-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2013; 2(4): 52-55
doi:10.5923/j.surgery.20130204.06
Annular Pancreas: A Case Report in Buea Regional Hospital (Cameroon)
Ngowe Ngowe M1, Weledji E1, Mouafo Tambo FF2, Verla V1, Sosso MA3
1University of Buea, Républic of Cameroon
2University of Yaounde I (UYI), Républic of Cameroun
3Head of Department of surgery and specialities, Faculty of Medicine (UYI). Surgical Unit, Buea Regional Hospital - South West Region, Cameroon
Correspondence to: Ngowe Ngowe M, University of Buea, Républic of Cameroon.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Annular pancreas is a congenital malformation in infants and children and even adults, affecting the duodenum and that may cause a sub and or occlusive syndrome. The treatment of this anomaly is surgery often yielding a good prognosis. We report a unique case of this rare condition in a 2 years old girl, described for the first time in the south west region of Cameroon.
Keywords: Annular Pancreas, Infant Gastrojejunal Anastomosis
Cite this paper: Ngowe Ngowe M, Weledji E, Mouafo Tambo FF, Verla V, Sosso MA, Annular Pancreas: A Case Report in Buea Regional Hospital (Cameroon), International Journal of Surgical Research, Vol. 2 No. 4, 2013, pp. 52-55. doi: 10.5923/j.surgery.20130204.06.
1. Introduction
- Annular pancreas is a congenital anomaly in which the pancreas forms a complete or incomplete ring at the second portion of the duodenum, causing partial or complete stenosis and / or localized atresia. Annual incidence of annular pancreas is variable: estimated 1 in 12,000 to about 1 in 50,000 births, this condition represents 10% of duodenal stenosis[1]. So this is a rare condition. Our rural hospital in the South West Region of Cameroon (West Africa) is less equipped in regards of modern tools of investigations. Nevertheless among activities, surgery occupies an important part dealing mainly with emergencies; this is why we consulted a young patient with a suspected case of duodenal obstruction that showed latter run as an annular pancreas, a rare congenital defect that has been little or no described at all in our milieu. It therefore seemed necessary to remedy this situation by reporting this unique case observed for the first time in the Buea regional hospital.
2. Observation
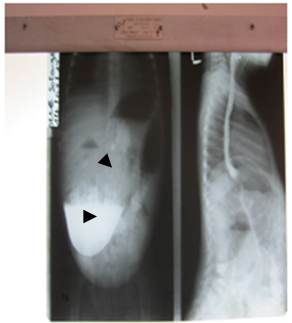
- The child O.S. female, 2 years old was taken in consultation for fatigue, recurrent postprandial vomiting and flatulence, all lasting for eight days. It was also noted a lack of appetite, weight loss. History of the disease showed that in the first week of life, postprandial non bilious vomiting was present as well as obstinate constipation. Constipation sometimes alternated with diarrhea. Parents then privileged successive enema and traditional medicine treatments. In the past history, the mother was G5P5005 and followed prenatally at the Buea regional hospital (south west region of Cameroon) with a normal 8 months pregnant ultrasound and had followed the normal programmed vaccinations; HIV serology, syphilis and TORCH were all negative. The pregnancy was terminated by a normal delivery at term of a baby girl with an APGAR of 10/10, a birth weight of 2.800 kg. Upon arrival in surgical ward, physical examination showed a young patient asthenic, undernourished. The weight was 8 kg, the heart rate of 90 beats / min, respiratory rate of 50 cycles / min and MUAC of 12 cm. Conjunctivae were slightly pale. The abdomen was distended and had epigastric peristaltic waves visible in oblique light. Abdominal lazy skinfold was observed; no organomegaly. The digital rectal exam brought some soft and greenish stools, odorless. No congenital anomalies had been noted on physical examination (negative VACTERL). The neurological examination was normal. Complementary tests showed hypochromic anemia with a hemoglobin level of 9g/dl. Contrast barium meal had shown the classic "double bubble"sign (Fig. 1, 2 and 3). Abdominal ultrasound revealed an enlarged stomach pouch, stasis, normal pylorus with increased peristalsis in the antrum suggesting stenosis of the second portion of the duodenum. A barium enema requested was not done. On the basis of probable atresia and / or duodenal D2 stenosis, the patient was prepared for corrective laparotomy. The young patient was operated under general anesthesia with endotracheal intubation. A lateral transverse incision was made above right umbilical side. Laparotomy revealed a fight stomach, very dilated, a normal pylorus, a significant dilatation of the first and second portions of the duodenum. The jejunum and ileum were of normal size and the exploration of otherintra-abdominal organs revealed no abnormalities (congenital among others). Exploration of the duodenum revealed a pancreatic portion encircling the duodenum on its front side and outer side: there was evidence of an incomplete annular pancreas (Fig. 4, 5, 6) responsible for sub-occlusion. Surgery consisted in the realization of a side to side gastro-jejunal anastomosis. Closure of the abdomen was made layer by layer without drainage. The immediate outcome was uneventful and the patient was discharged eight days after surgery.
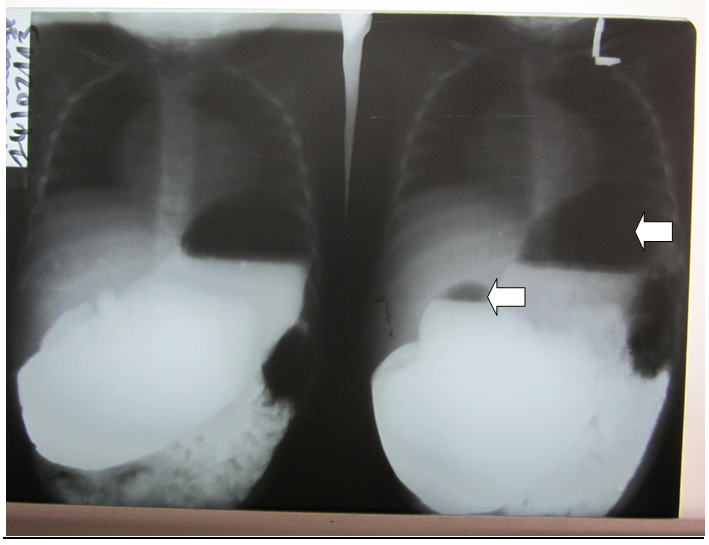 | Figure 1. Contrast Barium meal “double bubble” sign, front view |
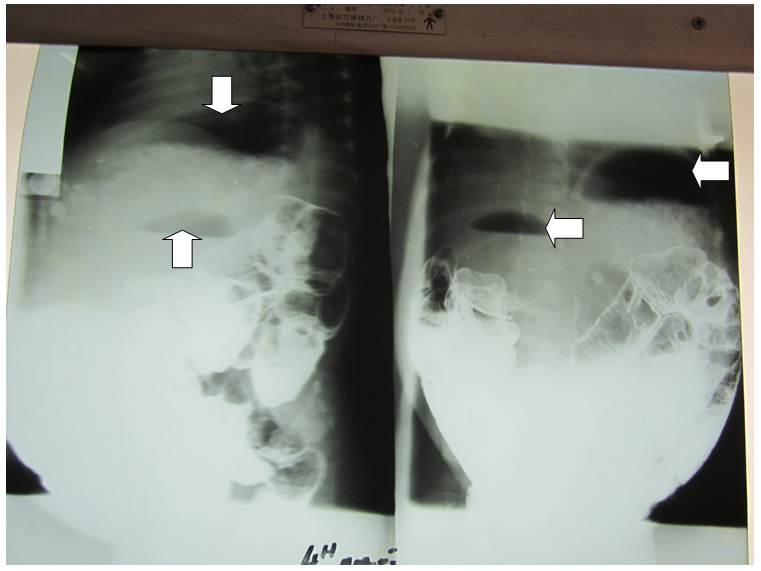 | Figure 2. persistence of the “double bubble” sign, after 4 hours |
 | Figure 3. lateral view of the “double bubble” sign |
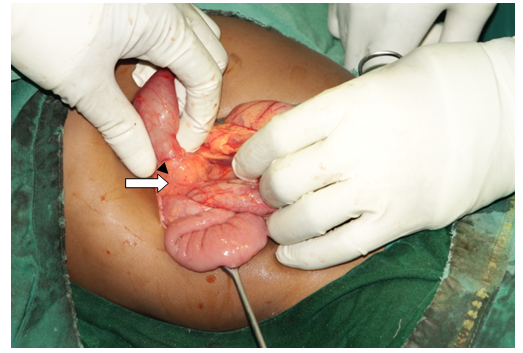 | Figure 4. annular pancreas (arrow). Laparotomy view |
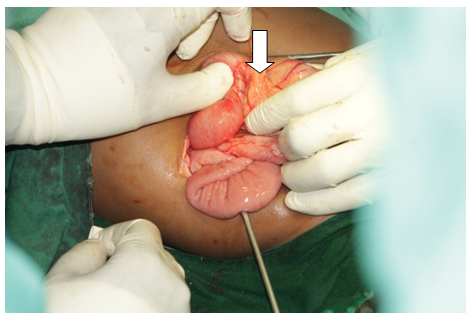 | Figure 5. brownish aspect of the annular pancreas (arrow) |
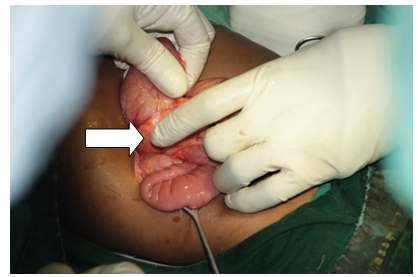 | Figure 6. partial and lateral view of the annular pancreas (arrow) |
3. Comments
- Annular pancreas is a result of early abnormality that happens at the fourth week of intrauterine development. This congenital abnormality which is a particular form of duodenal atresia may be associated with many other defects. Chromosomal abnormalities are present in one third of cases, the most common being Down syndrome, trisomy 21 (then 18 and 13)[2]. Malformations of the cranial gut are frequently associated[3], heart disease are also often found. [4] This condition appears more common in females as stated by Zyromski[5]. Neonatal symptoms are dominated by the existence of epigastric distension, accompanied by non bilious vomiting since the obstruction is beyond the Vater bulb: this was found in our reported case and had been previously described by Papandreou in Athens, Greece in 2004[6]. Most often, diagnosis is made before the birth through observable duodenal dilatation on ultrasound and the difficulty to show the peri-duodenal pancreatic development. If the diagnosis was not made before the birth, it is made in the neonatal period or later as in our case. It is based on the clinical and imaging tests (abdomen radiography, ultrasound): here the classic image of double bubble takes on its full meaning.[7] The differential diagnosis includes other forms of duodenal stenosis. Prenatal diagnosis allows immediate treatment in a specialized center [7]. Introduction of a nasogastric tube can drain the digestive tract upstream of the obstacle. Surgical treatment is made by a bypass (laparotomy or laparoscopy) of the obstacle using duodeno-duodenostomy, most often duodeno-jejunostomy or gastrojejunostomy as in our case[8]. The prognosis is very good and is related to the presence or absence of associated malformations.
4. Conclusions
- We reported this rare case of an annular pancreas discovered during surgery for a suspected duodenal stenosis. This was very interesting because that was the second case ever reported in our country in Cameroon for the past 30 years. Again, it was very exciting because this happened in a rural hospital where means of diagnosis were underdeveloped, making it almost impossible to have an obvious preoperative diagnosis of that congenital abnormality as it is done in developed countries. Finally, it was very useful for teaching purpose for our medical students and enhancing the scientific quality of the knowledge of that congenital defect in our milieu.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML