-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2017; 6(1): 18-23
doi:10.5923/j.surgery.20170601.03

Acute Bowel Obstruction due to Lesion of the Myenteric Plexus - A Case Report and Review of Literature
A. Bendjaballah, M. Taieb, R. Khiali, A. Haidar, M. R. Oudjit, N. Nait Slimane, R. Bekhouche
Department of General Surgery, Ain Taya Hospital, Algiers, Algeria
Correspondence to: A. Bendjaballah, Department of General Surgery, Ain Taya Hospital, Algiers, Algeria.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Chronic intestinal pseudo-obstruction (CIPO) is a clinical syndrome characterized by chronic and/or iterative episodes and it constitute a heterogeneous group of rare disorders considered by symptoms of intestinal obstruction with no mechanical evidence of obstruction. It is caused by ineffective intestinal contractions due to visceral neuropathy and/or neuropathy. The most common causes are metabolic disorders, connective tissue disorders, neuropathic drug related injuries, paraneoplasic and post-infectious syndromes and amyloidosis. We report a case with a hitherto undescribed lesion of the myenteric plexus, which was demonstrated by histological examination, the lesion mainly involved the small intestine and there is no other associated lesion. The diagnosis was performed by histological studies.
Keywords: Chronic intestinal pseudo-obstruction, Myenteric plexus lesion, Small intestine, Histological examination
Cite this paper: A. Bendjaballah, M. Taieb, R. Khiali, A. Haidar, M. R. Oudjit, N. Nait Slimane, R. Bekhouche, Acute Bowel Obstruction due to Lesion of the Myenteric Plexus - A Case Report and Review of Literature, International Journal of Surgical Research, Vol. 6 No. 1, 2017, pp. 18-23. doi: 10.5923/j.surgery.20170601.03.
1. Background
- Chronic intestinal pseudo obstruction is a clinical syndrome characterized by chronic or iterative episodes evoking a mechanical obstruction of the small intestine, but for which no obstacle is highlighted in .Involvement of the autonomic nervous system is often found as a cause of disturbance of bowel function. The main macroscopic feature was thickening of the bowel wall, which was due to smooth-muscle hypertrophy. This hypertrophy occurs in the absence of normal innervation and is in marked contrast to the atrophy that develops in striated muscle under similar circumstances. It may be produced in the experimental animal by procedures that damage innervation [37], but the mechanism is unknown. The condition is irreversible and should be distinguished from reversible conditions in which the obstructed bowel is dilated but thin-walled. Bowel wall hypertrophy may therefore reflect chronic damage to the myenteric plexus. [1, 2]
2. Case Report
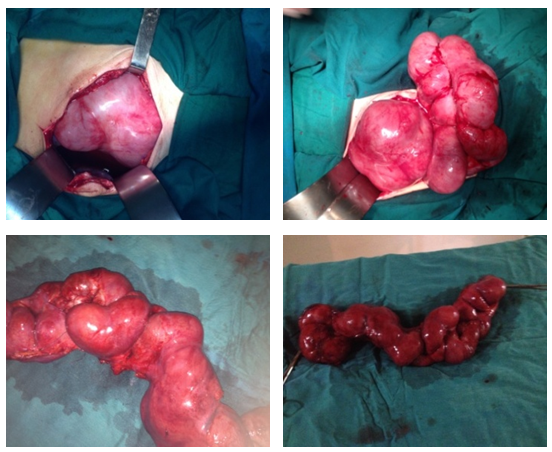
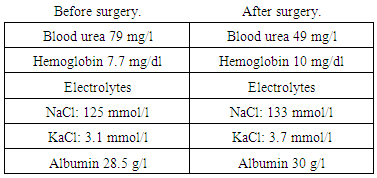
- A 59 years old male was admitted in emergency room for acute bowel obstruction for 04 days. There is no history of the similar symptomatology before and any history of, hemoptysis or melena, or fever but there is history of weight loss, not estimated since several months. General and systemic examination of the patient was characterized by severe dehydration. Examination of respiratory and cardiovascular revealed no abnormality. Rectal examination showed: rectum empty, no evidence of palpable mass was found. The abdomen was distended tender with metallic sound on auscultation. The several abdominal plan erect X ray film showed multiple air levels (Figure 1). Blood examination results showed in the table below
 | Figure 1. Showed multiple air levels |
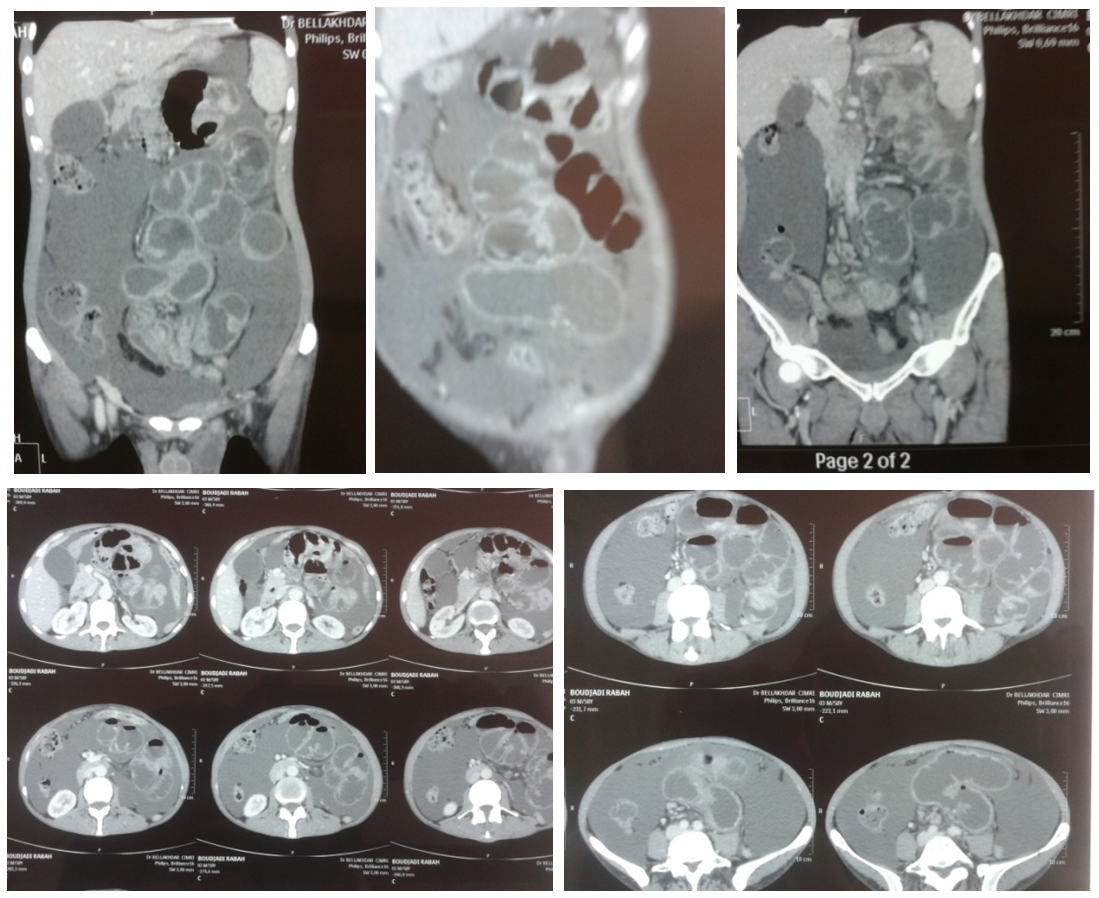 | Figure 2. CT scan showing: ileal and jejunal inflammatory storied stenosis. Inflamed and extended ileitis. Huge amount of ascites |
3. Discussion
- The purpose of our case report is to review the literature about this disease and we hope that will help in the surgical management of this difficult syndrome. Intestinal pseudo obstruction is a clinical syndrome characterized by signs and symptoms of mechanical obstruction without a mechanical origin present. [3, 4]. The most common type of pseudo-obstruction is the acute variety, which has many synonyms paralytic ileus, postoperative ileus and spastic ileus. Acute pseudo-obstruction is usually self-limited and related to operative procedures or acute illnesses, such as pancreatitis, cholecystitis, pneumonia or myocardial infarction. Chronic intestinal pseudo obstruction is much less common and, although it may be secondary to a known systemic disease, such as progressive systemic sclerosis or amyloidosis, it is often idiopathic.Chronic idiopathic intestinal pseudo-obstruction =CIIPO is an increasingly recognized syndrome in which patients usually present with an acute or chronic history suggestive of intestinal obstruction, although no obstructing lesion is found at surgery. In our case the bowel obstruction has occurred in an acute abdominal array. The diagnosis can be suspected in most cases from the clinical presentation. A diagnostic evaluation should be undertaken and exploratory laparotomy avoided if the diagnosis is confirmed on the basis of the radiographic (Showing signs of acute intestinal obstruction) and scanographic data (suspecting an acute bowel obstruction without mechanical cause for this obstruction). If, in the acute presentation, exploratory laparotomy proves unavoidable, and dilated, non-mechanically obstructed bowel is found, a full-thickness biopsy specimen should usually be taken and the abdomen closed. A carefully chosen, palliative procedure should be reserved for patients who have well defined clinicoanatomic patterns of involvement, and who are incapacitated by their symptoms despite medical management [5]. The diagnosis remains very difficult at the beginning before performing a laparotomy.Regardless of cause of CIIP, its pathophysiology involves loss of coordinated intestinal propulsive motility, often throughout the gastrointestinal tract as in our patient. [3]. Although no identifiable disease is present in some patients [6-8] the smooth muscle or myenteric plexus contain morphologic abnormalities in most patients. In addition, many cases are familiar. Hereditary hollow visceral myopathy and familial visceral myopathy are two terms which delineate a form of CIIP caused by smooth muscle degeneration and which is transmitted as an autosomal dominant trait. [9, 10]. Two other forms of CIIP are caused by degeneration of the myenteric plexus. One form of CIIP is familial, involves the central and peripheral nervous systems as well as the intestinal nervous system, and is marked by the presence of an eosinophilic intranuclear inclusion. [11]. The other form is not familial, involves only the intestinal nervous system, and intranuclear inclusions are absent. [12]. The former is called familial visceral neuropathy and the latter is called sporadic visceral neuropathy.Medical management of CIIP is difficult because there is no drug which can restore normal propulsive motility. Anorexia, vomiting, and malabsorption are common and lead to such significant weight loss that some patients must be placed on home parenteral nutrition. Many patients undergo laparotomy either because CIIP is not diagnosed or because a palliative procedure is attempted. [3, 13], despite the fact that these patients often undergo surgery, little is written about CIIP in the surgical literature.Because the natural history of this disease is characterized by remissions and exacerbations, an acute relapse subsequent to an exploratory laparotomy will raise the fear of true mechanical obstruction from the previous operation, thus laparotomy could thereby establish a cycle of repetitive operations. On the other hand, there may not be enough time to establish a diagnosis in a patient presenting for the first time with an acute attack, (as our patient); so that some patients will have exploratory laparotomies during which no mechanical cause for obstruction will be found. [5] As in our case, The presence of disordered peristalsis and muscular hypertrophy may both be explained by a lesion of the myenteric plexus. The clinical signs of distension, visible peristalsis, and hyperactive bowel sounds may also be attributed to this cause. The association of steatorrhoea and malnutrition should be attributed to the stagnant loop syndrome and the direct effects of mechanical obstruction on appetite and delivery of chyme to the small-intestinal absorptive surface. The apparently normal myenteric plexuses do not exclude the diagnosis, since conventional sections of bowel wall may not reveal the lesion. [12] If the diagnosis can be established by finding evidence of widespread abnormal motility in the absence of a mechanically obstructing lesion, an exploratory laparotomy will be unnecessary and, in fact, could be meddlesome.Secondary forms of CIPO have been reported with anti-Hu antibodies. This corresponds to an antineuronal antibody that recognizes a protein expressed in the nuclei of neuron (ANNA-1) and neoplasic cells. The anti-Hu antibody must be searched for in patients over 40 years old with CIPO (associated with small cell lung cancer in 75% of cases). The syndrome of the anti - Hu is one of the most common neurologic manifestations of Paraneoplastic syndromes. It corresponds to the clinical expression of circulating, Antibody directed against the core of neurons in the nervous system central and/or peripheral through nuclear proteins from 35 to 41KD [8]. Syndrome of the anti - Hu is associated with neoplasia in about 85% of cases and, in particular, to lung cancer-small cell (70-80% of cases). [14-16]. Other cancers have been reported (breast, prostate, non-Hodgkin's Lymphoma, Lung Squamous Cell Carcinoma, ganglioneuroblastoma, intestinal or pancreatic endocrine tumor...) [14-18].In 15 to 20% of cases, no neoplasia is found despite periods of close monitoring of ten years and the eventual practice of necropsy [14, 16]. The prognosis of the syndrome of the anti - Hu is generally pejorative (47% of survival at one year, 12% of five-year survival) and more often related to neurological damage (60% versus 40% linked to tumor progression) [14]. Anyway, antitumor treatment is a factor of prognosis of survival, with or without an immunomodulatory treatment [14]. On the other hand, only five cases of syndrome of the anti - Hu manifesting in the form of a CIPO have been reported [20, 21-23]. In two recent studies, the findings of three cases of CIPO called idiopathic neurogenic, associated with an aganglionnose and lesions of inflammatory visceral neuropathy (neuronal and axonal degeneration, dense Lymphocytic infiltrate), helped to highlight a humoral response associated with significant positivity of antibodies anti - Hu [20] in young patients without factor of risk for malignancy and especially lung cancer-small cell. Two hypotheses are currently evoked to explain the existence of a syndrome of the anti - Hu in the underlying lack of neoplasia. The first is based on the possibility of tumor regression of immune, mediated by antibodies anti - Hu. This hypothesis is based on isolated observations of spontaneous tumor regression associated with the existence of a syndrome of the anti - Hu [24], and by the fact that patients with syndrome of the anti - Hu have generally little evolutionary tumors confined to the mediastinum, often of small size, whose morbid evolution is more the fact of neurological damage to the cancer itself [14]. The second is based on the possibility of an autoimmune, non Paraneoplastic process [25]. The treatment of this sever pathology still not clear; recent studies proposed some measures” to be effective”, divided in two methods: the first one is medical comporting Prokinetic agents (Metoclopramide and Domperidone erythromycin Octreotide Prostigmine), systemic sequential antibiotherapy, nutritional assistance, lifestyle measures with dietary oral supplements, artificial nutrition (feeding) and gastrostomy aspiration [26]. Others authors suggest: reduction of neurodegeneration, Neurotrophic factors (BDNF, GDNF, NT-3), maintenance of neuronal pool, reduction of apoptosis factors, improvement of the motor in a model of diabetic mouse (BDNF), improvement of constipation in humans (BDNF and NT-3) [27-29]. This measures are followed by Agonists of 5HT (improved growth and survival of neurons myenteric as well as a reduction of the phenomena of apoptosis through an agonist 5HT (4): Tegaserod, Prucaloprid). [30, 31]. The perspective for the future is marked by: culture of stem cells from the neurologic extrinsic system by endoscopic biopsies, transplantation and implantation of stem cells in an aganglionic tissue [32]. The second way is the surgical support which have potentially deleterious and limited role in support of CIPO, the place of laparoscopy is not yet well defined. Surgery is essentially palliative (derivations, gastrostomy, jejunostomy, and/or Ileostomy; intestinal resections: limited or extended), subtotal enterectomy and intestinal transplantation. [33, 34].The use of the intestinal transplantation in the treatment of this pathology are not so important until now (only 13% of cases) and the indications are resumed to: permanent intestinal pseudo obstruction with updated in-game of the vital prognosis related to the parenteral nutrition= PN (feeding) and/or possibility of compromised PN, severe intestinal pathologies and precariousness of the quality of life. [35, 36]Concerning our case this is a very rare case of acute intestinal occlusion which revealed a rare lesion of the Myenteric plexus of intestine. There is no way for medical treatment for our patient because he presented with acute abdominal obstruction for four days duration.Concerning the follow up our patient was not reviewed in OPD after surgery.
4. Conclusions
- The acute intestinal obstruction by lesion of myenteric plexus is rare, serious with difficult diagnostic. Its difficulty lies in the elimination of the obstacle while knowing avoid surgery. Digestive and nutritional symptomatic treatment is essential. An operative procedure may be one possible answer. Who have procedures for defined clinicoanatomic patterns should be thoroughly studied beforehand, have regular follow-up examinations, and reported in the literature. Only with more data will we know whether any operative procedure will help to improve the quality of life of these patients.Recent advances in pathophysiology and diagnosis, with persistence of some importance of idiopathic CIPO. Growing interest in intestinal transplantation as well as targeted therapies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML