-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2013; 2(4): 42-47
doi:10.5923/j.surgery.20130204.04
Clinical Study of Vertical Bone Formation around Dental Implants Using Titanium Re-Inforced Membrane
Hamid Reza Arab, Moeentaghavi, Neda Nasr, Majid Reza Mokhtari, Fateme Farazi, Vahab Shiezade
Dental Research Center, Mashhad university of Medical Sciences, Mashhad, 91889, Iran
Correspondence to: Majid Reza Mokhtari, Dental Research Center, Mashhad university of Medical Sciences, Mashhad, 91889, Iran.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
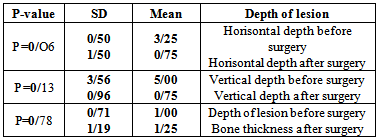
Objectives: This clinical study investigated the rate of bone formation in bone dehiscence and vertical bone defects around implants placed in one-stage approach with titanium reinforced membrane. Material and Methods:10 submerged implants (3I Osseotite) were placed in 7patients.From the 10 implants, 4 were installed in ridges with horizontal defects and the remaining 6 implants were installed in ridges with vertical bone defects in 3 patients. The exposed threads were covered with a xenograft bone material (Bio-Oss) and a titanium reinforced membrane. The membranes were removed after a minimum of six months. Whole-mouth GI (Gingival Index) was recorded at baseline and at re-entry surgery. A parallel PA was taken immediately after implantation and at re-entry surgery. Results: In horizontal defects, the baseline GI score was 0 for all patients. At re entry only one patient showed a GI=0.5. The mean defect width was 3.25± 0.05 mm and 0.75±1.50 at baseline and re entry respectively (P=0.06)and for the defect height were 5.00 ±3.56mm and 0.75±0.96 respectively (P=0.13). Mean depth dimension was 1±0.71mm and six months later, mean bone thickness was 1.25±1.19 mm(P=0.78). Conclusion: This clinical study showed that with the use of titanium reinforced membrane, clinical bone fill could be expected, if no membrane exposure and inflammation occurs.
Keywords: Titanium Reinforced Membrane, Endo Osseous Implant, Alveolar Ridge Augmentation
Cite this paper: Hamid Reza Arab, Moeentaghavi, Neda Nasr, Majid Reza Mokhtari, Fateme Farazi, Vahab Shiezade, Clinical Study of Vertical Bone Formation around Dental Implants Using Titanium Re-Inforced Membrane, International Journal of Surgical Research, Vol. 2 No. 4, 2013, pp. 42-47. doi: 10.5923/j.surgery.20130204.04.
Article Outline
1. Introduction
- After tooth extraction, alveolar bone atrophy may occur[1]. An insufficient bone volume and relevant vertical bone defect may render a difficulty for insertion of dental implants. GBR(Guided Bone Regeneration) can provide significant bone formation around placed implants in the alveolar bone. Many studies demonstrated significant bone formation in bone defects by means of barrier membrane in comparison with control group[2-4] ; and other studies showed implant success after ridge augmentation in atrophic jaw[5-10].GBR is accepted by researchers as a gold standard among various technique of ridge augmentation[11-14]. Sometimes this procedure is very time consuming; there are many cases with time limit which are not capable to accept such treatment. For these cases,simultaneous implant insertion and augmentation is proposed.The use of dental implants in partial or fully edentulous patients with inadequate alveolar bone has created a new demand for bone reconstruction prior or simultaneous implant treatment and also it is important when esthetic is considered by the patient. The most important and sensitive aspect of implant restoration is the implant placement in a predetermined prosthetic position to restore the normal position of the teeth and Simulate natural position of soft tissues. None position compliance of implant prosthesis, often lead to a restoration with function and esthetic problems and patient receivesless than acceptable results. Periodontal bone loss, tooth extraction and long-term usage of removable appliances result in boosted alveolar bone resorbtion that prevents implant prosthesis placement in proper position.Fortunately, numerous innovations in surgical techniques and advances in the biological understanding of bone regeneration techniques has led to improved methods of implant surgery and increased predictability in reconstruction of alveolar ridge defects[5,6].The aim of this study is to evaluate the clinical and radiographic success of implants that are located within bone by GBR and vertical and horizontal bone augmentation at the same time. Obviously if we have received an acceptable treatment success we may reduce treatment period significantly.
2. Materials and Methods
2.1. Inclusion Criteria
- 1- Patients had no contraindication for implant placement.2- Occlusion Condition was suitable for implant placement.3- Lack of periodontal disease in remaining dentition.4- Due to insufficient alveolar bone, it was not possible to insert implant without increasing the width and height of the alveolar ridge.5-Volume of alveolar ridge for simultaneous implant placement and ridge augmentation was sufficient.
2.2. Before Surgery
- Skin around the mouth was disinfected with “Povidone Iodine” solution and patient performed oral rinse with a solution of Chlorhexidine 0.2% for 2 minutes. Lidocaine combined with Adrenaline was used for local anesthesia. Anesthesia in the maxilla was performed by infiltration injection and in the mandible by inferior alveolar nerve block or mental block.
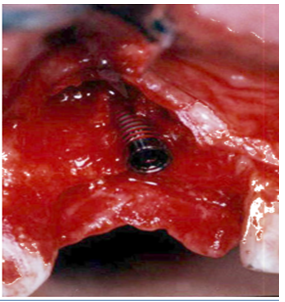
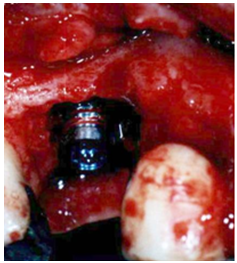
2.3. Surgical Protocol(Figures1-4)
- surgery was started with incision 2mm lingual from crest of alveolar ridge then continued in the gingival sulcus of adjacent teeth.(one tooth in anterior and the one in posterior) and finally ended with 2 releasing incisions 7-8 mm far from mesial and distal of implants. periosteum was incised in buccal in order to releas the flap for coronal movement.The two-stage implant type from 3I(3i osseotite)were placed with standard method and in ideal prosthetic location so that shoulder of implant was located 1-2 mm below cervical enamel junction of the adjacent teeth and implants had primary stability.
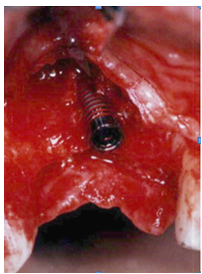 | Figure 1. Implant insertion |
 | Figure 2. Bone Material(bio-oss) around exposed threads |
 | Figure 3. Titanium reinforced membrane inserted. |
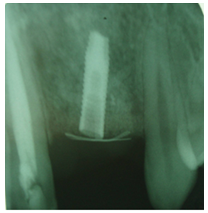 | Figure 4. Radiography |
2.4. Preparation of Client Area
- Cortical bone surrounding the implants was perforated by carbide bur to expose bone marrow and blood vessels and then the exposed screw of implants were covered by bio-oss.
2.5. Preparation and Placement of Membrane
- Titanium reinforced membrane was cut with scissors because of better adaptation with underlying bone and so on its edges was placed 4mm away from margin of bone defect. Membrane was fixed with apically extension of it and covering it with flap. Flap was sutured without pressure by “horizontal mattress suture” then releasing incisions were sutured with “interrupted suture”. A parallel radiograph from location of implant was taken for means of comparison with the one before re-entry surgery, to evaluate Osseo - integration.Gingival index was recorded in the whole mouth for each patient before surgery and again revaluated 6 month after surgery.
2.6. Postoperative Care
- Ice pack was instructed to use immediately after surgery up to 8 hours in the area.The patients were also told to clean all areas of their mouth with tooth brush and paste except the surgical areas ,and after brushing were asked to rinse their mouth with Chlorhexidin 0.2% for 2 minutes and do not consume anything for half an hour. Patients were treated with this antibiotic and anti-microbial regimen:7-10 days Amoxicillin 500mg and Metronidazole 250 mg both three times a day, and 100 mg doxycycline one time per day for 2 weeks; also Acetaminophen-Codeine 500 mg for every 6 hours was prescribed as for analgesic. One dosage of corticosteroid (Dexamethazone 8 mg) was used immediately after surgery to prevent swelling. Sutures were removed 14 days later; then patient was re-examined for plaque control and wound healing and a review was performed 3 months later.
2.7. Method of Measuring Bone Defect
- Vertical bone defect: measurement was performed with Williams calibrated probe from top of bone crest(palatal) down to upper part of implant shoulder in the center of it.
2.8. Horizontal Bone Defect
- First, the vertical height of defect was measured from most apically portion of defect to upper part of implant shoulder in center of it; second ,horizontal width was measured as mesio-distal in most labial portion of implant shoulder; third, horizontal width of defect was measured as bucco-lingual from most buccaly portion in center of implant shoulder to labial crest of bone.
2.9. Re-entry Surgery
- second surgery was done for each one of the bone defects at least 6 months after the first surgery, before surgery a parallel PA radiograph was obtained from the location of defect and then membranes were removed after local anesthesia by Lidocaine 0.2% and preparation of small flap with crestal incision. Measurements and evaluation of each lesion for vertical and horizontal defect was repeated by mentioned method. Radiograph was obtained from the area as a parallel PA. Film inserted in a XCP film holder.The distal end of tube should had been parallel with XCP loop. For assessing the mobility, two pieces of abeslangs were used and implant placed among them and then presence or absence of mobility was determined. For assessing the inflammation GI index was used,in this method 4 area of tooth or implant in facial mesial distal and lingual is examined for inflammation and receives a score 0 to 3; the score for each of these 4 areas is added together and calculated mean of it is added with the scores of the other teeth and implants(if any). For calculating average of full mouth GI the numbers are added together and are divided by total number of them.
3. Results
- 7patients (5 female, 2 male) from ages 22 to 45 participated in this study. Total of 10 implants were inserted using titanium reinforced membranes and Bio-oss bone graft in the areas of horizontal and vertical bone defect. 4 implants were inserted in horizontal and 6 in vertical defects. During the study period (6 months after implant insertion) none of the patients were excluded. In 2 patients (with5 implants) in vertical bone defect, early membrane exposure led to premature removal of membrane only one month after surgery. In one patient (with one implant)GI was 0.5(GI=0.5) six months after beginning the study.
3.1. Evaluation of Bone Construction in Horizontal Lesion
- 4 implants inserted in 4 patients with horizontal defects.GI was zero for all patients at the baseline. After 6 months, GI was 0.5only in one patient, because there was inflammation around the implant area. Horizontal loss of bone was measured in three dimensions (depth of the lesion, the horizontal and vertical dimensions) at the time of implant placement and 6 months after removal of membrane. The mean size of horizontal defects in horizontal dimension was 3.25 mm and 6 months after was 0.75 mm and mean size of vertical dimension was 5 mm and 6 months after the baseline was 0.75mm,the mean size of depth was 1mm before surgery and 6month after surgery was 1.25mm. Although the amount of bone in three dimensions, horizontal, vertical and depth of the lesion is clinically significant(Figure 5) But bone construction in none of horizontal and vertical dimensions and also depth of the lesion after 6 months, was significantly different from beginning of the study(table 1). Paired samples T-Test was used for statistical analysis. Power of this study using paired samples t-test for horizontal defects was 89% in horzontal,59% in vertical and 99% in depth of defects.
 | Figure 5. Evaluation of Bone Construction in Horizontal Lesion |
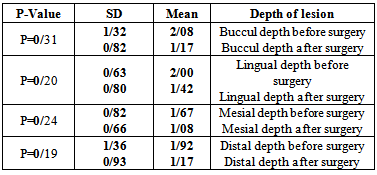
3.2. Evaluation of Bone Construction in Vertical Lesion
- 6 implants in 3 patients were inserted in vertical bone defects. GI was zero for all patients at the baseline and the end of study. In two patients, one with 2 and the other with 3 implants, early membrane exposure led to membrane removal one month after the beginning. Vertical bone defects in 4 dimensions (mesial, distal, lingual and facial) were measured for each implant at the time of implant placement and 6 months after surgery. The average size of defects in buccal dimension was 2.08 at the start of study and 1.17 6 months later, in lingual dimension was 2mm and 6 month later 1.42, in mesial dimension 1.67 and 6 months later 1.08 and in distal dimension was 1.92 and 6 months later 1.17(Table 2). No statistical significant difference in defect size was observed in vertical bone defects around implants (Figure 6).Paired samples T-Test was used for statistical analysis. In vertical defects, power of test in buccal and lingual dimension was 99% and 36 %, inmesial and distal 100% and 27% respectively.
 | Figure 6. Evaluation of Bone Construction in Vertical Lesion |
|
|
3.3. Radiographic Evaluation
- No radiolucency was observed around any of the implants, 6 months after implant insertion. Radiographic evaluation showed close contact of bone and implant in pre-existing bone and in area of bone construction.
3.4. Clinical Evaluation
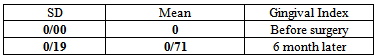
- After evaluating mobility with 2 abeslangs, no implant showed mobility and all of them were rigid after 6 months. GI index was used to evaluate inflammation, GI was zero at the start of the study for all of patients and 6 months later was 0.5 only in one patient. Thus the average of GI 6 months after surgery was 0.71(Table 3). Totally there was no significant difference in GI at the start of the study and 6 months after surgery(P=0.32)
|
4. Discussion
- Today autogenous onlay bone graft is the gold standard for comparing various ridge augmentation methods[5]. This technique involves removing autogenous bone block from sources inside or outside the mouth and screwing it on the bone surface with or without a membrane. Despite the good efficiency of this method there are many disadvantages mentioned such as rapid resorption of bone graft, having to use a large amount of bone block and thus complications like discomfort in the donor site, Impossibility of simultaneous implant insertion that results in prolonged treatment period and subsequently increasing patient costs[5,6]. GBR technique with protective membranes and graft biomaterials allow simultaneous implant insertion and ridge augmentation and therefore treatment time is reduced significantly. Bio-oss is axenograft and is made from bovine bone mineral[6]. This material has been extensively studied. In a study conducted by Hammerle et al this material compared with autogenous bone graft,that is known as the gold standard bone graft material,in this study Bio-oss bone conduction with GBR procedure was very similar to autogenous bone graft[15]. Simion et al also studied the combination of bio-oss and autogenous bone which were used in GBR and they achieved a successful result[16]. Furthermore, it has been shown that Bio-oss is absorbable in the body ; and absorption period is reported at least 6 months [17]. The use of Bio-oss may be better for the purpose rather than autogenous bone graft which requires surgery in another area of patient.Therefore, in this study Bio-oss was exerted as a bone conductig material.A2009 study, by Toygar et al ,evaluated titanium - reinforced membrane and non-resorbable membrane (e-PTFE) in GTR procedure, for the purpose of inducing periodontal ligament around the tooth lesions; the results showed that the titanium reinforced membrane was more effectively able to maintain space than e-PTFE and amount of regeneration of the lesions those were covered with titanium reinforced membranes were higher[18].Canullo et al in 2008 in a study demonstrated significant bone formation in vertical bone defects with titanium membranes[19]. Fugazzotto’s study in 2003, contained 59 sites of bone defects with titanium reinforced membrane comparing with several absorbable membranes; the results led to conclusion that the most ideal membrane to preserve space and bone formation is titanium reinforced membrane [20].This study evaluated the success of GBR techniques for vertical and horizontal bone formation after implantation by titanium reinforced membrane, In present study two patients, that one of them received two dental implants and the other received three implants in areas of vertical bone defects, were removed due to early membrane exposure (one month after the first surgery) before the end of the study, In these two patients no bone formation observed. In one patient implant regeneration wasn't successful although no exposure in membrane was present. In this case, GI 6 months after baseline was0.5 and BOP and inflammation observed in the surgical area. Inflammation in some areas of the mouth especially in bone lesion can be a major cause of treatment failure in this mentioned patient. Previous studies showed that if the membrane was exposed in the oral cavity early only a small amount or no bone is formed[6,21,22]. it depends on the membrane exposure timing after surgery. Wherever the exposure was sooner less amount of bone was formed. Previous studies showed that the GBR and simultaneous implant insertion had higher rate of soft tissue complications such as wound dehiscence and early membrane exposure in comparison with delayed implant insertion[3]. therefore although simultaneous implantation has the benefits of patient comfort, lower costs and shorter healing period; but also has soft tissue complications and higher risk of treatment failure. This study likewise previous studies emphasizes on the significance of membrane preservation during the period of bone formation in the site and also on the significance of soft tissue ability to keep surgery area safe and close during healing. in our study membrane exposure happened in the posterior regions of the mandible (two patients), and anterior region of mandible (1 patient).the reason of membrane exposure in the mandibular posterior region may be tension of buccinator muscle. Studies have shown that the major cause of wound dehiscence in surgical bone construction is tension on flap due to inadequate flap reflection and facial muscle tension[23]. Since there is lack of soft tissue overlying the membrane in the anterior mandible; this could possibly have led to flap tension and wound dehiscence. Chiapasco et al have investigated the vertical bone regeneration around implants with GBR in 11 cases, early membrane exposure occurred in 3 cases: the first patient at 3 weeks, second 8 weeks and the third one 10 weeks after suture removal. In all these cases bone construction and bone formation didn't happen[24]. In the present study, the incidence of premature membrane exposure was approximately equivalent to the mentioned study the complication which is the greatest problem for placing the implant in the vertical or supracrestal bone regeneration around implants. Evidence of connection between implant placement and supracrestal GBR is limited[25]. In a clinical study in 5 patients with vertical bone defects, simultaneously implant insertion led to 3mm to 7mm stripping of implant threads in the supracrestal region. In this region GBR procedure was used with BIO-OSS; results indicated 4mm bone gain after 9 months[26]. another study that investigated treatment of 7.2 mm average dehiscence in supracrestal region of implants revealed that bone formation in these areas ,which was determined by histometry, was 0.4 to 0.5 mm[27]. Thus, according to previous studies bone formation around vertical defects is less probable than horizontal defects. In our study all cases of membrane exposure occurred in vertical bone defects and the average of bone formation in the vertical lesions were lower than horizontal lesions. Based on the results of this study and previous studies using this method for regeneration of vertical bone defects is suggested if other methods of bone construction such as autogenous bone graft is not possible and the dimension of defect is small. The results of this study and previous studies suggest that bone regeneration around implants in the horizontal lesions can be successful if regeneration period is completely elapsed without difficulty (inflammation or premature membrane exposure not present). This was a pilot study conducted for the first time in our country (Iran). Due to the few number of samples in this study, because of different reasons including refusing of treatment and possibility of failure by patient, It is highly recommended that more studies be performed using a larger sample size, especially about vertical bone defects.
5. Conclusions
- This pilot study showed bone construction could be clinically significant using titanium re-inforced membranes, if early membrane exposure or inflammation and infection doesn't happen. Obviously if we have received an acceptable treatment success we may reduce treatment period significantly.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML