-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2013; 2(3): 27-30
doi:10.5923/j.surgery.20130203.05
Comparison of Conventional Pyodine Dressing with Honey Dressing for the Treatment of Wounds
Naeem-ullah1, Kamran Khan1, Habib-ullah2, Amer Hayat Khan3
1Orthopedic Department, District Headquarter (DHQ) & Teaching Hospital Bannu, Pakistan
2Plastic & Reconstruction unit, Hayatabad Medical Complex Peshawar, Pakistan
3Department of Clinical Pharmacy, School of Pharmaceutical Sciences Universiti Sains Malaysia, 11800 Penang, Malaysia
Correspondence to: Amer Hayat Khan, Department of Clinical Pharmacy, School of Pharmaceutical Sciences Universiti Sains Malaysia, 11800 Penang, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
objectives: To compare the conventional pyodine dressing with honey dressing, in terms of recovery time and debridement rate, in dirty wounds of the limbs. Material and Methods: Prospective study was performed in tertiary level and teaching hospital Bannu from August 2009 to July 2010. In patients were selected and assigned group A (Pyodine dressing) and group B (honey dressing) through simple convenience method. After proper clinical procedure, the surgical debridement group A was treated with conventional daily pyodine dressing and group B with daily honey application. Recovery time (in weeks) and debridement rate were noted for each patient. Patients consent form and ethical approval has been taken prior. Data were analyzed in the Statistical Package for Social Sciences (SPSS version 16 ®). Results: A total of 320 patients were registered, with mean age 26.56 ± 16.68 years and male to female ratio was 4.9:1. Recovery was found 1.612 times quicker in the Group B (Honey Dressing) as compared with the group A (conventional Pyodine dressing) (95% confidence interval[CI] 1.037–2.506, P = 0.034). Debridement rate was observed more in pyodine group as compared to honey dressing group. Healing was 1.751 times higher with honey dressing as compared with pyodine (95% confidence interval[CI] 1.120–2.736, P = 0.014). Conclusion: Honey dressing is an alternative dressing to the conventional Pyodine dressing with significantly improved recovery time in wounds. Further multicenter studies are suggested to prove its effectiveness with large population size.
Keywords: Honey, Iodine (Pyodine), Treatment outcomes, Wounds
Cite this paper: Naeem-ullah, Kamran Khan, Habib-ullah, Amer Hayat Khan, Comparison of Conventional Pyodine Dressing with Honey Dressing for the Treatment of Wounds, International Journal of Surgical Research, Vol. 2 No. 3, 2013, pp. 27-30. doi: 10.5923/j.surgery.20130203.05.
Article Outline
1. Introduction
- Many substances act as an antimicrobial agents were utilized to cover wounds, bleedings, reduce swelling, diminish pain, remove damaged tissue, treat infections, promote healing and care for thousands of years.[1] In 19th century the discovery of chemical preservatives and disinfectants, give better understanding of the nature of infection and inflammation, allowed increased control of wound infection.[2] In particular the use of carbolic acid by Joseph Lister in operating theatres from 1865 significantly reduced mortality rates associated with surgical procedures. When it was accepted that micro-organisms were the causative agents of infections, it became possible to consider more specific targeting. Wounds may be classified by several methods; their etiology, location, type of injury or presenting symptoms, wound depth and tissue loss or clinical appearance of the wound. Separate grading tools exist for Pressure Ulcers (EPUAP), Burns (Rule of Nines), Diabetic Foot Ulcers (Wagner / San Antonio) and General Wounds.[3]General wounds are classified as being[3]:● Superficial (loss of epidermis only) ● Partial thickness (involve the epidermis and dermis) ● Full thickness (involve the dermis, subcutaneous fat and sometimes bone) The most common method for classification of a wound is identification of the predominant tissue types present at the wound bed; i.e. black – necrotic and the respective amount of each expressed as a percentage. This classification method is very visual, supports good assessment and planning and assists with continuous reassessment.[4] Honey is an ancient remedy, which has been re-discovered for the treatment of wounds.[5,6] Many therapeutic properties have been attributed to honey including antibacterial activity and the ability to promote healing.[7] Evidence of antibacterial activity is extensive, with more than 70 microbial species reported to be susceptible.[8] Manuka honey shows bactericidal activity against strains of antibiotic resistant bacteria isolated from infected wounds. [9,10] Iodine (pyodine) is an element that was discovered in 1811. It is a dark violet solid that dissolves in alcohol and potassium iodide. Its first reported use in treating wounds was by Davies in 1839.[11] Early products caused pain, irritation and skin discolouration, but the development of iodophores (povidone iodine and cadexomer iodine) since 1949 yielded safer, less painful formulations. It has a broad spectrum of activity against bacteria, mycobacteria, fungi, protozoa and viruses. Iodine is mainly used in one of two formats: (a) as povidone-iodine (polyvinylpyrrolidone-iodine complex), an iodophor (a compound of iodine linked to a non-ionic surfactant), which is produced as impregnated tulle; and (b) as cadexomer iodine (a three dimensional starch lattice containing 0.9% iodine). Cadexomer iodine has good absorptive properties: 1 g of cadexomer iodine can absorb up to 7 ml of fluid. As fluid is absorbed, iodine is slowly released, reducing the bacterial load and also debriding the wound of debris. This mode of action facilitates the delivery of iodine over a prolonged period of time—thus, in theory, maintaining a constant level of iodine in the wound bed.[12] Clinically, pyodine has application not only in the management of wounds, but as a skin antiseptic prior to surgery, and in the disinfection of inert surfaces.[13] Whereas its efficacy as a skin disinfectant is undisputed, numerous publications describe the use of iodine in cleansing wounds, and as a topical agent to prevent or treat localized wound infections but controversy surround its safety and efficacy.[14] A report that absorption of pyodine gave rise to severe metabolic acidosis, which complicated the management of two burns patients who died of renal failure.[15] Thyroid disease owing to possible systemic uptake of iodine. For this reason, thyroid function should be monitored in patients who are treated with iodine dressings.[12] Lack of research attention to provide evidence that honey is effective or inferior to pyodine in wound dressing. This study is aimed to determine the effectiveness of honey dressing in wounds with compare to pyodine.
2. material and Methods
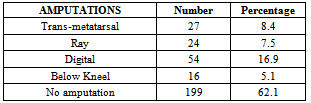
- This Randomized control trial was performed in orthopedics unit of tertiary level of teaching hospital[District Headquarter (DHQ) and teaching hospital] Bannu, Pakistan from August 2009 to July 2010. District Bannu is centre in south part of Khyber Pakhtoon-Khaw (North West Frontier) province of Pakistan with 942230 population and male to female ratio 1:1.08.[16]Patients were admitted from out-patients, emergency departments and referral from Medical units and assigned to group A (pyodine dressing) or group B (honey dressing) through simple convenience method. Patients’ detailed history, general clinical examination, local examination was documented. After proper surgical debridement group A was treated with conventional daily pyodine dressing and group B with daily honey application. Recover time (1-3, 4-6 weeks), outcome (Healed, amputated) were noted for each patient. Amputation type (Ray, trans-metatarsal, digital, below knee, above knee) were also documented in those who undergone amputation. All diabetic (both type I and II) were excluded from the study.Patients consent form and ethical approval has been taken prior from review board. Data were organized and analyzed with the help of Statistical Package for Social Sciences (SPSS 16).
3. Results
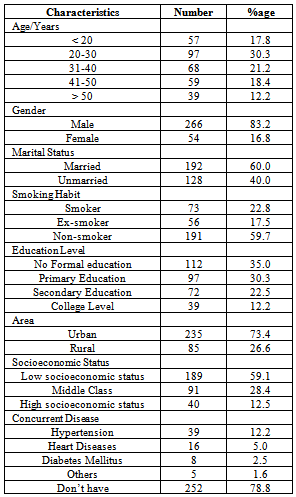
- Total of 320 patients were included in the study with age ranging from 8 to 70 years with mean age of 26.56 ± 16.68 years consisting of 266 (83.2%) male and 54 (16.8%) female patients with male to female ratio of 4.9:1. Out of total (N=320), 160 patients were included in group A and same in group B. Among total numbers of patients, 73(22.8%) were smokers and 191 (59.7%) were non-smokers. Majority of patients were either uneducated 112 (35.0%) or their level of education is primary level 97 (30.3%), whereas more than, one third cases were from urban area 235 (73.4%) with low socioeconomic status 59.1% and some concurrent disease were also observed 68 (21.5%), as illustrated in table 1.
|
|
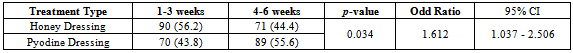
3.1. Recovery Time
- In group A (Conventional Pyodine Dressing), 71 (43.9%) patients healed in 1- 3 weeks and 89 (55.6%) in 4-6 weeks while in group B (Honey Dressing), 89 (56.1%) patients healed in 1- 3 weeks, and 71 (44.4%) in 4-6 weeks. Recovery was found 1.612 times quicker in the Group B (Honey Dressing) as compared with the group A (conventional Pyodine dressing) (95% confidence interval[CI] 1.037– 2.506, P = 0.034). (Table 3)
|
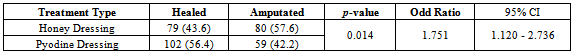
3.2. Outcome
- Table 4 revealed that, 102 (56.4%) patients healed with honey dressing, while 79 (43.6%) were with pyodine. Healing was 1.751 times higher with honey dressing as compared with pyodine (95% confidence interval[CI] 1.120 – 2.736, P = 0.014).
4. Discussion
- Utilizations of honey as a dressing can be traced back to Roman as well as Muslim civilization or perhaps earlier than them. Due to its hyper osmotic sugar contents, honey is sterile and thus inhibits bacterial growth. Honey has a thermo labile inhibin which due to its low pH and hygroscopic qualities acts as an antimicrobial agent. After the discovery of inhibin, honey was widely used for chronic wounds, burns, chronic leg ulcers, decubitus ulcers and radiation necrosis. Honey has catalase enzyme which helps in the healing process and promotes epithelialization.[5, 6, 17] In current study the age of the study population ranged from 8-70 years with mean age of 26.56 ± 16.68 years which is younger than some reported age in literature.[18] Male to female ratio was 1.62:1 in this study which is comparable with other published studies, may be due to male dominant society.[18, 19] Lazarus et al (1994) concluded so many factors which affect directly on wounds healing like hypertension, venous disease and diabetes mellitus etc, which strengthen the findings of current study.[18] Majority of population are staying in rural area of China and India, where the patients using traditional medicines and avoid to visit hospitals and ignoring their wounds which is affect the health and same picture are reflecting here, while low education levels also reported reasons for injury and or wounds[20, 21] Though findings of the study shows that honey is 1.012 times better treatment recovery time and treatment outcomes is also improved than Iodine (pyodine) but in-fact it is extremely small value, which needs further investigation with bigger sample size. On the basis of medical evidence and focus on clinical aspects, honey has been recently reviewed in literature for treating wounds.[7, 22] Various studies have shown the effectiveness of honey for the treatment of wound especially in diabetic foot ulcers, abrasions, abscesses, amputations.[23, 24] In the current study, honey group shown quicker recovery time and reduced rates of amputations as compared to conventional pyodine dressing. Application of ordinary honey on the wounds on daily bases shows good results, even no need to continue antibiotic or saline dressing. The cost of this therapy was merely that of the dressings. Dressing changes were painless and the serum glucose remained in good control. A large amount of evidence in the form of case studies also favors the effectiveness of honey in wound care.[25] In contrary Majtan reported that Manuka honey impairs wound healing in diabetic patients.[26] Seventeen randomized controlled trials involving a total of 1965 participants have shown positive results on honey in wound care, whereas 16 trials on experimental animals have also shown the effectiveness of honey in wounds healing, which further strengthen our findings.[27]
5. Conclusions
- Honey dressing is an alternative dressing to the conventional Pyodine dressing with significantly improved recovery time in wounds, but further large multicenter studies are suggested to establish its usefulness in the treatment of wounds. At initial stage of wounds, easy control can be possible but for this communication and appropriate education for patients should be conduct.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML