-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2018; 7(1): 1-6
doi:10.5923/j.surgery.20180701.01

Cystic Lymphangioma of the Mesentery: Difficulties of Diagnosis and Surgical Treatment Outcome
A. Bendjaballah, A. Haider, M. Nedjam, Walid Nader, M. Ait Said, R. Oudjit, Y. Belalem, A. Bedoui
Department of General Surgery, Ain Taya Hospital, Algiers, Algeria
Correspondence to: A. Bendjaballah, Department of General Surgery, Ain Taya Hospital, Algiers, Algeria.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Lymphangiomas are rare benign congenital malformations of the lymphatic system. They are thought to happen due to obstruction of the local lymph flow. Lymphangiomas may arise in any part of the body. Approximately 95% of lymphangiomas are found in the head, neck and axilla, and 5% appear in other parts of the human body. Lymphangioma of the mesentery is exceptional. Lymphangiomas are usually growing slowly and patients remain asymptomatic for a long time. We report a case of a cystic lymphangioma of the mesentery lymphangioma of the peritoneum in young man treated by total excision of the cyst.
Keywords: Lymphangioma, Benign congenital tumors, Lymphatic system, Mesenteric cyst
Cite this paper: A. Bendjaballah, A. Haider, M. Nedjam, Walid Nader, M. Ait Said, R. Oudjit, Y. Belalem, A. Bedoui, Cystic Lymphangioma of the Mesentery: Difficulties of Diagnosis and Surgical Treatment Outcome, International Journal of Surgical Research, Vol. 7 No. 1, 2018, pp. 1-6. doi: 10.5923/j.surgery.20180701.01.
1. Introduction / Background
- Mesenteric cyst is defined as a cystic lesion located between the leaflets of the mesentery from the duodenum to the rectum, being most commonly found in ileum level. Since its first description in 1507 by Benevienae until 1993 there are only about 820 cases reported in the literature [1, 2] Lymphangiomas are rare tumors of the lymphatic system comprised of multiple cystic spaces lined by endothelium. They are generally benign tumors. They are unusual in abdominal location. Its incidence is estimated at around 1:100,000 and 1:20,000 admissions in adults and in children. The first excision was performed by Tillaux (quoted Chung) only in 1802 [3] Despite the long recognition of this disease, its origin classification and pathology remain controversial. Lymphangiomas are a major group of so-called vascular hamartomas, which result from a failure in the evolutionary development of the vascular system, including lymphatic and/or arteries and veins [4]. These lymphatic tumors are divided in: 1/ simple, with capillary lymphatic channels; 2/ cavernous, with dilated lymphatics and the presence of capsule; and 3/ macrocystic malformations, clinically termed "cystic hygroma” [2] This is the most common type, and the most affected sites are head and neck. The main differential diagnosis is hemangioma, branchial cysts, lipomas and rabdmiossarcoma.
2. Case Report
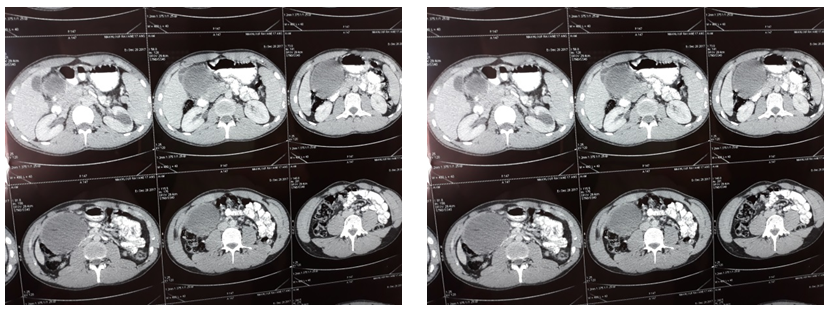
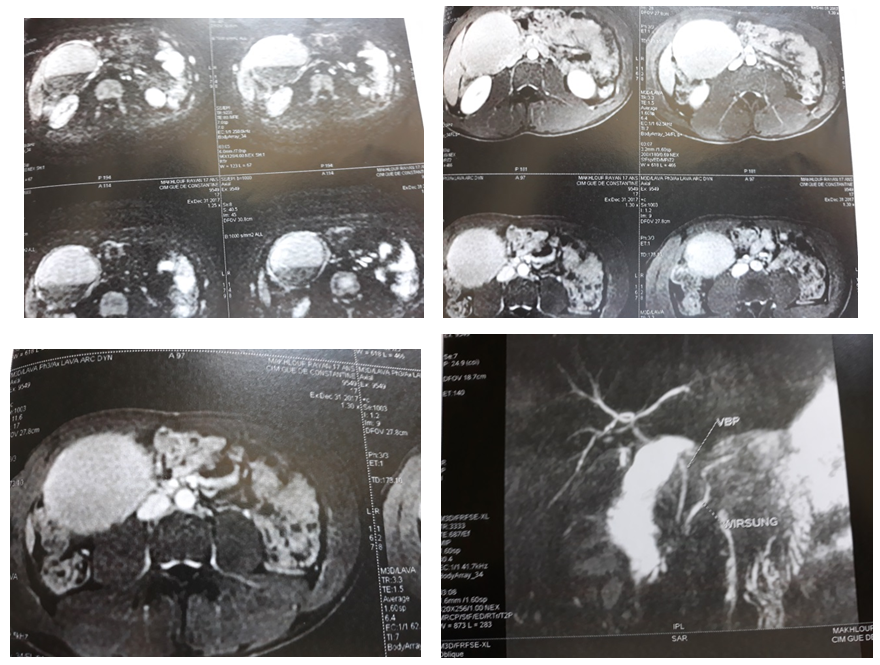
- A 17 years old young man admitted in surgical department for a cystic lymphangioma of mesentery for 1 year of evolution. There is no history of any illness. General and systemic examination of the patient was characterized by a good general condition, no pallor, no jaundice and no lower limbs oedema. Examination of respiratory and cardiovascular systems revealed no abnormality. Blood examination was within normal values. Chest x-ray examination and ECG were without abnormalities. The Ultrasound examination had shownt a bulky retouched cyst with a haemorrhagic appearance in the liver. (Figure 1). The CT scan has objected a cystic formation under hepatic oval well limited to regular contours with a thin wall measuring 100 x 90 x 75 mm pushing the duodenum forward and coming in contact with the head of the pancreas (Figure 2). The abdominal MRI with MRI of biliary tree highlighted: a cystic mass remodeled from the right flank independent of the biliary tree and neighboring organs. Two differential diagnosis are to be mentioned: mesenteric cyst or digestive duplicate. The biliary tree was without abnormality (Figure 3). Patient was operated and complete removal of .the cyst was carried out (Figure 4). He passed a smooth post-operative period et he was discharges on the fourth post-operative day. Histopathological result was in favor of cystic lymphangioma of mesentery.
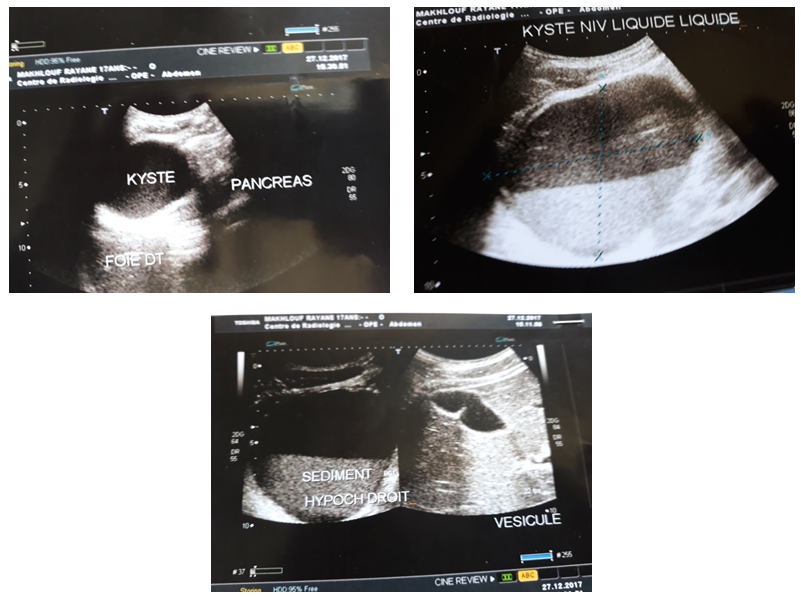 | Figure 1. Abdominal USE shows: a huge restored cyst with a haemorrhagic appearance in the liver |
 | Figure 4. Complete resection of the mesenteric cystic lymphangioma |
3. Discussion
- The lymphatic system consists of a network of unidirectional vessels that collects excess fluid from the interstitium, transports it to the regional lymph nodes and ultimately drains to the venous system via the thoracic duct. The lymphatic vessels are seen in all organs except in the brain, anterior chamber of the eye and in systems with rich sinusoidal networks such as bone marrow and spleen [7] Cystic cavernous lymphangiomas are uncommon benign slow growing tumor derived from the lymphatic vessels [8] It is more frequently found in childhood (60% are present at birth, and 90% are detected by the end of the second year), and mostly diagnosed in the first five years of life [8, 9]. It etiology is remains unclear. Congenital malformation of the lymphatic vessels leading to sequestrations of lymphatic tissue seems to be the cause of this condition [10]. The classification of lymphangiomas is mainly based on the size of the lymphatic space and the nature of the lymphatic wall [11, 12]. The cystic form is characterized by a thin irregular wall covered by endothelium, smooth muscle, foam cells and lymphatic tissue; it appears as a multiseptated, cystic mass with or without intracystic debris and has no connection with the adjacent normal lymphatics [13].Within the abdomen, the most common site of lymphangioma is the mesentery (mesenteric lymphangioma) in which most lymphatic channels are included [14]. Lymphangioma of small bowel mesentery is the commonest (70%) of intraperitoneal sites, with 50% to 60% of all cysts located in the ileal mesentery [15]. Other possible locations include the omentum, retroperitoneum, mesocolon, pancreas, spleen and adrenal gland [16]. The most frequent classification system used for lymphangiomas is still that of Wegner who categorized them as simple, cystic or cavernous, however, Losanoff et al. [17] reported another classification into pedicled, sessile, retroperitoneal extended or multicentric that may help in their treatment strategy. Thin walled lymphatic vessels situated superficially in the skin characterize the simple type. The cavernous type is composed of dilated lymphatic vessels and lymphoid stroma and has connections with normal adjacent lymphatics mass with or without intracystic debris and has no connection with the adjacent normal lymphatics. [13]. Thin walled lymphatic vessels situated superficially in the skin characterize the simple type. The cavernous type is composed of dilated lymphatic vessels and lymphoid stroma and has connections with normal adjacent lymphatics [11]. The size and location of the lymphangiomas are the determinants of the clinical presentation. Occasionally, the tumor is also discovered in adult in various other anatomic sites. It most often occurs in the head and neck, axillae, or groin of young children. It is rarely found as intra-abdominal masses when occurring in the abdomen (2-10% in the internal organs) [17]. The clinical manifestations vary from an asymptomatic state to acute onset of severe abdominal pain. Cystic lymphangiomas might arise with acute abdominal pain associated to bowel obstruction, signs of peritonitis, chronic abdominal swelling that is detected by palpation of a cystic mass or abdominal swollenness with lower extremities lymphoedema [18-20]. Diseases requiring particular attention to accurate diagnosis include: pancreatic pseudocyst, mucinous cystadenoma, serous cystadenoma and congenital neoplasms [21]. To ensure distinction between cystic lymphangioma and the aforementioned situations, diagnostic tools such as plain abdominal films, abdominal CT, and magnetic resonance imaging (MRI) may be utilized. The abdominal ultrasonography is the procedure of choice for establishing the diagnosis, even during the antenatal stage. A cystic lesion with multiple thin septa is the typical Ultrasonography finding of a mesenteric lymphangioma. Cavernous lymphangiomas appear as solid masses on CT. The MRI is more useful than CT for detecting fluid-filled cystic lesions like cavernous lymphangioma, as it has been for our patient [22]. Cystic lymphangioma should also be differentiated from cystic mesothelioma and lymphangiomyomas. They have similar histological appearance - Immunohistochemically, lymphatic endothelium is positive for CD31, CD34 and D2-40, Factor VIII related antigen, endothelial receptor- 1, vascular endothelial growth factor-3, prox-1 expression and negative for cytokeratins (Hornick et al., 2005). Calretinin and HMB-45 can differentiate lymphangiomas from multi-cystic mesothelioma and lymphangiomyoma respectively [23]. Earlier, lymphangiomas had been considered to be neoplastic in nature and capable of aggressive behavior. However, some investigators now believe that lymphangiomas are hamartomas. Others believe that both neoplastic and hamartomatous theories are possible [24]. Fibrosis of lymphatic channels following surgeries or infections leading to dilatation of the proximal channels has been postulated to be the underlying pathogenesis. [25]. The final diagnosis is always based on the histological findings, since this examination shows extensive myofibroblastic areas and objectifies the lymphatic character of the lesion [26].Although cystic lymphangiomas are benign tumors, they may compress adjacent structures via a mass effect. Other complications, including rupture, secondary infection, volvulus, or intestinal obstruction, have also been reported [27, 28]. In our case the big cyst had intimate relationships with gallbladder, right colon, transverse colon, duodenum first jejunal loop and stomach which necessitated a longer time for the release of the cyst from these attachments with the aforementioned organs. The gold standard treatment modality of cystic lymphangiomas is surgical excision. Treatment with OK-432, steroids, bleomycin, fibrin glue, or Ethibloc has not been established to be superior to surgery However, some authors recommend conservative management of asymptomatic cystic lymphangiomas due to the spontaneous regression rate of 10% [17]. Other treatment modalities including aspiration and injection of sclerosant agents may be performed for emergent decompression; nevertheless, these approaches are not recommended for elective therapy due to the high recurrence rates. The treatment is mainly surgical; it consists of enucleation when feasible; the segmental intestinal resection is achieved when the cyst adheres intimately to the bowel [29]. Prognosis is excellent if cyst resection is complete [30, 31]. This therapeutic option (complete cyst ablation) was applied for our patient (Figure 4). If complete cyst excision is not possible because of its huge size, deep location within the root of mesentery or it infiltrates the main branch of arteries or IVC, the other option is partial excision of the cyst with marsupialization of its remaining part into the abdominal cavity. About 10% of patients need this form of therapy [32]. Tumors were cystic masses associated to areas of fat necrosis and hemorrhage. Often, cysts contain thick, gelatinous or milky fluid. In our case the fluid had a chocolate brown color. The recurrence rate ranges from 0% to 13.6%, averaging about 6.1%. Most recurrences occur in patients with retroperitoneal cysts or those who had only a partial excision. Location of the cyst does not influence the recurrence rate if it is resectable [33, 34]. The resection could be performed with laparoscopic technique without large incisions [17]. In our case a try at a laparoscopic approach (Fig 5) was attempted, but the existence of multiple adhesions with neighboring organs forced us to opt for laparotomy. Laparotomy or laparoscopy both are acceptable routes of surgery for treatment. There are several reports in the literature of successful open resection of intra-abdominal lymphangiomas, but only few such report describing the laparoscopic treatment of an cystic mesenteric lymphangioma. It has inherent advantages in the form of less intra-operative blood loss, early recovery, less morbidity, and low complication rate compared with laparotomy [35].
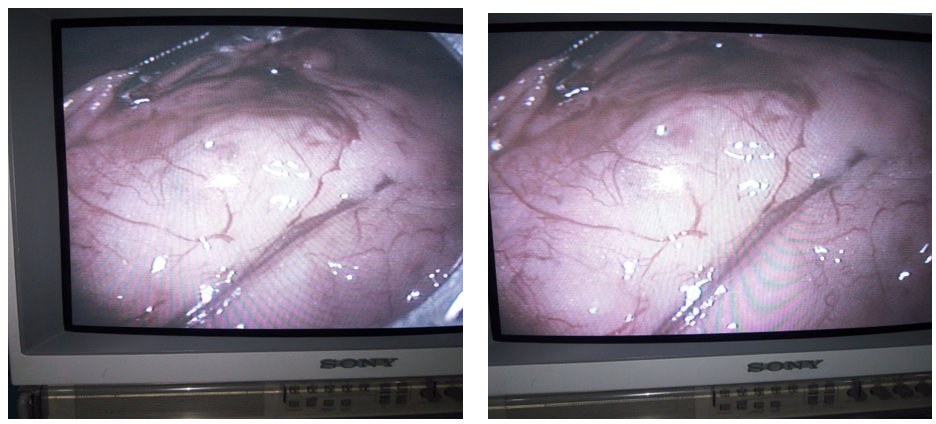 | Figure 5. Laparoscopic view of the cystic lymphangioma of the mesentery |
4. Conclusions
- The cystic Lymphangioma of the mesentery is extremely rare benign tumor. The clinical symptomatology is polymorphic and not specific. It’s preoperative diagnosis is usually difficult due to its variable misleading clinical presentations, rarity of the disease, and its resemblance to many other intraperitoneal cysts The diagnosis is suggested by the imaging modalities (US, CT& MRI), however, the definitive diagnosis is made only after histopathological examination of the excised specimen. The treatment of choice is surgical and consists of a full resection of the lesion. The intracystic sclerotherapy could be used for symptomatic tumors. Even though, they are being benign in nature majority of the time, total resection and regular follow up is mandatory. The laparoscopic excision is a safe and reliable approach for the treatment.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML