-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Surgical Research
2012; 1(1): 1-6
doi: 10.5923/j.surgery.20120101.01
Autotransplantation of A Third Molar with Complete Root Development: A Case Report
1Iranian Center for Endodontic Research, Dental Research Center, Shahid Beheshti University of Medical Sciences, Tehran, 1983963113, Iran
2Dental Research Center, Shahid Beheshti University of Medical Sciences, Tehran, 1983963113, Iran
Correspondence to: Saeed Asgary , Iranian Center for Endodontic Research, Dental Research Center, Shahid Beheshti University of Medical Sciences, Tehran, 1983963113, Iran.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Autogenous transplantation is a feasible, fast and economical option for the treatment of missing teeth when a suitable donor tooth is available. This paper presents successful autotransplantation of a hemisected mature mandibular third molar (tooth #48) with complete root development used to replace a maxillary second molar (tooth #17). The maxillary second molar was deemed non-restorable due to a vertical root fracture in mesial root. Root canal therapy was first performed on the mesial root of the mandibular third molar before the two extractions to minimize post-treatment irritation. After extraction of maxillary second molar, the mandibular third molar was hemisected and the mesial root was placed into the recipient site. After one year, clinical and radiographic examinations revealed satisfactory outcomes with no signs or symptoms suggestive of pathology. In selected cases, autogenous tooth transplantation, even after complete root formation of the donor tooth, may be considered a practical treatment alternative to conventional prosthetic rehabilitation or implant treatment.
Keywords: Autogenous, Autotransplantation, Endodontic, Molar, Tooth, Transplantation
Article Outline
1. Introduction
- The replacement of missing or extracted permanent teeth has always been a challenge for dentists[1]. Autotransplantation refers to the repositioning of autogenous erupted, semierupted or unerupted tooth, from one site into another in the same individual[2]. This is a possible treatment option for the replacement of missing or extracted permanent tooth, for example, in cases of congenital tooth agenesis, malformation, unrestorable caries or traumatic injuries, periodontal disease, ectopic eruption, and endodontic failure[3,5]. Despite the widespread use of dental implants, autogenous tooth transplantation is frequently performed to replace missing mature teeth[6-8] It is still a useful procedure, specifically for adolescents as implants and other prosthetic replacements may not be indicated[1,9-11]. The earliest case reports of tooth autotransplantation date back to 1950s[12-13]. The procedure involves atraumatic removal of a donor tooth, creation of a socket at the recipient site, and replantation of the tooth into the new position. In mature teeth, root canal therapy (RCT) is also necessary[14]. The transplanted tooth can serve as a normal tooth when the procedure is successful[15]. Therefore, in addition to improved esthetics and mastication, successful tooth transplantation offers arch space maintenance and preserves the volume and morphology of the alveolar bone[1,16]. The cost is also considerably low in comparison to advanced treatment options such as dental implants and/or prosthetic replacements; moreover, it can be performed as a single-step surgical procedure. From an orthodontic point of view, the desirable aspect of autotransplantation is that it allows orthodontic movement[4]. Provided that case selection is carried out meticulously, autotransplantation can serve as a feasible, fast and economical treatment option for patients[6]. A multitude of factors influence the success rate; including developmental stage of the root, type of tooth, surgical trauma, the time tooth is preserved outside of the alveolar bone, the shape/site of the recipient socket, and vascularity of the recipient bed. Last but not least, periodontal ligament (PDL) healing plays an extremely critical role in success[14,17-19]. Pulp regeneration, however, only occurs in developing teeth[20-22]. Viability of PDL cells may be affected during extraction or by extra-oral factors such as variable pH, osmotic pressure, and dehydration[22]. Therefore, special attention should be paid to preserving the PDL. A donor tooth chosen for autotransplantation should be of limited value in the dentition, e.g., a third molar[23]. This case report presents successful transplantation of a third molar with complete root formation.
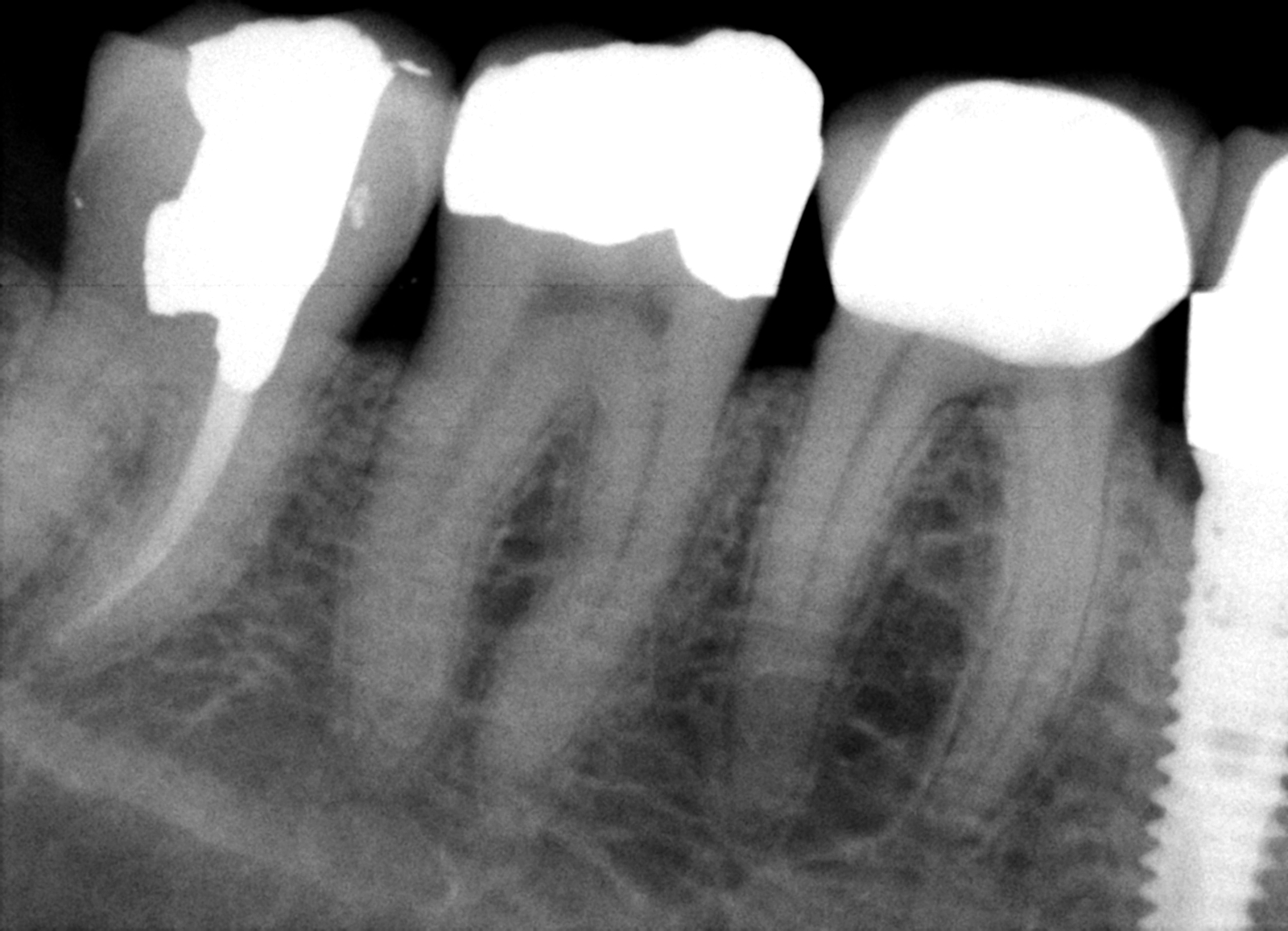
 | Figure 1. Periapical radiograph showing maxillary right second molar |
2. Case Report
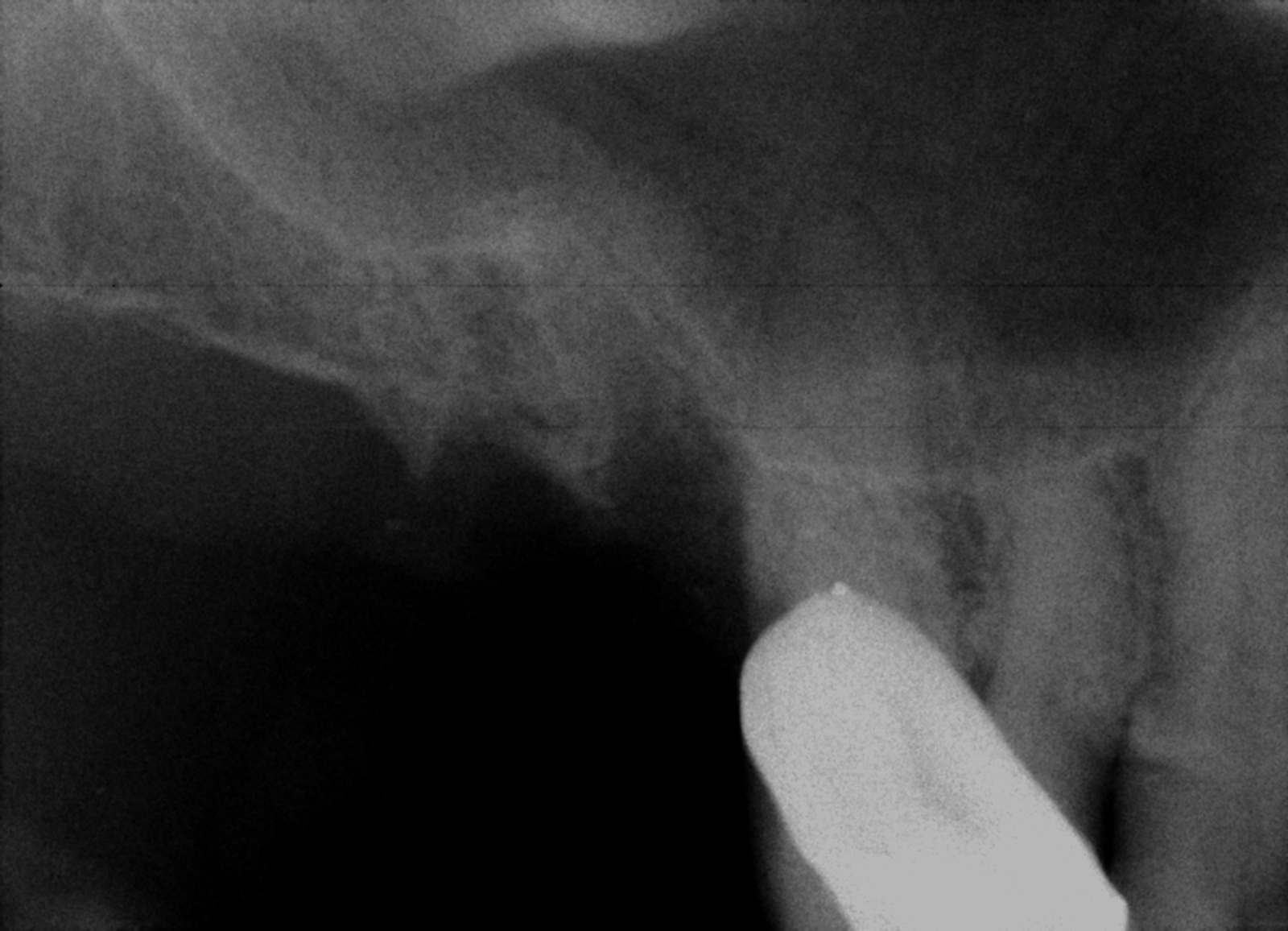
- A 52-year-old male presented with vertical root fracture in the maxillary right second molar (#17). The tooth had previously received RCT. The palatal root was amputated and the tooth was restored with a post and crown. The patient referred to us one day after the tooth fractured which was subsequent to loss of the crown. The tooth was not restorable and extraction was indicated (Figure.1). Tooth #48 was present and completely erupted, and therefore, suitable for autotransplantation (Figure.2). Clinical and radiographic examinations showed that both the donor and recipient tooth and sites were suitable for transplantation (Figure.3). The patient was not medically compromised. An informed consent form was signed by the patient after thorough explanation of risks and benefits of the procedure.
 | Figure 2. Periapical radiograph showing mandibular right third molar |
 | Figure 3. Preoperative panoramic radiograph showing donor mandibular right third molar |
 | Figure 4. Postoperative periapical radiograph showing RCT of the mesial root of mandibular right third molar |
 | Figure 5. Postoperative periapical radiograph showing extraction site of the maxillary right second molar (recipient site) |
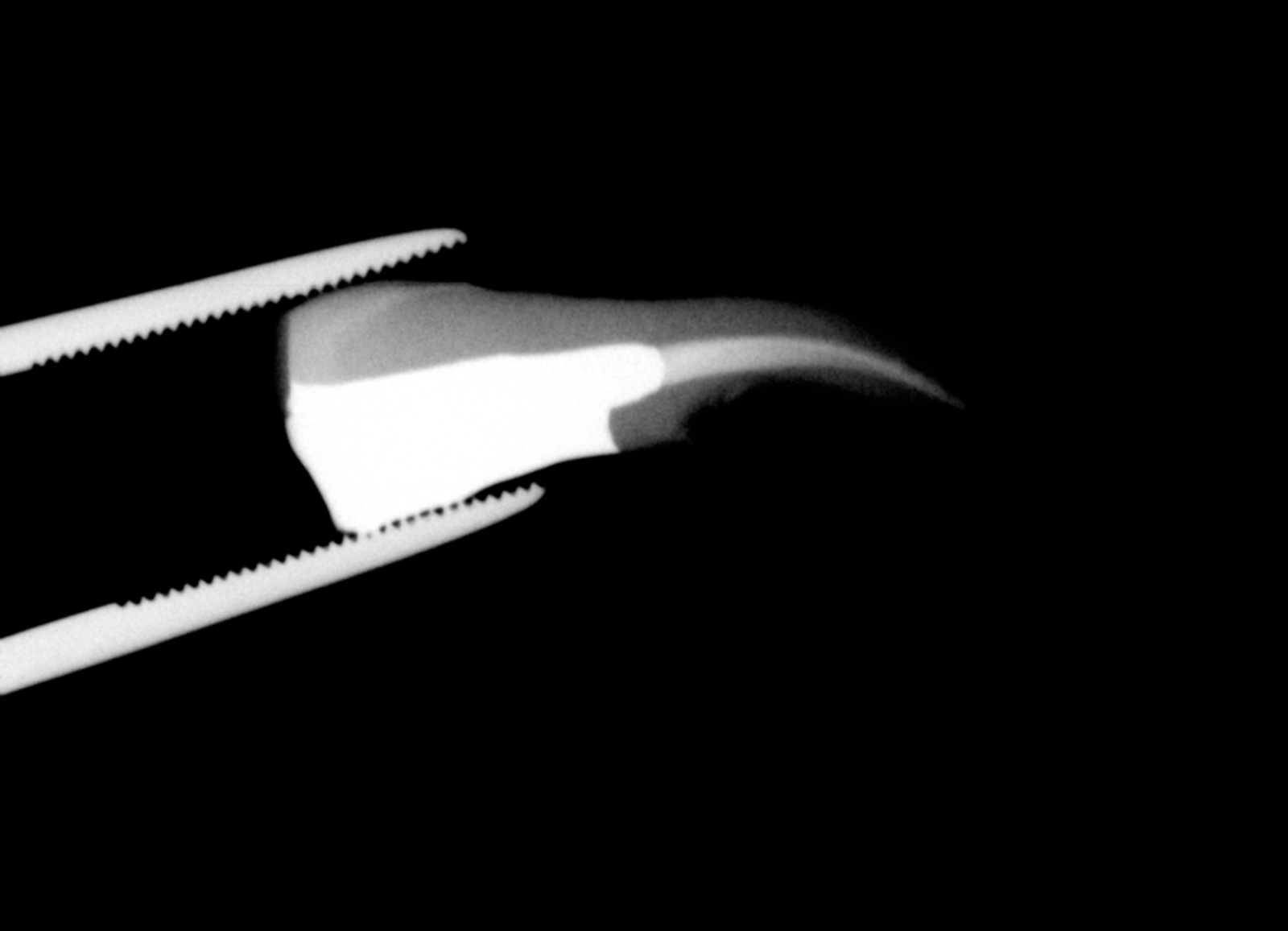 | Figure 6. Radiograph showing hemisected mesial root of the mandibular right third molar (donor) |
 | Figure 7. Immediate post-operative periapical radiograph showing transplanted autogenous tooth in place. |
 | Figure 8. Panoramic radiograph taken 1-year after treatment showing successful outcomes. |
3. Discussion
- The success rate of autogenous tooth transplantation in initial reports has been approximately 50%[4] and therefore, this procedure was not a common treatment option for patients. In addition, etiology of root resorption in transplanted autogenous teeth was not widely understood. In the past few decades, root resorption, its prevention and the healing process of periodontal tissues have been examined by a host of investigators and the success rate of transplantation procedure has increased rapidly from 67% to 84%[24-25]. Like other surgical procedures, careful case selection and treatment planning is essential for successful autotransplantation. The donor tooth and recipient site should be both examined meticulously for suitability and fittingness[26-27]. The recipient site should have adequate bone support with sufficient attached keratinized tissue to allow tooth stabilization and be free of infection and/or inflammation[27]. Insufficient buccolingual width in the recipient site or excessive preparation of the site may result in resorption of the alveolar ridge, loss of buccal bone coverage and consequent loss of periodontal integrity. An extensive study that evaluated autotransplantation of fifty third molar teeth with developed roots reported that lack of buccal bone plate was the only significant predictor of transplant failure[28]. In the present case, the recipient sites had sufficient bony support and keratinized mucosa to enhance post-operative stability.The patient in this report wished to save his tooth, however, he was not as young as most cases reports of autotransplantation in literature[14,22,29-31]. Patients 15-19 years of age are considered to be more appropriate candidates for third molar transplants[16].Preservation of the periodontal ligament cells is critical for the success of a tooth transplant[9,18,32-34]. Accordingly, teeth which have sharp root curvatures are not good candidates for transplantation because there is an increased risk of PDL damage during extraction[26,35]. The extraction procedure in this case was carried out with special care to minimize injuries to the PDL and cementum. The preparation of the recipient socket requires an extended time period; more than half an hour in most cases[4]. Moreover, the procedure often involves fitting the tooth to the bone socket which may then damage the periodontal ligament and root surface. In this case, the mesial root of the donor tooth had the same shape and size of the mesiobuccal root of the recipient site and the socket did not require preparation.The periodontal ligament is extremely sensitive, and its survival ability is significantly reduced if the extraoral dry time is prolonged[4]; this effect has been demonstrated to be significant after 18 minutes[18,36]. The increased length of the extra-alveolar period/time, increases the possibility of inflammatory replacement resorption, reduces the healing capability of the periodontal ligament cells which in turn induces unfavourable consequences such as inflammatory external root resorption. In the present case, the extraalveolar time of the transplanted tooth was kept to a minimum (approximately 5 minutes) as it was extracted and hemisected when the recipient socket was ready for transplantation. After autotransplantation of permanent teeth with fully developed roots pulpal revascularization or revitalization is not expected[20-21]. Previous studies have shown a high incidence of pulp necrosis in mature teeth. Therefore, root canal therapy or root-end filling has been advised to prevent pulpal infection and/or inflammation and subsequent root resorption[6,16,28,37]. Routinely, root canal therapy is performed a few weeks after transplantation[16]. However, Bae et al. recommend that if the donor tooth is easily accessed, root canal therapy should be performed before transplantation[4]. This study conducted root canal therapy before extraction of the donor tooth as this may minimize post-operative intervention and may improve the healing process of the periodontal ligament, thus increasing the chances of long term success. Effective and successive transplantation requires proper adaptation between shape and size of the donor teeth with the donor site[26]. It has also been postulated that maxillary transplants have greater risk of failure due to the wide variation in the size and shape of the teeth and the proximity of the maxillary antrum to the molar sockets[4]. In this case, however, the tooth to be transplanted fitted the recipient site, thus the procedure caused minimal trauma. In addition, the favorable cervical adaptation between the tooth and bone decreased the chance of infection and increased the likelihood of an uneventful healing and periodontal reattachment. Moreover, because of the shape similarity between the tooth and bone socket, fixation was not used.Patient in this case report did not receive prophylactic or postoperative antibiotics as he did not suffer from systemic diseases which indicate prophylactic antibiotic prescriptions.It can be assumed that the physiologic mobility of the transplanted tooth stimulated the activation of periodontal ligament cells (i.e. fibroblasts, cementobalsts and osteoblasts) and bone repair[4]. The transplanted molar tooth in the present case had complete developed roots, which encourages transplantation in these teeth. Both clinical and radiographic outcomes were considered satisfactory after one year.
4. Conclusions
- Although autotransplantation is not very common in general dental practice, it may be regarded as a different, but clinically feasible and economic treatment modality compared to complicated prosthetic treatment. Careful case selection, atraumatic surgical technique, and meticulous adherence to the biologic principles of healing can result in satisfactory outcomes.
ACKNOWLEDGMENTS
- The authors wish to thank staff of Iranian Center for Endodontic Research who assisted in the preparation of this report.
Conflict of Interest
- The author(s) declare no conflict of interests
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML