-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Stroke Research
2020; 6(1): 1-4
doi:10.5923/j.stroke.20200601.01
Received: August 2, 2020; Accepted: August 20, 2020; Published: August 29, 2020

Stroke Pre and Post-Cardiac Event; a Predictive or a Prognostic Factor
Wesam A. Alhejily1, Mohammed A. Almekhlafi2
1Departments of Medicine (Division of Cardiology), Faculty of Medicine, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
2Departments of Neurology, Faculty of Medicine, King Abdulaziz University Hospital, Jeddah, Saudi Arabia
Correspondence to: Wesam A. Alhejily, Departments of Medicine (Division of Cardiology), Faculty of Medicine, King Abdulaziz University Hospital, Jeddah, Saudi Arabia.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

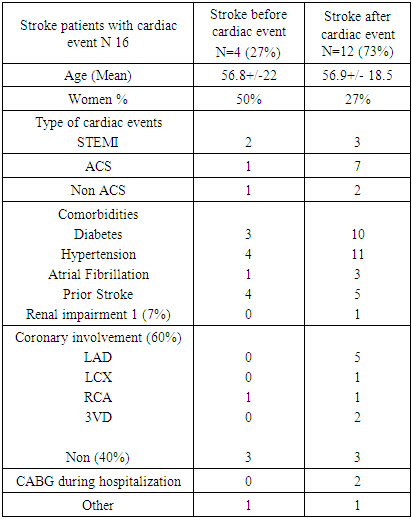
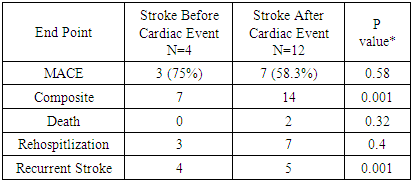
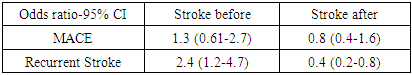
Background: Cerebral and cardiovascular events can occur simultaneously in a patient and with differential timing. Despite large studies addressing the presence of one diagnosis preceding the other, there are no comparative studies that address the impact of stroke timing difference on coronary event and its subsequent outcomes. In this study we sought to describe the association of cerebrovascular and cardiac events and the impact of the order of the occurrence of these events on patients’ outcomes. Methods: A retrospective longitudinal cohort studyin a single tertiary center (King Abdulaziz University Hospital) from two separate databases were crossed matched to identify patients with both diagnoses, then temporal relationships were identified on both directions (stroke before or after cardiac event). Cardiac events include any suspected acute coronary events that triggered referral for coronary angiogram. We included all patients who underwent coronary angiogram and had a primary admitting diagnosis of stroke. The primary endpoint was the incidence of major adverse cardiac event (MACE), the secondary endpoint was a composite of death, recurrent stroke and rehospitlization within 30 days. Risk assessment was evaluated using odds ratio at 95% confidence intervals. Results: Among 500 stroke patients and 6300 cardiac patients admitted in the span of 5 years, 16 patients were identified with both diagnoses, all had ischemic strokes. The mean age was 56.9±18.5 years, 37.5% were females. The most common cerebrovascular risk factors were hypertension (94%) diabetes (81%), atrial fibrillation (25%), and renal impairment (6%). When classified based on stroke timing, a quarter (n=4) of patients had stroke pre cardiac event (SPRE) and 75% (n=12) had stroke post-cardiac event (SPOST). Comparatively major adverse cardiac events were similar on both group (p=0.58) odds ratio of MACE was 1.3 95% CI (0.6-2.7) vs. 0.8 (0.4-1.6) for patients in the SPRE and SPOST cohorts, respectively. Secondary composite endpoint of death, recurrent stroke and rehospitlization within 30 days was higher in the SPRE group (p=0.0001. This was primarily driven by increased risk of recurrent stroke; odds ratio 2.4 (1.2-4.7) vs. 0.4 (0.2-0.8). The mean time from stroke to cardiac event was 89.5 days compared to 40.5 months from cardiac event to stroke. Conclusions: In this cohort of patients with the diagnoses of both stroke and cardiac events, timing of stroke predicts and prognosticates future outcomes in a differential manner as stroke occurrence before a cardiac event (SPRE) tends to cause more recurrent strokes and possibly more cardiac events than its occurrence after a cardiac event (SPOST). Limitations: This was a small cohort identified retrospectively from a single center.
Keywords: Stroke, Myocardial infarction, Timing, Death, Rehospitalization
Cite this paper: Wesam A. Alhejily, Mohammed A. Almekhlafi, Stroke Pre and Post-Cardiac Event; a Predictive or a Prognostic Factor, International Journal of Stroke Research, Vol. 6 No. 1, 2020, pp. 1-4. doi: 10.5923/j.stroke.20200601.01.
1. Background
- Stroke is an important complication following myocardial infarction (MI). There is a large body of clinical evidence to describe the temporal relationship between both particularly in the first 30 days [1]. As previously proven in many studies, myocardial infarction is a predisposing factor for embolic stroke [2,3] particularly in diabetic, hypertensive and patient with atrial fibrillation. The size of myocardial infarction in addition to impaired renal function are independent predictors for increased mortality [4]. In a large recent cohort of patients, the mortality among patients with ischemic stroke was higher compared to ischemic cardiac event [5]. In a smaller series, 0.5% of patients sustained acute stroke in acute MI setting compared to 1.6% of MI presenting as a stroke. Among all patients who suffered a stroke following MI, 22% of "these strokes occurred at the time of MI admission [6]. In the MAGneisum In Coronaries (MAGIC trial) 9% of patients with ST segment-Elevation-Myocardial Infarction (STEMI) had a stroke prior to presentation. In this series, in-hospital stroke, severe congestive heart failure, and 30-day mortality were higher among patients with prior stroke [7]. Albeit the association of stroke with MI is proven, there is limited data comparing the impact to timing of stroke pre or post MI (when both diagnoses) exists on outcomes of patients. In this study, we systematically reviewed the coexistent temporal relationship between stroke and cardiac events on both directions to address the differences in clinical presentations and outcomes.
2. Methods
- Two separate databases (stroke and cardiac) were crossed matched to identify patients with both diagnoses, and then temporal relationships were identified on both directions (stroke before or after myocardial infarction or other cardiac related event). The details of the stroke database have been published before [8]. In brief, this was a retrospective longitudinal cohort of all patients with the admitting diagnosis of stroke hospitalized at King Abdulaziz University Hospital between January 2010 and December 2014. All adult patients with ischemic or hemorrhagic strokes were included. Patient’s characteristics as well as clinical data were gathered. Primary end point was any major adverse cardiac event during or after the initial hospitalization. Secondary endpoint was the composite of death, recurrent stroke or rehospitilization within 30 days. A 2x2 factorial Analysis of Variance (ANOVA) was used to look for difference in variance across the means. Risk assessment was done using odd ratios and 95% confidence intervals (CI). All tests were two-tailed with a p-value of < 0.05 for significance.
3. Results
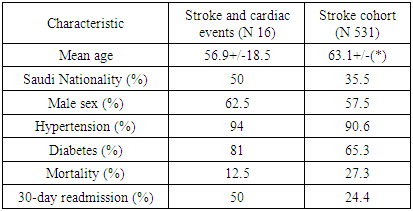
- Cross-matching 546 stroke patients and 6300 patients who underwent cardiac catheterization, we identified 16 patients. The mean age of these patients was 56.9±18.5 and female represented 37.5%. The most common vascular risk factors were hypertension (94%) diabetes (81%) new onset atrial fibrillation (25%), and renal impairment (6%) (Table 1).
|
|
|
|
4. Discussions
- This study is among the first to address the difference in outcomes related to timing of stroke when both cerebral and cardiac events occur. The overall mortality in our cohort was nearly half that observed in previous studies (12.5% vs. 24%) [9]. This can be explained by having younger patients with mean age (56.9 compared to 65), the small number of patients (as only 16 patients 3/100 stroke patients and 3/1000 cardiac patients) and stroke type which was ischemic of athero-embolic nature rather than hemorrhagic strokes which carries worse outcomes. Meanwhile, mortality related to cardiac event at our center is only 2.5-5%; and 30-day-rehospitlization was higher in patients with the combined diagnoses compared to stroke only patients (50% versus 24%). Risk factors like diabetes hypertension and atrial fibrillation were prevalent and well-balanced between both groups. However multiple nuances exist that discriminate one from the other. For example, there were more females and more anterior infarcts in the SPOST than the SPRE group. There were more strokes leading to a cardiac event than cardiac events leading to stroke. For mortality, there were only two deaths in the SPOST group, the major adverse cardiac events were not different between the groups. However, proportionally SPRE has more MACE than SPOST. For the secondary outcomes, recurrent stroke appears to be statistically significant and more in the SPRE than the SPOST and enough to drive the composite end point to significant value (p value < 0.05). We observed that the mean time of cardiac event following stroke was shorter than that of stroke following a cardiac event by 14 times. Prior studies mostly reported on the incidence of stroke during cardiac hospitalization but did not follow patients longitudinally [10-13]. In these reports, stroke within 24-hours of coronary interventions were related to underutilization of parenteral antiplatelet agents while those occurring days after were associated with cardioembolic sources from large infarcts like anterior MI, low ejection fraction, or diabetes. Hemorrhagic strokes were observed in a much close relationship to coronary interventions compared to ischemic strokes that are relatively delayed. However, we did not observe any hemorrhagic strokes in our cohort. This could be partially related to the fact that none of our patients with prior stroke were treated with thrombolytic therapy when presented with ST-Elevation MI. Our study has advantages and some limitations. It investigated a clinical question that has not been adequately addressed in the literature with no data exists in our geographical area. A major limitation is the retrospective nature of the study. However, it could be argued that we used hard outcomes to minimize any biases related to that. Nonetheless, patients who suffered future events after a stroke or cardiac events and readmitted to a different center were not captured in our databases. The small number of patients who cross-matched between the stroke and cardiac databases has affected the power of the statistical tests. This, however, is in accordance with previous literature that reported low frequency of stroke in patients with cardiac events [13].
5. Conclusions
- Stroke timing before cardiac event has impactful and differential effect on the outcomes of patients with strokes or cardiac events. Those patients warrant more attention, early risk stratifications and prompt intervention. Further multi-center studies with larger sample size are advised to confirm our findings.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML