-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2013; 2(3): 21-23
doi:10.5923/j.surgery.20130203.03
Oxidized Cellulose (Surgicel) As a Surgical Hemostat in Liver Injury: A Case Report and Litrature Review
Azhar Amir Hamzah1, Azreen Syazril Adnan2, Mohammad Nor Gohar Rahman1, Amer Hayat Khan3
1Urology Unit, Department of Surgery, Hospital University of Malaysia, Kubang Kerian, Kelantan, Malaysia
2Nephrology Unit, Department of Internal Medicine, Hospital University of Malaysia, Kubang Kerian, Kelantan, Malaysia
3Department of Clinical Pharmacy, School of Pharmaceutical Sciences, Universiti Sains Malaysia, 11800 Penang, Malaysia
Correspondence to: Azhar Amir Hamzah, Urology Unit, Department of Surgery, Hospital University of Malaysia, Kubang Kerian, Kelantan, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Liver is a common solid organ injured in a blunt abdominal injury; frequently inflicted by motor vehicle accidents (MVA). Whilst most low grade liver injury is managed conservatively, operative approach remains an option in many cases, notably liver packing. A 15 year-old Malay, male who sustained a blunt abdominal injury and fractured left clavicle with no loss of consciousness was referred to a tertiary level hospital, six hours following an MVA. On arrival, patient appeared restless; blood pressure was 90/50 mmHg, distended abdomen with board-like rigidity in both upper quadrants and was managed for hypovolaemic shock. His haemoglobin was 4g/dl. Subsequent imaging revealed a fluid collection in the Morrison’s pouch on ultrasound while computed tomography (CT) scan revealed grade IV splenic injury and 5 & 6cm lacerations in segment II & VII of the liver respectively. The operative findings were shattered spleen (grade V injury), a concealed liver laceration and a massive clot at the splenic bed. Splenectomy was done along with oxidized cellulose (surgicel) packing of the liver. The estimated blood loss was 4 litters. The post-operative recovery over six weeks was uneventful and was vaccinated against encapsulated organisms prior to discharge. Grade IV liver injury using oxidized cellulose (Surgicel) proven to good response.
Keywords: Liver Injury, Hemostasis, Oxidized Cellulose
Cite this paper: Azhar Amir Hamzah, Azreen Syazril Adnan, Mohammad Nor Gohar Rahman, Amer Hayat Khan, Oxidized Cellulose (Surgicel) As a Surgical Hemostat in Liver Injury: A Case Report and Litrature Review, International Journal of Surgical Research, Vol. 2 No. 3, 2013, pp. 21-23. doi: 10.5923/j.surgery.20130203.03.
1. Introduction
- The use of oxidized cellulose in various surgical fields as a useful tool for hemostasis is well recognized.[1] This ranges from cardiothoracic, neurosurgery, orthopaedics, obstetrics and gynaecology to paediatric surgery in securing hemostasis for cases such as uterine perforation, paediatric liver and splenic injury, as well as thoracotomy. Oxidized cellulose use has been extended even in bones, but this requires removal to avoid nonunion. Moreover, there has been reports linking its use with complications such as nerves entrapment or herniation into the intervertebral space, particularly with thoracotomy.[2-4] Oxidized cellulose (“Surgicel”; Johnson & Johnson) is a synthetic hemostat produced from wood pulp.[5] It acts by stimulating the innate coagulation mechanism, and in the process expanding and producing an acidic medium that converts hemoglobin to acid hematin, giving rise to black color, which responsible for antimicrobial affect.[3,5, 6]Literature shows that oxidized cellulose exert its effect through the intrinsic coagulation pathway.[5,7] Although an effective hemostat and exact mechanism of action remains elusive after over half a century of discovery.[6]In addition, oxidized cellulose fulfills the first principle of hemostasis i.e pressure. As it absorbs fluid, it swells thereby exerting a pressure effect on the surrounding tissue eventually effecting hemostasis.[3,5,6,8] However, a complete absorption is possible within 2-4weeks.[5,6] Nevertheless, several reports previously highlighted the practical ease of administration and use of oxidized cellulose compared with other topical hemostatic agents.[5,9] Injured liver in a blunt abdominal injury, commonly inflicted by motor vehicle accidents (MVA). Low grade liver injury is managed conservatively, while operative approach remains an option in many cases, current patient is one of such scenario.
2. Case Report
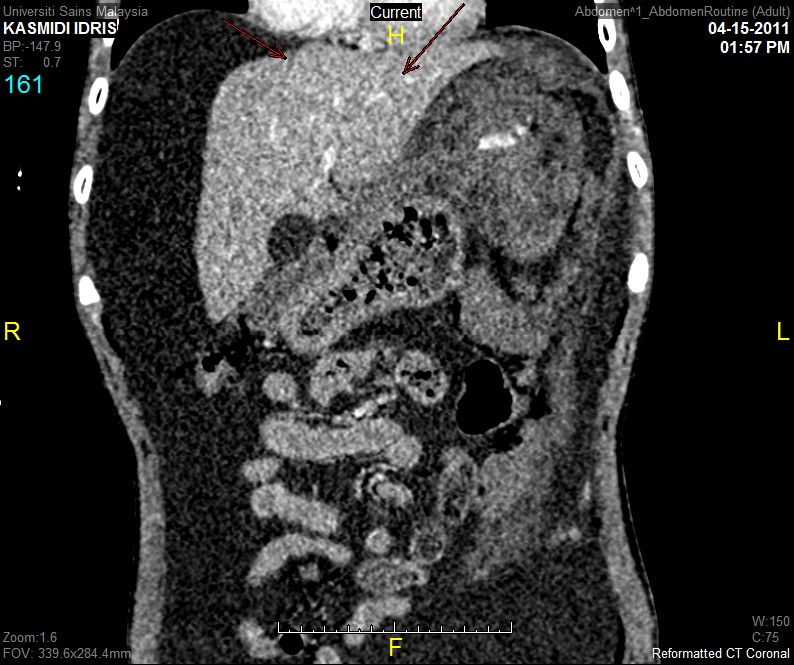
- A 15 year-old Malay boy who sustained a blunt abdominal injury and fractured left clavicle with no loss of consciousness was referred to a tertiary level hospital, six hours following an motor vehicle accident (MVA). On arrival, patient appeared restless; blood pressure was 90/50 mmHg, distended abdomen with board-like rigidity in both upper quadrants and was managed for hypovolaemic shock. His haemoglobin was 4g/dl.Subsequent imaging revealed a fluid collection in the Morrison’s pouch on ultrasound while computed tomography (CT) scan revealed grade IV splenic injury and 5 & 6cm lacerations in segment II & VII of the liver respectively (figure 1 and 2).The key operative findings were shattered spleen (grade V injury), a concealed liver laceration and a massive clot at the splenic bed. Splenectomy was done along with oxidized cellulose (surgicel) packing of the liver. The estimated blood loss was 4 litters. The post-operative recovery over six weeks was uneventful and was vaccinated against encapsulated organisms prior to discharge.
 | Figure 1. Segment II |
 | Figure 2. Segment VII |
3. Discussion
- The application of oxidized cellulose in various surgery is an effective tool, whereas it is recognised that liver injury imposes a surgical challenge in practice.[1] Although conservative management is favored in grade I-III injury especially in the pediatric age group, while some still require operative management.[10,11] Conservative management aims to stabilize the patient and frequently involves transfusing blood and blood product when indicated.[1,2] Present patient needs were beyond conservative management because he had a grade V splenic injury which was underestimated by CT scan and presented with a significant haemodynamic compromise.Although minimal invasive methods had been advocated, including the use of angiographic embolization and laparoscopic application of fibrin glue, open surgical approach for higher grades of injury (IV-VI) offers favorable outcome in large number of patients.[8,10-12] In the latter scenario, perihepatic packing either with gauze alone or hemostat impregnated gauze remains the preferred choice in the management of liver injury.[10,13]Unlike an abundance of literature on liver packing using gauze and its hemostat coated derivatives scarce clinical data exist to advocate oxidized cellulose for the same purpose. Literature shows that perihepatic gauze packing had been reported to improve survival but disadvantaged by re - exploration for safe removal of the hemostat.[1, 13] Some controversies existing there and studies shows that oxidized cellulose is thought to deliver a desired hemostatic effects from local effect and co-activation of the intrinsic pathway of the clotting mechanism and platelets.[7,8] Evidently, in current patient, the liver bed drain remained empty from day first to day-5 post operatively when it was removed. The in-situ drain was kept in anticipation of probable clot lysis which tends to occur within the first 72 hours.Some latest research revealed new methods for liver packing. Such methods include a nanotechnology-based synthesis of a biodegradable material that gets converted into amino acids once internalized.[15] Although of unclear mode of action, Nano Hemostat Solution (NHS) for example, delivers a rapid onset of effect (within 15 seconds) that certainly hold breakthrough promises for wider use in surgical practice.[7] Nonetheless, NHS lacks practical value in hemostat packing of liver injury owing to its liquid nature as well as restrictions to apply to the injured liver segments that may be concealed underneath the diaphragm.
4. Conclusions
- Routine follow-up with radiological findings were effective diagnostic/confirmative tools. Oxidized cellulose in current patient is relatively simple and effective technique. Still effective liver packing for grade IV liver injury using oxidized cellulose (Surgicel) and offer insightful overview of its use as a surgical hemostat despite its current under utility in the management of such injuries.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML