-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2013; 2(4): 48-51
doi:10.5923/j.surgery.20130204.05
Role of Laser Depilation in Treatment of Pilonidal Sinus Disease
Ayman F El-Ramah1, Hanan M Darwish2
1Department of General Surgery, Faculty of Medicine (Damietta branch), Al-Azhar University, Egypt
2Department of Dermatology, Faculty of Medicine for Girls, Al-Azhar University, Egypt
Correspondence to: Ayman F El-Ramah, Department of General Surgery, Faculty of Medicine (Damietta branch), Al-Azhar University, Egypt.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Background: Pilonidal sinus is a chronic disease affecting mainly men from puberty to their early thirties. Surgical treatment has significant failure rate, and recurrence is common. Excessive hair growth in the natal cleft is thought to be a factor in initiating this disease. Objective: To evaluate the role of Laser hair removal following surgery in treatment of pilonidal sinus. Methods: 18 patients with pilonidal sinus were treated initially by open surgery followed by division into two groups; Group A using Laser hair depilation in the natal cleft following pilonidal sinus surgery, Group B using the conventional methods for hair removal. Results: Group A patients received the full course of treatment of Laser (4 sessions, 6-weekly) after surgical treatment. None of the patients developed recurrent disease at 1-year follow up and, none have required further surgery. Group B patients showed recurrence in 4 patients. Conclusion: Our results strongly suggest that Laser hair removal after surgical interventions in pilonidal sinus disease decreases the rate of recurrence and should be advised to all patients. However; larger studies are needed to ensure this adovacation.
Keywords: Pilonidal Sinus, Laser Depilation, Excesive Hair Growth
Cite this paper: Ayman F El-Ramah, Hanan M Darwish, Role of Laser Depilation in Treatment of Pilonidal Sinus Disease, International Journal of Surgical Research, Vol. 2 No. 4, 2013, pp. 48-51. doi: 10.5923/j.surgery.20130204.05.
Article Outline
1. Introduction
- Pilonidal sinus disease (PSD) is a painful disorder usually found in the natal cleft; it is diagnosed by the presence of a characteristic epithelial track between the buttocks . The sinuses may be caused by hair growing into the skin where there is excessive body hair or if tight clothing is worn, and is often seen in occupations that involve sitting for long periods[1]. PSD is a problem suffered mostly by young men, with an incidence of 26 per 100,000 population, affecting men twice as often as women[2] with symptoms of recurrent infection of the area of the natal cleft[3]. The clinical presentation of the disease varies from asymptomatic pits to painful draining abscesses and chronic fistulae. The most common manifestation of pilonidal disease is a painful fluctuant mass in the sacrococcygeal region[2].Many treatment options for pilonidal sinus have been reported including , antibiotics, drainage, and excision surgical treatment. Different modalities of surgery have been used, but they often result in recurrence, and additional surgery is needed[4]. Laser hair epilation in the affected area have shown beneficial effect by decreasing the risk of recurrent pilonidal sinus disease[5].Laser depilation is used in a number of medical conditions, such as ingrown hairs, hirsutism (male pattern of hair distribution in females), and folliculitis (inflammation around the hair follicle), as well as PSD. Lasers emit specific wavelengths of light that are absorbed by a different colour in the tissue, known as chromophore, and are converted into heat. The chromophore for laser hair removal is melanin; since this is lacking in light hairs, laser hair removal treatments are better suited to people with darker hairs[6].Laser has been available as a permenant method for hair removal[7]. Multiple sessions are often needed and seem to increase progressively the hair free period between sessions and decrease hair regrowth[8].
2. Patients and Methods
- This study was done on 18 patients, 16 males and 2 females with pilonidal sinus attended to out patient’s clinic in Al Azhar university hospitals and other hospitals .Age of patients ranged from 17– 30 years. 11 Patients had primary disease and 7 had recurrent disease. All of patients underwent surgical intervention by open technique in which the whole sinus was excised and the wounds left open for healing by secondary intention. After complete wound healing , patients were divided into 2 groups: Group A: 9 patients were treated with alexandrite Laser for hair removal after application of local anesthesia cream eutectic mixture of prilocaine 2.5% and lidocaine2.5% (EMLA CREAM). The Laser system protocol was:1-Laser system: Cynosure Apogee 55002-Wavelength (nm): 7553-pulse duration (ms): 34-Fluence (J/cm2):18-20 according to skin type of each patient.5-spot size (mm):12 -156-sessions (n):3- 57-Time interval (weeks):4-6Group B: 9 patients were using traditional methods for hair removal (shaving, and hair removal creams).All patients were followed up for about one and half years, every 2 months for 6 month, and every 3 months for 1 year.Written informed consent from all study patients was taken.
3. Statistical Analysis
- All statistical calculations were done using computer programs.Microsoft excel version 10 and spss (statistica package for the social science version 20.00) statistical program. at 0.05, 0.01 and 0.001 level of probability [9] .Comparison of percentage was done using the t test and chi square were presented using percentage, mean ± standard deviation. The Pearson linear correlation coefficient was estimated to show the relationship of the physiological parameter to each other[10].
4. Results
- Demographic data, type of lesion, method of hair removal and recurrence after treatment were shown in table 1.Our study was done on 18 patients, 16 were males (89%) and 2 were females (11%) with age ranged from 17 to 30 years, with a mean age of 22.3+0.7 years. 11 patients(61.1%) had primary lesion, while 7 patients (38.9%) had recurrent lesion. Group A patients had a mean age 21.33±3.94 years, 8 (88.9%) were males, 5 (55.6%) were primary cases and 4(44.4%) were recurrent. Patients in Group A underwent Laser hair removal at the natal cleft after complete wound healing and according to the explained protocol. Group B patients had a mean age 23.33±3.60 years, 8 (88.9%) were males, 6(66.7%) were primary cases and 3(33.3%) were recurrent. Group B patients use the traditional methods for hair removal (table 2, 3),(Figure 1,2). Patients in Group A mentioned that the Laser hair removal was comfortable with no complications while those in group B reported difficulty in maintaining hair removal at regular periods.Recurrence occurred in 4(44.4%) in Group B while there were no recurrence in Group A and this difference was statistically significant. (Table 3), (Figure 3)
|
|
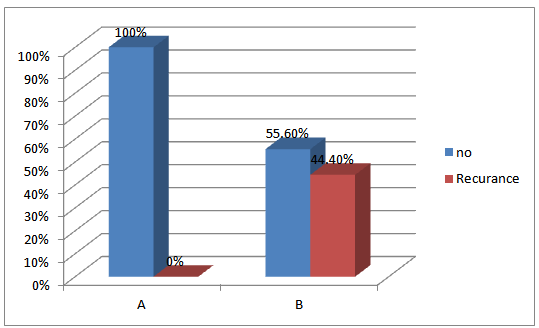 | Figure 1. Comparison between studies groups as regards Recurrence |
5. Discussion
- Pilonidal disease is a chronic disease of the natal cleft that causes both discomfort and embarrassment to sufferers. Recurrent follicular infection is the causative factor. It is often resistant to treatment so its treatment remains in question. Surgical treatment has a significant failure rate, and recurrence is common. The aim of the treatment of pilonidal sinus includes excising and healing with decrease recurrence rate[11]. The origin of pilonidal sinus has been a subject of interest for many years. It was thought to be of congenital origin, involving the remnant of the medullary canal and the infolding of the surface epithelium or a faulty fusion of the cutaneous covering in the early embryonic stage[2] but now it was believed that the majority of pilonidal disease cases are acquired and the result of a foreign body response to entrapped hair[12]. After the onset of puberty, sex hormones affect the pilosebaceous glands, and the hair follicles become distended with keratin. As a result, a folliculitis is created, which produces edema and follicular occlusion. The infected follicle extends and ruptures into the subcutaneous tissue, forming a pilonidal abscess. This results in a sinus tract that leads to a deep subcutaneous cavity. The laterally communicating sinus overlying the sacrum is created as the pilonidal abscess spontaneously drains into the skin surface3. Loose hair is sucked into the pilonidal sinus by friction and movement of the buttocks whenever the patient stands and sits. This trapped hair stimulates a foreign body reaction and infection[13]. Excess hair in and around the gluteal cleft increase the risk of the occurrence of the disease, and the frequency and severity of recurrences are directly related to the density of the hair present on the buttocks. Long-lasting or permanent hair removal in the gluteal area in pilonidal sinus disease would eliminate the hair decreasing the risk of recurrent disease[14]. Benedetto and Lewis[12] reported that the 800 nm diode laser may be an effective tool in the treatment of pilonidal sinus disease. Presence of large amounts of hair in the lower back is one of the risk factors that increase the chance of pilonidal sinus development. By eliminating the source of hair and hair fragments that course along the surface of the lower back and buttocks, interruption of the etiologic source for pilonidal sinus disease can be accomplished[14].There are recent reports that Laser hair removal in the area may be effective treatment for pilonidal cysts[15].Lavelle et al.,[16] said that laser treatment for pilonidal sinus, either as primary treatment or as an adjunct to surgery in refractive cases. It could also be useful in preventing the growth of hairs into wounds that have been left open and allowed to granulate.Oram et al.,[17] suggest that laser hair removal after surgical interventions in pilonidal sinus disease decreases the risk of recurrence over the long term.Our study meets with these studies in the effect of the Laser hair removal after pilonidal sinus excision decrease the rate of recurrence.
6. Conclusions
- Laser hair removal after surgical interventions in pilonidal sinus disease decreases the risk of recurrence. We recommend laser epilation to every patient with pilonidal sinus disease as an adjunct treatment after the surgical treatment.
References
| [1] | Nelson H, Cima RR. Anus. In: Townsend CM et al (eds) Sabiston Textbook of Surgery 2007; 18. Philadelphia, PA: Saunders Elsevier. |
| [2] | Hull TL, Wu J.Pilonidal disease. Surg Clin North Am2002; 82:1169–85. |
| [3] | McCallum IJD, King PM, Bruce J.Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ 2008;336:868–71. |
| [4] | Clothier PR, Haywood IR. The natural history of the post anal (pilonidal) sinus. Ann Royal Coll Surg Engl. 1984;66:201–3. |
| [5] | Downs AM, Palmer J. Laser hair removal for recurrent pilonidal sinus disease. J Cosmet Laser Ther. 2002;4:91. |
| [6] | Ghnnam WM, Hafez DM . Laser hair removal as adjunct to surgery for pilonidal sinus: our initial experience. Journal of Cutaneous Aesthetic Surgery 2011; 4, 192-195. |
| [7] | Boss WK Jr, Usal H, Thompson RC, Fiorillo MA.A comparison of the hair removal using the long-pulsed ruby Laser.Dermatol Surg. 1998; 24(8):837-42. |
| [8] | Williams R, Havoonjian H, Isagholian K, Menaker G, M. clinical study long-pulse and short-pulse Alexandrite laser hair removal systems.Ann Plast Surg. 1999. |
| [9] | Snedecor G M.and CochranW G. Statistical methods 1982 7th edition, lowa state Univ., Press, Ames. loww3a, USA., pp. 325-330 |
| [10] | Härdle W. and Simar L. Applied Multivariate Statistical Analysis 2007 2nd ed, Springer, 420pp. |
| [11] | Landa N, Aller O, Landa--Gundin N, Torrontegui J, Azpiazu Jl. Successful Treatment of Recurrent Pilonidal Sinus with Laser Epilation Dermatologic Surgery 2005 ;31(6):726-728 |
| [12] | Benedetto AV and Lewis AT. Pilonidal sinus disease treated by depilation using an 800 nm diode laser and review of the literature. Dermatol Surg. 2005 May;31(5):587-91. |
| [13] | Nivatvoungs S.Pilonidal disease.In:Gorden PH,Nivatvongs S,editors.Principles and Practice of surgery for the colon, Rectum,andAnus.NewYork:Informa Health care USA Inc; 2007.p,235-46. |
| [14] | Sadick NS, Yee-Levin J.Laser and light treatments for pilonidal cysts. Cutis2006;78:12. |
| [15] | Badawy EA, Kanawati MN. Effect of hair removal by Nd YAG laser on recurrence of pilonidal sinus. Journal of the European Academy of Dermatology and Venereology 2009 23: 8, 883-886. |
| [16] | Lavelle M, Jafri Z, Town G. Recurrent pilonidal sinus treated with epilation using a ruby laser. J Cosmet Laser Ther. 2002 Jun;4(2):45-7. |
| [17] | Oram Y, Kahraman F, Karncaoglu Y, Koyuncu E. Evaluation of 60 patients with pilonidal Sinus Treated with Laser Epliation after Surgery. Dermatologic Surgery 2010; 36, (1); 88-91. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML