-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
p-ISSN: 2332-8312 e-ISSN: 2332-8320
2017; 6(1): 1-4
doi:10.5923/j.surgery.20170601.01

Duplex Ultrasound Guided Catheter Directed Foam Sclerotherapy for Treatment of Axial Varicose Veins of the Lower Limbs and Its Preliminary Results
Mohamed Saad Saleh
Vascular Surgery Department, Faculty of Medicine (Boys), Al-Azhar University, Cairo, Egypt
Correspondence to: Mohamed Saad Saleh, Vascular Surgery Department, Faculty of Medicine (Boys), Al-Azhar University, Cairo, Egypt.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Catheter directed foam sclerotherapy for treatment of lower limb varicose veins guided by duplex ultrasound is an important option in management of varicose veins. This prospective clinical study underwent in Al-Azhar University Hospital Vascular Surgery Department 73 patients with great or lesser saphenous venous reflux between July 2015 and July 2016 all the patients were treated by catheter directed foam sclerotherapy and the result was initial technical and clinical success of more than 92% and also preliminary result was satisfactory with higher rate of vein occlusion by fibrosis. So catheter directed foam sclerotherapy under ultrasound guided is a safe procedure with high clinical success and lower complications rate.
Keywords: Duplex ultrasound, Lower limbs, Catheter directed foam sclerotherapy
Cite this paper: Mohamed Saad Saleh, Duplex Ultrasound Guided Catheter Directed Foam Sclerotherapy for Treatment of Axial Varicose Veins of the Lower Limbs and Its Preliminary Results, International Journal of Surgical Research, Vol. 6 No. 1, 2017, pp. 1-4. doi: 10.5923/j.surgery.20170601.01.
Article Outline
1. Introduction
- The indications of foam sclerotherapy in the management of varicose veins have rapidly increased over the last decades [1]. Foam sclerotherapy is effective in treatment of axial vein (great and lesser saphenous veins). It does not require anesthesia or attending operating room as well as it has a very acceptable safety profile [2].Duplex ultrasound guidance plays an important role in assessment of anatomical variations, precise foam delivery and confirms patency of the deep venous system [3].The sclerosant material causes irreversible disruption of the endothelial cell membrane resulting in vasospasm, which ends as fibrous obliteration of the vein lumen [4].Many reports and trials documented the beneficial effect of foam sclerotherapy in refluxing long axes veins [5].However, it has some limitation, especially for high risk patients for deep venous thrombosis, history of allergy to the sclerosant material and in patients with limited mobility [6]. This study is done to introduce the sclerosing material through the catheter to stimulate maximum vein spasm minimizing the drug dose, and to be sure that all vein segments has direct contact with the drug with maximum opportunity to occlude the vein and abolishing the reflux.
2. Material and Methods
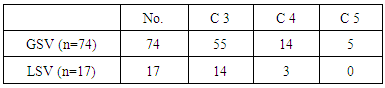
- Between July 2015 and July 2016, 73 patients were treated for primary varicose veins as a chronic venous insufficiency with proven great saphenous vein (GSV) (n=74) and lesser saphenous vein (LSV) (n=17) and outcomes reported. The median age was 37 (23-48 years) and 56% were females. Clinical data of the patients are demonstrated in table (1).
|
3. Technique
- After careful history and physical examination for the patients complaining of pain and swelling of the lower limbs. Duplex ultrasound should be carried out for all patients to confirm diagnosis of venous reflux and to rule out deep venous thrombosis as well as to localize sites of perforators.The color duplex ultrasound (Mindray DC8, China) with high resolution transducer (10 MHz) was used in all cases.The duplex study was done while the patient is in standing position to assess reflux in the deep veins, confirm and localize degree of axial reflux.The patient has to rest in a head up position on the examination table to facilitate the vessel puncture or lying prone to puncture the proximal LSV.The desired puncture site of GSV is 5cm below the knee while puncture of LSV is behind the lateral malleolus.Sterile draping of the ultra sound probe and access side is performed using small amount of Xylocaine 2% to infiltrate the access site while keeping the patient covered in a warm room to acquire a maximum dilatation of the vein.Ultra sound guidance of the punctured site with 18 G standard vascular access needle taking in consideration the multiple puncture trials reduce the opportunities of proper cannulation.After successful cannulation, a standard guide wire 035 is inserted into GSV or LSV and advanced under ultra sound guidance to reach the saphenofemoral junction of saphenopopliteal junction then small stab skin incision to allow a 5 French straight tip angiography catheter to pass over the wire.Then the patient is kept in horizontal position with elevation of the leg 30degree, make sure the tip of the catheter is at 1 to 2cm distal to the junction of the deep veins.The presence of the catheter inside the vein together with leg elevation allows the vein to reach its maximum vasospasm thereby increase vessel wall contact of the sclerosant material.Preparation of the sclerosant foam using 2% polidocanol solution (Aethoxysclerol) using the three way cannula according to Tessari methods in a liquid-air ratio of 1:4 as shown in figure (1). So two ml of 2% polidocanol gives 10ml of foam.
 | Figure (1). Tessari method |
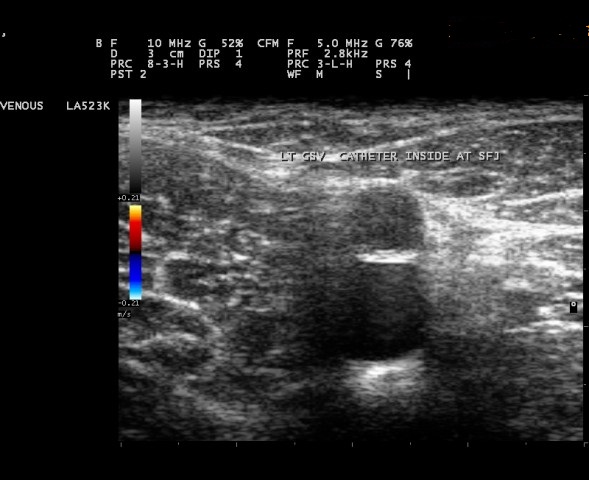 | Figure (2). Catheter beyond saphenofemoral junction |
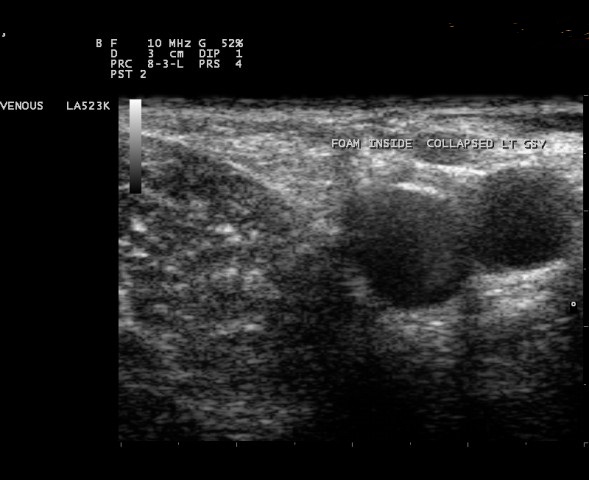 | Figure (3). Foam inside great saphenous vein |
4. Results
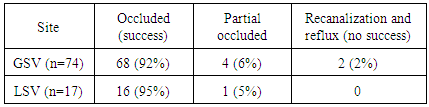
- Between July 2015 to July 2016, 73 patients with GSV and LSV reflux subjected to catheter directed foam sclerotherapy at Al-Azhar University Hospital Vascular Surgery Department Primary initial success with foam sclerotherapy was obtained and achieved in 91 limbs of 73 patients.In six patients there was a failed puncture of the vein due to repeated attempt with subsequent venous vasospasm and venous cut down was performed through a small stap incision.Two female patients developed vasovagal attack and the procedure postponed to another day.Two patients developed chest discomfort, visual disturbances and dry cough which resolved by O2 mask and reassurance. No immediate complications from treatment occurred.The GSV and LSV were examined by duplex ultrasound after one week to assure its obliteration and it was achieved in all patients.12 patients developed painful thrombophlebitis after one week that required low molecular weight heparin for 10 days.Color duplex was done after 3 months and the result of the study is demonstrated in table (2).
|
5. Discussion
- This prospective study on 73 patients treated with catheter directed foam sclerotherapy for axial vein reflux in the lower limbs is showed a high initial success as described by other studies.The chest discomfort, visual disturbances and dry cough was very low representing 2 patients out of 73 patients, (less than 3%) as documented and observed in other studies in up to 14% of the patients [7].This very low incidence of early side effect of foam sclerotherapy in this study may be due to the vasospasm of the treated vein which induced by presence of the catheter and also manual compression at the saphenofemoral or saphenopopliteal junction using duplex probe that keep the foam to be inside the superficial venous lumen and prevent escape of the foam to the deep venous system.The clinical success rate and assessment of treated vein reflux at three months follow up as preliminary results are comparable to other reported studies on foam sclerotherapy through direct puncture of the axial veins [6-8].However this study showed a number of advantages, the vasospasm of the vein is maximum due to presence of the catheter inside the vein lumen.The limb elevation and low injection pressure are two important factors in distribution of the foam inside the whole vein length which is not predicted in direct vein puncture [9, 10]. Also in this study minimal amount of foam needed with minimal pressure and this allow efficiency of the technique and diminished incidence of thromboembolism [11].However, the absence of burses, post procedure pain and no requirement of anesthesia are advantages of catheter directed foam sclerotherapy.Further studies are required to assess and explain the migration of foam into the common femoral vein; to assess the leg elevation and manual compression provide any advantages.
6. Conclusions
- In conclusion, the catheter directed foam sclerotherapy is accepted as an option of foam sclerotherapy with initial and short term success in vein obliteration and has a very low numbers of complications.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML