-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2015; 4(1): 7-9
doi:10.5923/j.surgery.20150401.03
Intra-Medullary Primary Spinal Cysticercosis: A Case Report
Sanjay Surase1, Ashwini Natekar1, Sanjay Bijwe1, Vernon Velho2, Rahul Tiwari2, Vaishali Solanke3
1Department of Pathology, Grant Medical College and J J group of Hospital, Mumbai, India
2Department of Neurosurgery, Grant Medical College and J J group of Hospital, Mumbai, India
3Department of Microbiology, Seth G.S Medical College and KEM Hospital, Mumbai, India
Correspondence to: Vaishali Solanke, Department of Microbiology, Seth G.S Medical College and KEM Hospital, Mumbai, India.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
We describe a rare case of intra-medullary form of primary spinal cysticercosis. A 40 year male, resident of Mumbai and a taxi driver by occupation presented with radicular pain and weakness in left lower limb since 3 months with urinary retention and dribbling micturation since 1 month. MRI showed a large intra-medullary lesion in the conus/ epiconus area and was diagnosed as intra- medullary granulomatous pathology. The patient underwent surgery for the same. Intra-operatively a mass was identified in the conus which was light brown to gray in color and firm in consistency with small pus pockets. Part of the lesion was sent for frozen section and reported as inflammatory lesion. Then the mass was excised en block and sent for histopathological examination. We received a single tissue bit measuring 1cmx0.6cm, grayish white and soft in consistency. On histological examination the section showed a parasite surrounded by mixed inflammatory infiltrate and was confirmed as cysticercus larva. As there was no intracranial lesion, the final diagnosis was primary spinal cysticercosis. Cysticercosis at the conus/ epiconus region of the spinal cord is rarely seen.
Keywords: Intra-Medullary, Spinal, Cysticercosis
Cite this paper: Sanjay Surase, Ashwini Natekar, Sanjay Bijwe, Vernon Velho, Rahul Tiwari, Vaishali Solanke, Intra-Medullary Primary Spinal Cysticercosis: A Case Report, International Journal of Surgical Research, Vol. 4 No. 1, 2015, pp. 7-9. doi: 10.5923/j.surgery.20150401.03.
1. Introduction
- Cysticercosis is the most common parasitic disease affecting the human central nervous system and is caused by Taenia solium. In all patients with neurocysticercosis (NCC) the spinal involvement is uncommon (1-3% of all cases). [1] Neurocysticercosis can be categorized into parenchymal, leptomeningeal, intraventricular or spinal cysticercosis according to the location of the lesions. [2] About 80% of spinal cysticercosis are intradural-extra-medullary forms. [3,4] The intra-medullary type is quite rare and only 54 cases have been reported until 2012. [5-10]
2. Case Report
- A 40 year old man, resident of Mumbai and a taxi driver by occupation presented with complaints of radicular pain and weakness in left lower limb since 3 months with urinary retention and dribbling micturation since 1 month. CSF examination was within normal limits. MRI of the spine was done which showed a large intra-medullary lesion in the conus/ epiconus area, with diffuse contrast enhancement on post contrast study. Hence radiological diagnosis of intra-medullary granulomatous pathology in conus / epiconus area was suggested.Patient underwent surgery for the same. Intra operatively a mass was seen in the conus which was light brown to gray in colour and firm in consistency. There were also seen small pus pockets in the lesion. A small tissue was sent for frozen section. The squash cytology report was suggestive of inflammatory lesion. However confirmatory diagnosis was awaited for histopathological examination. Further the mass was excised en block and sent for histopathological examination.We received a small tissue bit measuring 1cmx0.6cm, which was grayish white and firm in consistency. On histopathological examination, multiple sections study demonstrated the cystic wall consisted of an outer cuticular layer with brush like border, an epithelial like intermediate layer, and an inner reticular layer made up of a canaliculi network. The scolex was not been identified along with numerous congested thick and thin blood vessels. Hence the diagnosis of spinal cysticercosis was confirmed.Post operatively the patient showed marked improvement in pain and a complete cranio-spinal MRI evaluation excluded any other cysticercus lesion.
2.1. Figures
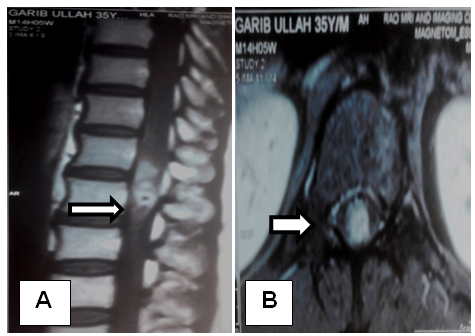 | Figure 1. Pre- operative MRI of spine showing the lesion ( A – Sagital section, B – Coronal section) |
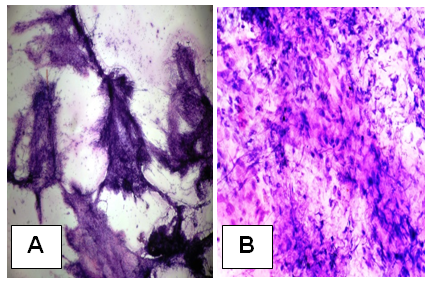 | Figure 2. Squash cytology showing granulomatous inflammation (A – 4X magnification, B – 40 X magnification) |
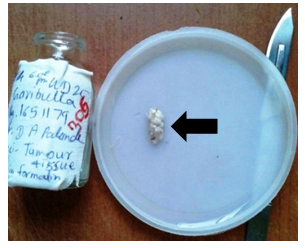 | Figure 3. Gross appearance of the mass |
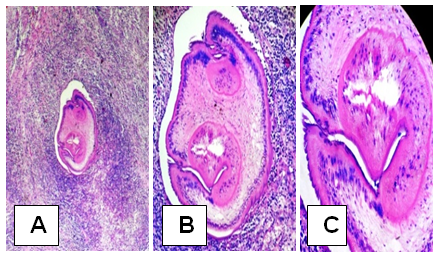 | Figure 4. H & E stain showing Larva of Cysticerus with surrounding granulomatous inflammation (A – 4X magnification, B – 20 X magnification, C- 40X magnification) |
3. Discussion
- Cysticercosis is widely endemic in Brazil, Peru, Mexico, Korea and India. [11,12] Intra-medullary cysticercosis often presents in the patients between 20 and 45 years old, with the youngest one reported being 5 years old and the oldest one 45 years old. [13] The common clinical manifestations included pain, paraparesis, spasticity, bowel and bladder incontinence and sexual dysfunction [5,12]. Most patients experienced a progressively worsened course from a week to 10 years.Inside the spinal cord, cysticercus usually distributes in the thoracic cord, with a few cases involving the cervical and the lumbar cord. This distributional mode of cysticercus supports the hypothesis that intra-medullary cysticercus comes from the blood circulation, because thoracic cord has a richer blood supply than the other parts of the spinal cord. [4, 12] However, it is also thought that intra-medullary cysticercus could migrate to the spinal cord via the ventriculo-ependymal pathway.MRI is a sensitive diagnostic tool for the identification of cystic lesions in the spine; however it is difficult to distinguish cysticercosis from a non-infectious cyst. Contrast enhanced MRI is mandatory for evaluating spinal cysticercosis. [14]The differential diagnosis of an intra-medullary cystic lesion is extensive, including some other cysts such as arachnoid cyst, [17] ependymal cyst, [18] neurenteric cyst, [19] sarcoidosis, [20] neoplasms such as ependymoma and infections such as abscess. [21]If patient has a history of cysticercosis and/or hails from an endemic region and MRI reveals a cystic spinal cord lesion, the diagnosis of intramedullary cysticercosis should be suspected and be further verified by serologic alterations, subcutaneous nodules and/or changes in the cerebrospinal fluid. The CSF examination often shows increased proteins, a low or normal glucose, moderate lymphocytic pleocytosis and eosinophilia. [22] Cysticercal antibodies found in CSF either by ELISA or in serum by enzyme linked immunoelectrotransfer blot assay have good sensitivity and specificity in cysticercosis diagnosis. [22, 23]Our patient did not belong to endemic region of cysticercosis nor had any previous history of the same. Due to the neurological deficit surgery was considered a primary line of treatment and also for confirming the diagnosis on histological examination. Post operatively our patient showed improvement in pain.In the reports published in recent years [5, 6, 13] surgical outcome has significantly improved; with no reported death and the majority of patients living a life without special support. Surgery is considered the procedure of choice only when diagnosis is in doubt otherwise medical treatment has its advantages. Albendazole is normally used postoperatively as a regular treatment (15mg/kg/day) for 4 to 6 weeks, according to the idea that cysticercosis is a generalized disease with focal manifestation.
4. Conclusions
- In conclusion, intra-medullary cysticercosis represents a diagnostic challenge and neurocysticercosis should also be strongly considered for intra-medullary cystic lesions, even in a non-endemic area. Surgery is the mainstay of treatment as it helps in excision of lesion, decompress the cord as well as provide definitive histopathological diagnosis.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML