in industrial countries, it represent10-20% [1]. Over 100 years the safe cholecystectomy need a generous abdominal incision to provide good exposure and lighting. Laparoscopic cholecystectomy was introduced and widely used in late 1980, as a result of improved optics [2]. LC has an advantage than open procedure as minimal postoperative pain, better cosmoses, short hospital stay and early recovery [3, 4]. There are many factors which make LC difficult as chronic cholecystitis with scarring of Calot’s triangle, fibrotic and contracted gallbladder, cholcystoenteric fistula, old age, male sex, obesity, attacks of acute cholecystitis with fever and leukocytosis, gangrenous gall bladder and previous abdominal surgery [5]. Certain ultrasonograpbic findings such as thickened wall gallbladder, distended gallbladder impacted stones or pericholecystic collection also make it difficult [6]. In such cases conversion to open surgery is an option. An early conversion to open cholecystectomy is indicated when there are difficulties will result in bile ducts injuries or life-threatening complications [7, 8]. Personal ego and feeling of failure are the main two factors of surgeons that contribute to blind and impatient dissection in cases of difficulty [9]. Conversion from LC to OC has a disadvantage as it increases perioperative time, complication rates, perioperative costs, the length of hospital stay, and hospital charges [10]. It also associated increased risk of death, bile leak, bile duct injury, or bleeding, requiring reoperation or transfusion [11]. To decrease these complications different modalities have been described for intraoperative assessment of biliary anatomy during LC to decrease as intraoperative cholangiography (IOC) and laparoscopic ultrasound (LUS) [12]. A methylene blue injection into the lumen of the gall bladder to delineate cystic duct and CBD described by Sari et al 2005. This technique seems easier to perform, no need for radiation exposure and less time consuming than conventional IOC [13]. In this study, we used this technique in difficult LC to reduce the time consumed, avoid biliary leakage or injuries and decrease conversion to OC. The aim of this work is to evaluate methylene blue in difficult LC in comparison to the traditional method.
2. Material and Method
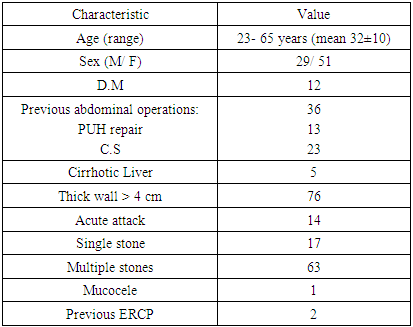
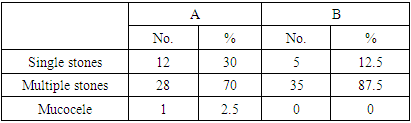
- A prospective cohort study was conducted in the general surgery department in AL-Zahraa University hospital from May 2016 to November 2018 to evaluate Methylene blue injection during difficult laparoscopic cholecystectomy compared to traditional method. The study involved 80 patients with symptomatic cholelithiasis with a risk factor for difficult laparoscopic cholecystectomy e.g. obesity, previous abdominal operation (table 1) (table 2). The main complaint was a pain in right upper abdomen, epigastric pain, dyspepsia or fat intolerance. For every patient, the informed consent form was obtained which included detailed demographic data, also medical history and examination, essential investigations in form of abdomen US, liver function test, kidney function test, CBC, fasting and postprandial blood sugar was done. Exclusion criteria were patients with renal impairment, multiple drugs allergies, relative contraindications for laparoscopic surgeries, intraoperative easy cholecystectomy. Patients were randomly divided into two groups, group (A) include 40 patients without methylene blue injections and group (B) include 40 patients with methylene blue injections during LCS.
|
|
3. Operative Technique
- All patient had LC under general anesthesia after receiving perinduction 1g ceftriaxone intravenously. An orogastric tube was inserted to decrease gastric distension which may affect the view of Calot′s triangle. The surgical site was prepared and draped according to standard protocol. The patients were in reverse Trendelenburg position slightly tilted to the left side. Pneumoperitoneum was done by carbon dioxide by a veress needle through a transverse incision above umbilicus in which subsequently replaced by10mm port for 30 -degree laparoscopic camera. Working port 10 mm was placed high in epigastrium to the right side of falciform ligament. 5mm port through which a grasping forceps for fundus of the gall bladder was inserted in anterior axillary line midway between coastal cartilage and anterior superior iliac spine. Finally, 5 mm port was placed in the right midclavicular line below the liver edge. In group A, the fundus of gall bladder was grasped and held tightly toward the anterior abdominal wall after dissection of adhesion. All bile in gall bladder was aspirated through spinal needle 18 G and an equal amount of diluted Methylene blue 60% was injected through the abdominal wall (fig 1). To prevent leakage of methylene blue fundus was grasped tightly toward the anterior abdominal wall at the site of the puncture. Gall bladder completely was seen so dissection completed, Hartman pouch grasped and retracted caudally to the right. Peritoneal layer overlaying cystic duct- gall bladder junction was dissected. Cystic artery and duct were clipped after they clearly appeared. In group B all as previous except no injection of methylene blue. Peritoneal wash was done in all cases where there were bile or dye leakage, or minimal bleeding from dissected adhesion around gall bladder. Drains were inserted for all cases.
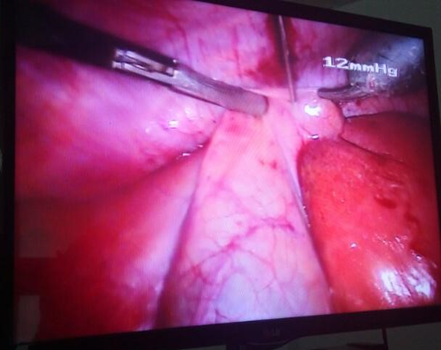 | Figure 1. Injection of methylene blue in a gall bladder |
4. Result
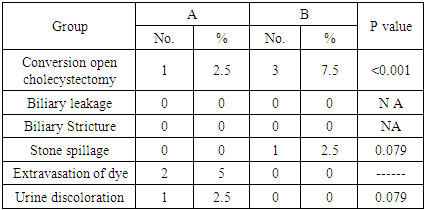
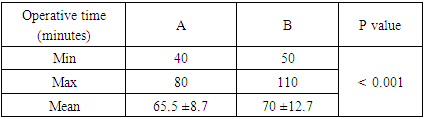
- Eighty patients were included in this study, 29 men (36.25%) and 51(63.75%) women while means age mean 32±10. our patients randomly grouped in group A with methylene blue injection during LC and group B with traditional method for LC without methylene blue. As regard conversion to open cholecystectomy in group A there were one (2.5%) cases due to extravasation of dye and disturbed anatomical view. In group B there were 3 (7.5) cases, one case for uncontrolled bleeding from the cystic artery and the other two cases there was severe adhesion with difficulties in dissection and unclear anatomy. There were no biliary leakage or biliary injury or strictures in both groups. In group A 2 (5%) cases had extravasation of dye, one during removal of the needle after injection of dye and the other due to an injury of gall bladder during its dissection (fig 2). One (2.5%) case had urine discoloration. As regard stone spillage there was one (2.5) case recorded for in group B (table 3). Operative time range 40-80 minute and 50- 110 minute in group A and B respectively (table 4). Hospital stay one day in group A and 1-2 days in group B. As regard to group A use of methylene blue result in delineation of all gall bladder 40 cases (100%) (fig 3), 21 cystic ducts were delineated (52.5%) (fig 4), while common bile duct delineated in 15 cases (37.5%) (fig 5).
|
|
 | Figure 2. Extraversion of dye |
 | Figure 3. Delineation of gall bladder |
 | Figure 4. Delineation of gall bladder & cystic duct |
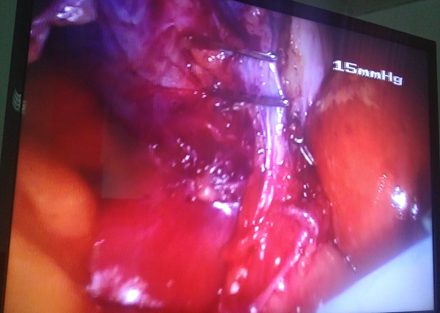 | Figure 5. Delineation of cystic & CBD |
5. Discussion
- The primary goal of LC is ‘‘safety first, total cholecystectomy second.’’ While the majority of laparoscopic cholecystectomies performed will be straightforward, the surgeon should always keep this culture of safety in his mind when dealing with a difficult situation [14]. LC has some disadvantage considered as complications like an injury to the common bile duct, bowel, iliac vessels etc., costly equipment, high conversion rates (10-50 %) in acute cholecystitis, difficulty in management of simultaneous common bile duct stones and limitation of a facility to the tertiary health care centers [15]. LC considered difficult when there are difficulties during access or dissection and safe completion of the procedure cannot be ensured. Difficulties usually due to an anatomical ductal and vascular anomaly or distorted anatomy following acute or chronic inflammation [16]. Many studies recommend some instructions and method to avoid complications as adequate training in laparoscopic surgery, proper delineation of biliary anatomy in Calot’s triangle, judicious use of electrocautery, avoiding blind application of clips and cautery, performing intraoperative cholangiogram, and converting to open procedure in the event of failure to progress or unclear anatomy [17]. Intraoperative cholangiography (IOC), Laparoscopic ultrasound (LUS), intraoperative choledochoscopy, Light cholangiography, passive infrared cholangiography, fluorescein- guided LC [12] and Near-infrared assisted LC all these procedures has been described for intraoperative assessment of biliary anatomy to increase safety in LC [18]. A methylene blue injection into the lumen of the gall bladder to delineate cystic duct and CBD described by Sari et al 2005 [13]. This technique seems easier to perform, no need for radiation exposure and less time consuming than conventional IOC [13, 19]. Study of Nikhil Gupta et al, 2013 [5] & Shreenath Patil & Padmanabh S. 2016 [20] reported that male gender, old age, previous ERCP, obesity, and acute cholecystitis are the risk factor for difficult LC. Our study included 80 patients 51 were female and 29 males their age range from 23- 65 years (mean 32±10), all had calcular cholecystitis with a risk factor for difficult LC cholecystectomy. The patients randomly grouped into two groups. Group A with methylene blue injection during LC, group B traditional method. As recommended by Ramlah Ghazanfar et al, [21] we concerned with safety during LC in both group by used orogastric tube to avoid gastric distension which affects a surgeon´s view of the triangle of Calot. Also as Fernando Santos et al, [14] we used an angled laparoscopic camera 30° insteated of straight for better visualization the medial and lateral aspect of gall bladder as well as obtain more of “bird´s eye” view of the operative field and reverse Trendelenburg position with slight tilt to the patient´s left for adequate exposure of gall bladder in all patients. Conversion from LC to OC in group A less than in group B as it was one case (2.5%) due extravasation of dye and disturbed anatomical view while in group B there were 3 (7.5%) cases, one case for uncontrolled bleeding from cystic artery and the other two cases for severe adhesion, difficulties in dissection and unclear anatomy (table 3). However current literature suggests that, conversion rate from LC to OC was 6% [22], 3% [23], 1- 15% [24, 25] and 7- 35% [26]. In group A there were 2 cases 5% of methylene blue extravasation while there were 5 cases 11% had methylene blue leakage from gall gladder in Sari et al 2005 study [13]. In group A also all gall bladder 100% delineated, 21 cystic ducts 52.5% while 15 common bile duct 37.5 % were delineated (table 5). CBD delineation in relation to the numbers of gall stone was 11 cases (73.3%) had a single stone & 4 cases (26.6%) had multiple stones (table 6). Our result different from Sari et al 2005, they found that from 46 cases gall bladder, cystic duct, and ductal choledochus were painted with methylene blue in 43 cases (93.47%) but only gall bladder and proximal cystic duct were visualized in 3 cases (6.5%) [13]. Also Sajid 2016, he found that gall bladder delineation 98.9%, cystic Hartmann´s pouch 92.8%, whole cystic duct 62.2%, common bile duct 32.6% [19]. Methylene blue excreted through kidney so urine discoloration may occur which occur in one case only 2.5%. operative time in group A ranged from 40 -80 minutes with a mean 65.5 ±8.7 minutes, this differs from the result of Sajid 2016 where the mean operative time was 55 minutes [19]. No operative time recorded in Sari et al. Operative time in group B ranged from 50- 110 with mean 70 ±12.7 which longer than operative time in group A. In Subramaniyan P et al, mean operative time differ from 54.22 minutes to 78.25 minutes according to male or female, age above 60 or below, gall bladder walls thickened or not an acute cholecystitis [27]. Hospital stays in our study in group A one day while in the study of Sajid 2016 mean was 26 hours [19] while in group B was range from 24 – 48 hours with mean 29±6 hours. Study of H. Asbahceci et al 2012 recorded mean hospital stay 1.2 days [28], while K. Leick et al recorded it 2.1 ±2.5 days [23]. As regard biliary injury or leakage no recorded case in both group. The prospective study of Viste et al 2015 recorded 0.9% bile leakage and 0.4% injury to CBD or right hepatic duct [29]. There was one case 2.5% of stone spillage in group B while in group A no case recorded. Sabah A et al 2018, recorded 3.82% spillage of gallstones to the peritoneal cavity [30].
|
|
6. Conclusions
- From previous we recommend methylene blue injection in gall bladder during difficult LC as methylene blue dye not expensive, has no major side effect and the technique not need for radiation or complicated equipment also this technique decrease operative time, hospital stay and help in avoiding biliary injury.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML