-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2017; 6(2): 25-28
doi:10.5923/j.surgery.20170602.01

Right Lumbar Incisional Hernia Repair after Iliac Crest Bone Graft: A Case Report and Literature Review
A. Aissat1, A. Mesbahi1, M. Habarek1, A. Bendjaballah M. D.2, M. Taieb2, N. Nait Slimane2, R. Khiali2
1Department of Surgery Tizi Ouzou’s Teaching Hospital, Tizi Ouzou, Algeria
2Department of Surgery Ain Taya Hospital, Algiers, Algeria
Correspondence to: A. Bendjaballah M. D., Department of Surgery Ain Taya Hospital, Algiers, Algeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The most common source for autologous bone graft is the iliac crest. Use of autologous bone grafts is common in orthopedic surgery. However this procedure, may be associated with considerable morbidity. Among this complications, lumbar hernias occur rarely with a stated incidence of 4% to 10%. The diagnostic study of choice is represented by Computed tomography (CT). Surgical repair is preconized to avoid and prevent the risk of incarcerated or strangulated bowel. Several transabdominal, retroperitoneal, and laparoscopic approaches have been described to repair this lumbar hernias. We report a case of lumbar incisional hernia repair successfully after iliac crest bone graft harvesting that used.
Keywords: Autogenous bone harvesting, Bone graft, Bowel herniation, Iliac crest, Incisional hernia
Cite this paper: A. Aissat, A. Mesbahi, M. Habarek, A. Bendjaballah M. D., M. Taieb, N. Nait Slimane, R. Khiali, Right Lumbar Incisional Hernia Repair after Iliac Crest Bone Graft: A Case Report and Literature Review, International Journal of Surgical Research, Vol. 6 No. 2, 2017, pp. 25-28. doi: 10.5923/j.surgery.20170602.01.
1. Introduction
- The most common source for autologous bone graft in orthopedics is the iliac crest. It may be harvested from the anterior or the posterior iliac crest. [1] Reported complications include arterial injury, nerve injury, ureteral injury, ileus, hematoma, pelvic instability, fracture, and herniation. [2] Herniation through an iliac crest defect is a very rare but major complication of this procedure. Anatomically, Lumbar hernias are bound superiorly by the 12th rib, inferiorly by the iliac crest, the erector spinae muscle medially, and laterally by the external oblique muscle. The incidence of lumbar hernia after iliac crest bone graft harvesting is estimated to be 5% to 9 %. [3, 4]. This disease is unique for its anatomic specialty and for its rarity, since most surgeons do not have exposure to such a problem. So Surgery is recommended secondary to the 25% risk of incarceration and 10% risk of strangulation with lumbar hernias. [5] We present a case of right lumbar incisional hernia repair using prosthetic mesh.
2. Case Report
- A 68-year-old woman presented with pain in abdomen associated with constipation. Physical examinations revealed a large bulging mass under the right iliac crest scar. The patient had a history of allergy for gentamycin and she undergone bone grafting at the time of total hip replacement 15 years ago. She was treated for cotyloid detachment dating back 10 months of right total hip replacement (cemented femoral stem) + spongy graft (this is more right). The bone grafts were harvested from the right iliac crest. Since 5 months the patient had reported the appearance of painful swelling along her right flank. On examination, a moderately sized, reducible bulge was palpated just under the graft harvest scar along the right iliac crest. Computed tomography (CT) confirmed a large right lumbar hernia containing omentum and a portion of colon located above the iliac crest without evidence of bowel obstruction. (Figure 1). After making a pre-operative investigations which were within normal limits, we performed an open lumbar incisional hernia repair with polypropylene mesh. The defect measured 5 cm × 7 cm and contained omentum and colon, which were easily reduced. The edges of defect were clearly defined and a polypropylene mesh was placed and was fixed to the surrounding muscles with 2-0 prolene. Anchorage of the broad muscles of the abdomen over a width of about 2 cm and over their entire depth to the iliac bone by anchor screws. Postoperative recovery was uneventful. Follow-up at 6 months demonstrated no hernia recurrence by using CT control (Figure 2).
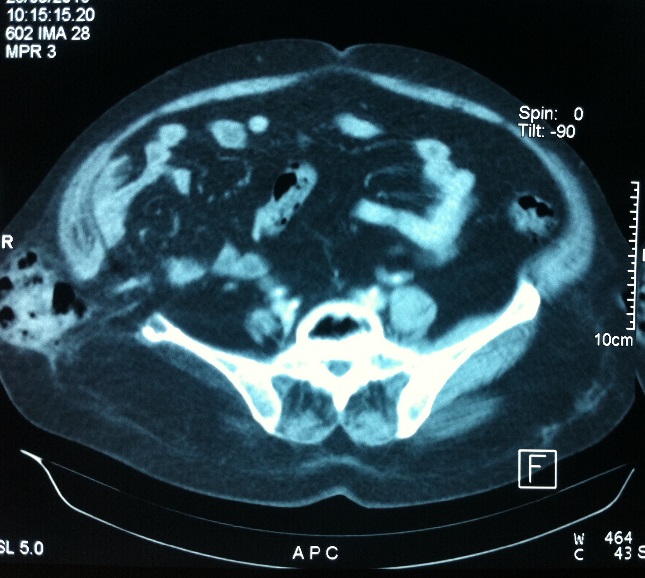 | Figure 1. Computed tomography confirmed a large right lumbar hernia containing omentum and a portion of colon located above the iliac crest without evidence of bowel obstruction |
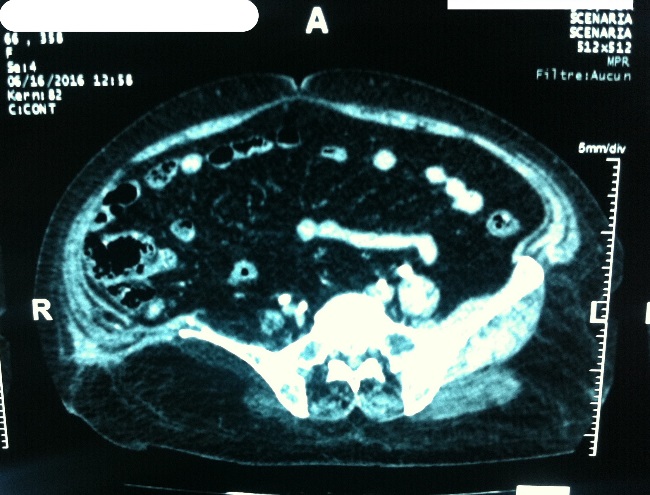 | Figure 2. CT control showing Follow-up at 6 months demonstrated no hernia recurrence |
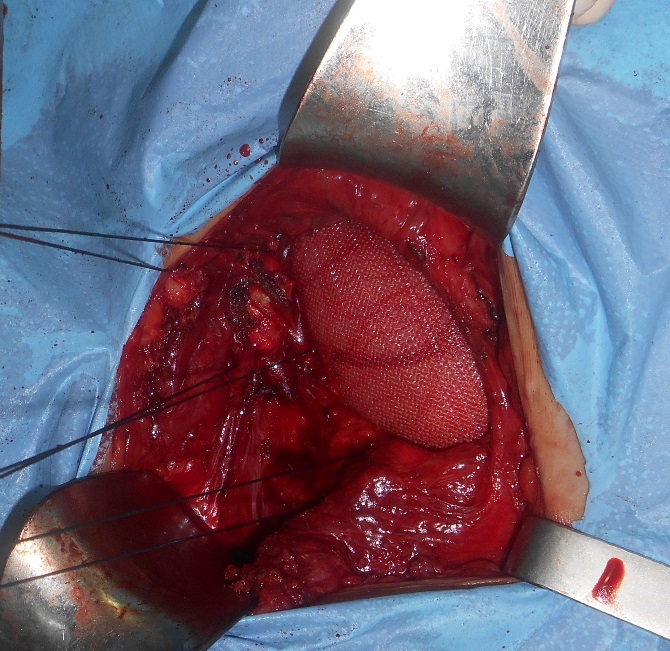 | Photo 1. Showing a wide mesh repair applied to cover the lumbar defect |
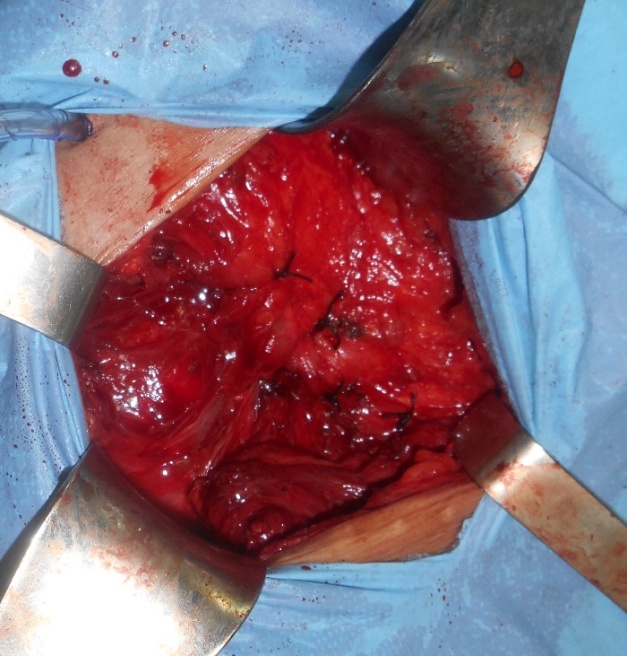 | Photo 2. Showing the end of the procedure coverage and fixation of the mesh |
3. Discussion
- Lumbar hernias are rare with approximately 300 cases described in the literature. [6] In 1945, Oldfield first described hernia through iliac crest bone defect. [7]. In a series of 414 cases, it was seen in two patients (0.5%) [8]. Whereas an incidence of 5 and 9% has been reported by other authors. [9] There is difference between 4 and 5%? They are more common in females, with onset of symptoms ranging from 24 days to 15 years after bone harvest. [10]. They are more frequently seen in females, with onset of symptoms ranging from 24 days to 15 years after bone harvest. [11] Our patient noticed symptoms 10 months postoperatively. A lumbar hernia usually occurs when the full thickness of the iliac bone graft has been removed, or when there is a substantial defect after the bone graft harvesting. Early symptoms include development of a soft-tissue mass associated with discomfort. Clinical examination may reveal bowel sounds on auscultation over the hernia. [11] The lumbar area is a space bordered by: the lower edge of the twelfth rib superiorly, the iliac crest inferiorly, the erector spinae muscle and the lumbar spinous processes medially, and the external oblique muscle laterally. This area is divided into two compartments: superior (Grynfeltt hernia) and inferior triangle (Petit hernia). [12] (This is an anatomical description) The superior lumbar triangle is bordered superiorly by the twelfth rib, the lumbocostal ligament, and the serratus posterior inferior muscle, laterally by the internal oblique muscle, and medially by the erector spinae muscle. The inferior lumbar triangle includes the iliac crest inferior, the external oblique muscle laterally, and the latissimus dorsi muscle medially. [13] Various factors may contribute to the development of these hernias. Bone graft harvesting by itself creates a potential bony defect. The musculoaponeurotic structures get detached during the course of the procedure and remain unsupported despite sutured approximation. However, due to the tension on the non-elastic musculoaponeurotic structures the chances of give way are very high thereby giving rise to a defect resulting in an incisional hernia. The contents of such incisional hernias can vary from cecum to loops of small intestine as seen in our case. Therefore great care needs to be exercised while dealing with the sac and its contents. [14] Signs of bowel obstruction may be present if incarceration or strangulation is involved. Diagnosis is confirmed with CT, which can delineate the anatomy and hernia sac content. Plain radiograph shows the bone defect and sometimes intestinal loops outside the wing of the ileum. The definitive diagnosis can be done with an abdominal CT scan that shows the hernia and its content. [15] CT scan is done early before surgery to make rapid diagnosis and to avoid complications of this hernia-like strangulation and bowel necrosis. (This description of investigation is right as described in the literature)Repairing such hernias can be done by patching up the soft tissue, or by reinforcing the soft tissue with fascial flaps, bone transfer or mesh. The tension-free mesh repair can be performed with a laparoscopic, retroperitoneal or transabdominal approach. [16] Various methods have been described to repair such lumbar incisional hernias, including bone transfer and various soft tissue flaps. The Bosworth repair describes transferring the anterior superior iliac spine inferiorly and posteriorly, drawing muscle and fascia over the defect [17]. The Dowd technique advocates the use of a pedunculated gluteal fascia flap to cover the defect [18]. The Koontz technique involves a lumbar fascia flap for repair [18]. Laparoscopic approach has also been described in the literature [19]. Attaching the mesh to the iliac bone is facilitated by suture bone anchors or corkscrew anchors. Another technique of soft tissue transfer involves using the transversalis fascia, abdominal musculature, and tensor fascia lata. Alternatively, the anterior superior iliac spine can be moved inferiorly and posteriorly to cover the defect in the iliac bone [20]. Laparoscopic approaches have been promoted as providing excellent visualization with the benefits of minimally invasive surgery. [6, 21] Single incision endoscopic surgery has even been described as having favorable results. [22]. However, where the cecum and ascending colon being content of sac this could prove to be dangerous as dissecting the contents could inevitably lead to damage to the colon. Open approach therefore continues to be the safest for such hernias. A wide mesh repair is a procedure of choice. Care needs to be taken that the mesh extends for at least 2.5 cm beyond the defect under the overlying adjacent muscles all around the circumference. The use of suture bone anchors or corkscrew anchors to fix the mesh have been described [23]. The mesh can also be secured to overlying muscle and the periosteum with 2-0 prolene as done in our case. A negative suction drain is placed over the mesh in order to prevent the development of a seroma. I have the impression that the reviewer did not understand the question raised by the article which is very interesting to consider.
4. Conclusions
- Lumbar hernia is a rare complication following iliac bone graft harvest. Various surgical methods have been recommended to prevent such hernia. Ideally, harvesting the full thickness of the bone graft should be avoided. These types of hernias poses an anatomical challenge to the operating surgeon. Preoperative CT scan evaluation provides an excellent tool for planning the repair. Early open repair is advisable as it allows meticulous identification and safe dissection of contents at time of herniotomy. A mesh repair provides adequate strength thereby preventing recurrence. Regardless of its rarity, these hernias should be looked for in each patient who underwent bone graft surgery and who present a lumbar mass. This is a conclusion that deals with the whole subject not just my clinical cas (case report).
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML