-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2013; 2(3): 13-15
doi:10.5923/j.surgery.20130203.01
Prospective Study of Open inguinal Hernioplasty and Short-Term Outcomes
Amer Hayat Khan1, Andee Dzulkarnaen Zakaria2, Syed Hassan2, Siti Rahmah Hashim Isa Merican2, Syed Azhar Syed Sulaiman1
1Department of Clinical Pharmacy, School of Pharmaceutical Sciences Universiti Sains Malaysia, 11800 Penang, Malaysia
2Department of Surgery, School of Medical Sciences, Universiti Sains Malaysia, Health Campus, Kelantan, Malaysia
Correspondence to: Amer Hayat Khan, Department of Clinical Pharmacy, School of Pharmaceutical Sciences Universiti Sains Malaysia, 11800 Penang, Malaysia.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Inguinal hernia still remains a significant clinical issue and surgeon has to manage. Though, improved surgical techniques and a better understanding of the anatomy and physiology of the inguinal canal have significantly improved outcomes for many patients. This study was designed to evaluate the outcomes among hernia patient. Between March 2012 and May 2012, a prospective study of 11 consecutive patients operated for groin hernia using an open preperitoneal tension free mesh technique by a single surgeon was performed in surgical unit, Hospital Universiti Sains Malaysia (HUSM). The outcome variables being analyzed included time to return to normal activity, pain level, complications and recurrence rate. Mean age of the patients was 58.34±14.62 years. Majority of patients (5) had right sided inguinal hernia. Wound infection occurred in 1 patient. No recurrence was observed. Moreover, mild pain were found in 2 patients. A good short-term outcome was found in this study. Lichtenstein’s technique of inguinal mesh repair is a safe and effective procedure even in comrobid condition.
Keywords: Open inguinal Hernioplasty, Short Term Outcomes, Co-morbid Condition
Cite this paper: Amer Hayat Khan, Andee Dzulkarnaen Zakaria, Syed Hassan, Siti Rahmah Hashim Isa Merican, Syed Azhar Syed Sulaiman, Prospective Study of Open inguinal Hernioplasty and Short-Term Outcomes, International Journal of Surgical Research, Vol. 2 No. 3, 2013, pp. 13-15. doi: 10.5923/j.surgery.20130203.01.
1. Introduction
- Inguinal hernia regardless of type is one of the most common clinical problem that a surgeon has to manage, despite advances in surgical technique[1]. Improved surgical techniques and a better understanding of the anatomy and physiology of the inguinal canal have significantly improved outcomes for many patients. Recurrence rate of 16-18% following a variety of repair techniques and re-recurrence rates of over 30% have been reported[2]. Application of prosthetic mesh has improved the recurrence rate, worldwide[3]. However, in the re-operative challenging condition the anterior approach still has the disadvantages with the risk of damages to the testicular blood supply and sensory nerves[4].Traditional suture repair of inguinal hernia is fast giving way to routine tension-free mesh repair. This operation is called a ‘hernioplasty’. In many countries, mesh repair is now more common than suture repair[5]. Lichtenstein presented his open mesh repair technique for inguinal hernia in 1986. The Lichtenstein technique has since become the most commonly used[6] (with various modifications) on account of its ease of operation and because it provides a tension free repair with good long-term results[7].Tension-free mesh repair is nevertheless associated with complications such as foreign body reaction, infection, pain, fistula formation, migration, shrinkage, and recurrence[5]. Other complications include skin anaesthesia, bruising and haematoma formation, seroma formation, orchitis and testicular atrophy. Co-morbid condition may affect surgical procedure and or may be delaying.The aim of the study was to evaluate the outcome of early experience of open pre-peritoneal mesh hernioplasty with or without co morbid condition in 11 patients.
2. Methodology
- Between March 2012 and May 2012, a prospective study of 11 consecutive patients operated for groin hernia using an open pre-peritoneal mesh technique by a single surgeon was performed in surgical unit, Hospital Universiti Sains Malaysia (HUSM). Following admission a detailed history and examination was performed. All patients were investigated for haemoglobin %, blood urea and glucose, chest x-ray. Electrocardiogram was advised for all patients over the age of 45 years. In patients whom incidental findings of derangements of investigations were found, opinion from relative specialties was requested to assess fitness for anaesthesia. Final assessment was confirmed by the attending anaesthetist. A detailed explanation about the participation in the study was given to the patient and a written consent was obtained.The repair technique was modified from Nyhus[8] and Wantz[9], using a transverse incision just below the level of the iliac crest. Polypropylene mesh with size varies from 10 × 12 to 10 × 15 cm was shaped to fit properly in each patient. The mesh was attached inferiorly at the pubic symphystic and the superior pubic rimus just medial to the femoral vein with non-absorbable 2/0 polypropylene sutures. The upper portion of the mesh which extended above the incision was picked up with 2 or 3 bites. No vacuum drain was used in these patients. Patients were discharged few days after operation and were followed for at least 4 weeks in the out-patient department.
3. Results
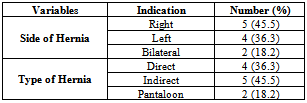
- There were no major difficulties during the operation. Patients were hospitalized for 1-2 days following the procedure. Among 11patients, 9 were males and 2 were females, and mean age of the patients was 58.34+ 14.62 years. Table 1 revealed that, 5 (45.5%) patients had right sided inguinal hernia while 4 patients (36.3%) had a left sided hernia and two patients (18.2%) had bilateral hernia. Those with bilateral hernia were operated for only the side with more symptoms and were given a later date to follow for surgery on the contra lateral side. Five patients were diagnosed per operatively with indirect hernia, whereas 4 had a direct hernia and 2 (18.2%) patients had a pantaloon hernia.
|
4. Discussion
- The mean age in current study is 58.34+ 14.62 years (S.D±14.62) which is comparable to studies in the west and Asia but strongly contradicts African studies[10]. The side of inguinal hernia was dominantly found per operatively on the right side in patients (45.5%). Whereas the type of hernia was predominantly of the indirect type; 5 (45.5%) patients comparable to the study conducted in Nigeria[11].Recurrence after mesh hernia repair is related to technical factors such as inadequate dissection, insufficient prosthesis size and fixation, and surgeon skill[13]. Prolene mesh was better option, whereas the method of mesh attachment was similar to that used by Rives et al.[14].The pre-peritoneal approach for recurrent inguinal hernia which avoids reoperation through distorted anatomy and scar tissue markedly reduces the risk of damage to the testicular vessels and permits inspection of all potential groin hernia sites. Through an open incision, the dissection is rapid, while structures are easily to access and widely visible. Its benefits have long been proclaimed[15]. The operative procedure was done with ease in 3 patients in our series. Although access is easy and good via this route, the results of recurrent hernia repair remained poor unless prosthetic mesh was added to the repair[8]. Stoppa and colleagues[16] placed a large sheet of mesh, via a midline incision, in the pre-peritoneal plane without closing the defect or fixing the mesh. Wantz described a unilateral version of the procedure through a high transverse incision[9]. Even with complex or multi-recurrent hernias, this method gave impressive results.Despite these clear benefits and excellent results, open pre-peritoneal mesh repair has not been widely adopted, in part because of the unfamiliarity with this approach. In a recent survey of groin hernia repair, 85% of repairs for recurrent inguinal hernia were open anterior procedures and only 15% were pre-peritoneal approaches (9% laparoscopic and 6% open re-peritoneal)[17].The laparoscopic surgery provides a means of entering the pre-peritoneal space without an open incision. The technique was adopted with widespread enthusiasm, followed by alarming reports of vessel and viscous injury, nerve damage and high recurrence rates when inadequate pieces of mesh were used by inexperienced surgeons[18]. Furthermore the laparoscopic approach cannot be used in patients with incarcerated, large inguinoscrotal hernias or in patients unfit for general anaesthesia[19].In this study, postoperative pain was minimal, only oral analgesia was required and rapid mobility was permitted so that patients could be discharged within 24 to 48 hours after operation. Three comparative studies found more postoperative discomfort and a longer recovery time with the open operation[19], although all used a lower midline incision. The present experience accords with that of Rignault[20], who concluded that a pfannenstiel incision causes the least discomfort as well as lowest risk of incision hernia. In conclusion, the open pre-peritoneal mesh repair for inguinal hernia is effective surgical technique to achieving a low recurrence rate in current study. It is a simple procedure and easier to learn as well as safer than laparoscopic repair, and should be the choice for all groin hernias.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML