-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2012; 1(2): 7-10
doi: 10.5923/j.surgery.20120102.01
Bridge-Plating Technique for Tibial Shaft Fractures: Is Rotation Deformity a Rare Complication
Pedro José Labronici 1, Robinson Esteves Santos Pires 2, Junji Miller Fukuyama 3, José Sérgio Franco 4
1Donato D’Ângelo Orthopaedics and Trauma Department, Santa Teresa Hospital, Petrópolis, RJ, Brazil
2Department of Orthopaedics and Traumatology, Federal University of Minas Gerais and Felicio Rocho Hospital, Belo Horizonte (MG), Brazil
3Department of Orthopaedics and Traumatology, Vila Penteado Hospital, Sao Paulo (SP), Brazil
4Department of Orthopaedics and Traumatology, Federal University of Rio de Janeiro, Rio de Janeiro (RJ), Brazil
Correspondence to: Robinson Esteves Santos Pires , Department of Orthopaedics and Traumatology, Federal University of Minas Gerais and Felicio Rocho Hospital, Belo Horizonte (MG), Brazil.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
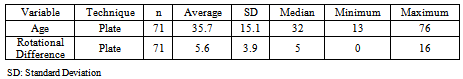
Objective: Assess postoperative rotational deviation in patients treated with bridge-plating technique for tibial shaft fractures. Methods: Between 2002 and 2005, 113 patients with tibial shaft fractures were surgically treated in a general trauma center. Seventy-one underwent the bridge-plating technique. CT scan measured tibial rotation. All fractures were classified using AO Classification System and divided into sub-groups according to anatomic location (proximal, medial, distal, and segmented), exposure (closed and open, sub-classified using Gustilo Method), and internal or external rotation percentage. Results: No significant difference in tibial rotation was found in fracture location and type (A or B). External rotation was two times more frequent than internal rotation. Rotational deviation following the bridge-plating technique occurred mainly in Type C and open (high energy) fractures. Conclusion: Regardless of tibia fracture location, rotational deviations are related to trauma energy, and thus more difficult to control using the bridge-plating technique.
Keywords: Tibial fracture, Bridge-plating, Fracture
Article Outline
1. Introduction
- The tibia is the long bone most often affected by fractures1,2,3. Each treatment type involves inherent complications associated with the specific stabilization method4-10. According to stability concepts, unstable displaced tibial shaft fractures may be treated by the principle of relative stability11-13. Thus, bridge plating is an available technique and presents good functional results and a low complication rate compared to plaster immobilization, open reduction with internal fixation, and external fixator4,14-21. Regarding postoperative complications, rotational deviation is poorly valued, as it can cause cosmetic problems and may lead to functional complications and osteoarthritis22-28.This study aimed to use CT scan to prospectively assess the rotational deviation incidence in patients who underwent bridge-plating technique for tibial shaft fracture treatment.
2. Patients and Methods
- Between 2002 and 2005, 113 patients with unilateral tibial shaft fractures underwent surgical treatment in a general trauma center. Seventy-one were treated with bridge-platingtechnique. Inclusion criteria were adult patients with closed or open tibial shaft fractures for which bridge plating was indicated according to surgeon preference, and patients previously treated with an external fixator for local damage control. Excluded were patients having tibial shaft refracture, bilateral fractures, ipsilateral femur fracture, and those suffering from conditions such as neurological or congenital disorders, Gustilo Type 3C, and patients who refused the CT scan.Radiological assessment involved CT imaging of both tibiae to compare rotation degree. In the technique used, developed by Jakob et al1, the patient was maintained in a supine position with legs fixated and patella parallel to the table on supports to prevent movement. Tomographic slices were 2 mm, taken in the proximal region above the tibiofibular joint and in the proximal region of the tibiotarsal joint (Figures 1 and 2). The proximal line of reference was tangential to the dorsal edge of the tibia and proximal to the head of the fibula29. The distal reference line was perpendicular to the tibiofibular joint in the tibial pilon region28. Tibiofibular rotation was defined as the angle between the two axes and compared with the unaffected limb. Internal rotation deformities were classified with a negative score and external rotation deformities with a positive one. Rotational deformity was defined as a 10º difference in relation to the unaffected limb7,30,31. The authors received informed consent to publish the case reports, and the accompanying images were obtained from all the patients concerned. The main institution in the study obtained ethical approval in accordance with the 1964 Declaration of Helsinki ethical standards.
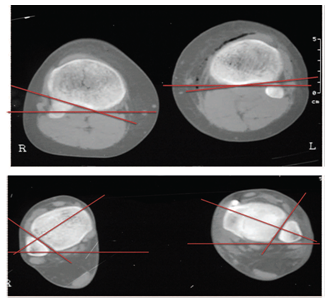 | Figures 1, 2. CT slices of proximal and distal tibial regions and their respective measurements |
2.1. Statistical Method
- Statistical analysis was performed using Mann-Whitney to check degree of tibial rotation differences for the different fracture patterns treated by bridge-plating technique. Kruskal-Wallis variance analysis was used to compare three groups (Types A, B, and C). The proportion of internal and external rotation was assessed using chi-squared test (χ2). Non-parametric tests were used when the rotational difference did not have a normal (Gaussian) distribution due to data dispersion and lack of distribution symmetry. The criterion used to determine significance was 5%.
3. Results
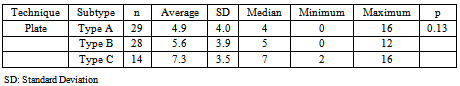
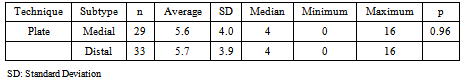
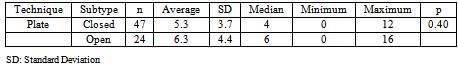
- Of the 71 bridge-plating cases, 57 were male and 14 female. The ages ranged from 13 to 76, with the average being 35.7 years old. Patient fractures were located as follows: 4 in proximal third, 29 in medial third, 33 in distal third, and 5 segmented fractures. According to AO fracture classification26, 29 patients had a Type A fracture, 28 Type B, and 14 Type C. Open fractures were classified usingGustilo-Anderson Classification27: five patients had Type 1, 11 Type II, and 8 Type III. In 47 patients, the fractures were defined as closed.Internal rotation deviation was 28.17%, external 59.15%, and null 12.68%.A 5.1º rotational difference existed, varying between 0º and 16º. Using this technique, 7 patients presented rotational deviations over 10º, ranging from 12º to 16º, with an average of 14º.Tables 1, 2, and 3 show if there is any significant rotation difference between the fracture subgroups when patients were treated with the bridge-plating technique.
|
|
|
|
4. Discussion
- Irrespective of treatment type, clinical manifestations of rotational deviations following tibia shaft fracture treatment are so discreet they often go unnoticed. Various methods cited in the literature measure tibial rotation, although most are unreproducible25, 32-34.In most studies, rotational deviation was defined as a rotational difference greater than 10º, varying between 5º and 15º compared to the unaffected limb7,30,31. In the literature, the incidence of this deformity when related to intramedullary nailing ranges from 0% to 6%. Statistical parameters for bridge plating are undefined15,35-40. In all cases however, the assessment method used was clinical or unspecified. To accurately quantify the incidence of tibial reduction following the bridge-plating technique, CT scan was used in a prospective series of patients.This method of assessing tibial rotation was first recorded by Jakob et al1, although Jend et al28 proposed a similar method. Both studies confirmed the precision of the measurements and demonstrated cumulative reproducibility after the measuring the angles, with 95% of the sample located between 3º and 7º1,28.Studies analyzing rotational deviation after intramedullary nailing suggest the complication is rare. When observed clinically however, the literature reports an incidence between 0% and 15%7,30,31. In Puloski et al39, CT scan demonstrated rotation in tibial shaft fractures treated with intramedullary nailing, which suggested 20% of patients developed tibial rotation greater than 10º.Although the aim of this study was to tomographically assess tibial shaft fractures, the authors realize clinical alterations such as functional limitations, osteoarthritis, and walking alterations may develop. Krettek et al40 and Puloski et al39 demonstrated that the injury pattern may influence results. High energy and comminuted fractures, large bone fragment deviations, and fractures of the distal third seem particularly prone to rotational deformities. As shown in the literature, high energy and/or complex fractures were the most susceptible to rotational deviation. The authors found no more significant rotation degree for distal tibial fractures as demonstrated by Puloski et al39. The probable reason for absence of these deviations was plate pre-modelling. Therefore, the operating theater should have a model tibia to ensure adequate plate modelling, or in unilateral fracture cases, an aluminum modeller may be used to obtain the angulation based upon the unaffected limb.This study contains critical factors. First, there were few proximal and segmented tibial fractures, making it impossible to obtain a discerning statistical analysis. As shown in the literature, the worst outcomes are related to proximal tibial fractures. The second factor concerns the reduction method used. The method chosen (manual traction, calcaneous traction with Kirschner wires, traction table, distractors, or external fixators) may have affected the final outcome38-40. Another study weakness was not performing CT scan of patients who underwent tibial nailing to compare results.As strengths, this survey attempts to highlight this possible complication for orthopaedic surgeons and signal the need for plate modelling and fracture reduction prior to plating, such as with a distractor or an external fixator, to minimize the risk of rotational deformity.
5. Conclusions
- The authors observed that when computed tomography is used to measure tibial rotation, high energy fracture patterns (open fractures and AO Type C) treated using thebridge-plating technique presented the greatest tendency for rotational deviation. External rotation was twice as frequent as internal rotation.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML