-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2022; 12(3): 73-80
doi:10.5923/j.sports.20221203.03
Received: Oct. 20, 2022; Accepted: Nov. 23, 2022; Published: Dec. 6, 2022

The Effect of Chronic Ankle Instability (CAI) on Athletes’ Gait and Muscle Activity (EMG): A Systematic Review and Meta-Analysis
Christina Martzivanou1, Dimitrios Varvarousis1, Dimitrios Dimopoulos1, Georgios Ntritsos2, Nikolaos Giannakeas2, Georgios I. Vasileiadis1, Athanasios Kyritsis1, Avraam Ploumis1
1Department of Physical Medicine and Rehabilitation, University of Ioannina, Ioannina, Greece
2Department of Informatics and Telecommunications, University of Ioannina, Arta, Greece
Correspondence to: Christina Martzivanou, Department of Physical Medicine and Rehabilitation, University of Ioannina, Ioannina, Greece.
| Email: |  |
Copyright © 2022 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Background: The purpose of this study was to evaluate the effect of chronic ankle instability (CAI) on gait and muscle activity (EMG) of athletes. This review focused on the chronic ankle instability (CAI) caused by ankle sprains during athletics. Methods: This review and meta-analysis included 10 studies level I-III: randomized controlled trials (RCT), observational or descriptive laboratory studies and case-control studies. All injured-athletes were compared to healthy controls. Differences in muscle activation between the two groups have been retrieved and documented. Results: Each study demonstrated significant reduction of activation of the affected muscles near the ankle sprain. Overall, the EMG amplitude of peroneus longus (PL), tibialis anterior (TA) and in some cases that of gastrocnemius medius (MG) were decreased after the initial injury, causing the instability of the ankle joint. Conclusion: Despite the differences in how many ankles sprains each athlete has had, all participants revealed significant reduction in muscle activation, specifically that of peroneus longus, thus altering their gait pattern. Significance: The importance of understanding which muscles are activated after an injury is vital not only for post-injured rehabilitation, but furthermore for preventing such injuries and helping young athletes to get back on truck on pursuing their athletic careers.
Keywords: Athletic, Injuries, Electromyography, EMG, Gait, Chronic ankle instability, CAI
Cite this paper: Christina Martzivanou, Dimitrios Varvarousis, Dimitrios Dimopoulos, Georgios Ntritsos, Nikolaos Giannakeas, Georgios I. Vasileiadis, Athanasios Kyritsis, Avraam Ploumis, The Effect of Chronic Ankle Instability (CAI) on Athletes’ Gait and Muscle Activity (EMG): A Systematic Review and Meta-Analysis, International Journal of Sports Science, Vol. 12 No. 3, 2022, pp. 73-80. doi: 10.5923/j.sports.20221203.03.
Article Outline
1. Introduction
- Chronic Ankle Instability, shortly known as CAI, is caused by repeated episodes of ankle sprains during sports involving a “dynamic manoeuvre” [1]. According to Doherty et al. [2], a great number of individuals (the number reaching almost half of them) are sustaining an ankle sprain [3] [4]. Besides that, joint instability, pain, swelling, loss of function and gait alteration are chronic residual symptoms often lasting for a life-time [5]. In this systematic review, collected data in the past 20 years have been documented and analysed. The review, consisting of 10 clinical studies reports on information about the participants, their mean age and CAIT score, and their performed tasks. The muscle activation of lower extremity in athletes with chronic ankle instability, after an ankle sprain injury, was measured with the use of attached electrodes. A surface electromyography (sEMG) was placed on the targeted ankle muscles and was compared to the muscular activity of the non-CAI group.The aim of this study was to evaluate the effect of repetitive ankle sprains on gait and muscle activity (EMG) of athletes. This review focused on the chronic ankle instability (CAI) caused by ankle sprains during athletics. Our purpose was to answer the following questions:ü What are EMG changes of injured athletes with CAI and how they affect the muscles around the ankle joint? ü How does the ankle muscular activity of injured athletes with CAI change their gait patterns?
2. Methods
2.1. Protocol and Registration
- In accordance with the PRISMA guidelines [6], our systematic review protocol was registered with the International Prospective Register of Systematic Reviews (PROSPERO) on the 28th of August 2021. The registration number is the following CRD42021270671. The designed study and the noted results were based on the PRISMA statement. Therefore, the review conformed to all PRISMA guidelines and reported the required information.
2.2. Eligibility Criteria
- The research was limited to English articles illustrating the effect athletic injuries have on muscle activity (EMG) and gait patterns of athletes. In order to optimize the relevance and accuracy of our research, we decided to include articles published in the last two decades (2001-2021) which were conducted on humans, specifically adults over the age of 19 years. Another important eligible criterion was the type of articles, e.g., randomized controlled trials (RCTs), cross-sectional studies (CSS), case-control studies, meta-analyses and descriptive or observational laboratory studies.
2.3. Search Strategy
- A computerized literature review was performed including the following databases: MEDLINE, Springer, Research Gate, BMC, Scopus, Cochrane databases. The total number of articles found was 2120 and after filters were applied the number dropped to 418. The last search was conducted on the 15th of December 2021.
2.4. Search
- The medical search algorithm used in MEDLINE, included following keywords: ("sports" [MeSH Terms] OR "sports" [All Fields] OR "athletic" [All Fields]) OR ("sports" [MeSH Terms] OR "sports" [All Fields] OR "sport" [All Fields]) AND ("injuries" [Subheading] OR "injuries" [All Fields] OR "wounds and injuries" [MeSH Terms] OR ("wounds" [All Fields] AND "injuries" [All Fields]) OR "wounds and injuries" [All Fields]) AND ("electromyography" [MeSH Terms] OR "electromyography" [All Fields] OR "emg" [All Fields]).
2.5. Study Selection
- The systematic search of the electronic databases (Medline, Springer and PubMed) identified a total of 418 studies, 54 of which were selected for full text screening. The inclusion criteria for participants in these studies were following: adults >19 years, presence of an athletic injury, injury on the lower limbs, participants were athletes (professionals and non-professionals). Studies that mentioned and/or examined underage athletes, non-athletic participants, injury on upper extremities, SCI, tendinopathy, peripheral neuropathy, impairment of the CNS (central nervous system), history of fractures, anatomical lesions (osteochondral), peroneal tendon tears, ligament laxity, ACL ruptures or deficiency were excluded from our study. Only ten studies were considered suitable for data extraction and meta-analysis according to the previous eligibility criteria. The flow chart of the study selection process can be seen in Figure 1.
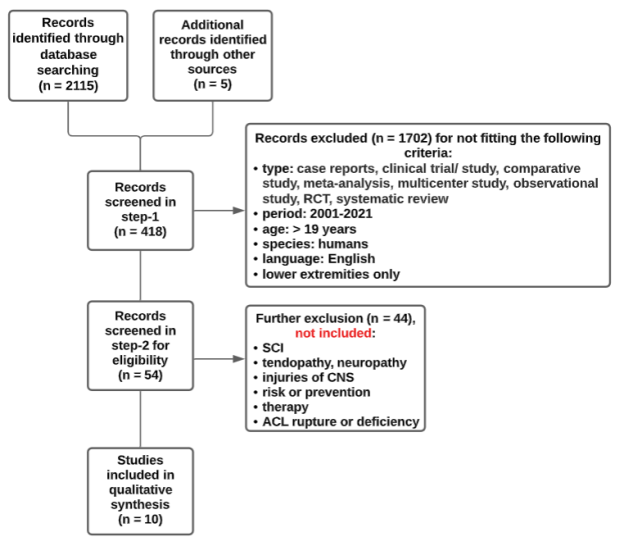 | Figure 1. Flowchart [11] of the process of gathering the published relative literature |
2.6. Data Selection
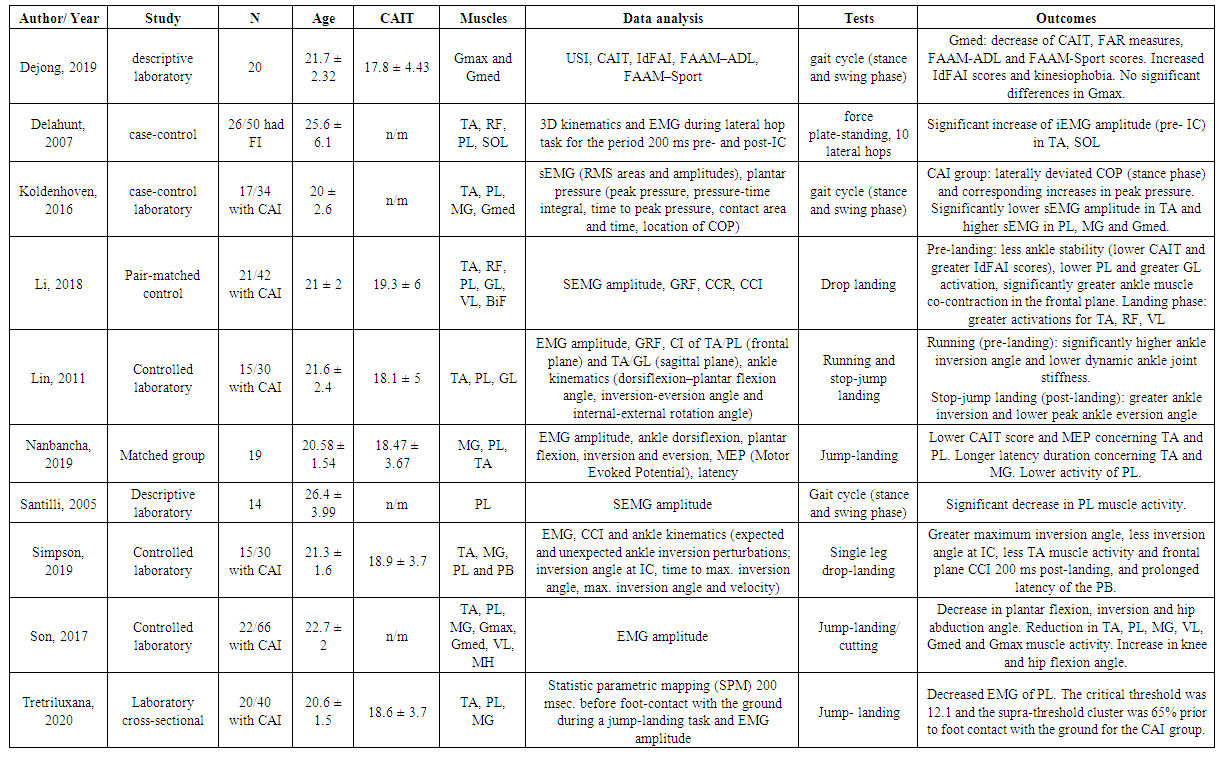
- We extracted individually information on: a) the author and year of publication b) the study-design c) the total number of participants d) the mean age e) the CAIT-score f) which muscles were attached with electrodes g) the data analysis h) undergone tasks by participants and i) the results. Table 1 presents the characteristics of the included studies.
2.7. Statistical Analysis
- We calculated the summary mean differences, along with the corresponding 95% CI, by pooling the study specific estimates using random-effects models [7]. The presence of heterogeneity was estimated with the Cochran’s Q statistic and it was quantified with I [8] [9], when at least 10 studies were included in the meta-analysis. All analyses were performed using Stata (version 14; StataCorp, College Station, TX, [10].
2.7.1. Risk Of Bias
- The reviewers (CM and AP) documented the methodological quality of the studies and extracted the relevant data. The Biostatistician (GNt) assessed the possible small study effects (an indication of publication bias) by visual inspection of funnel plots and Egger’s test, when at least 10 studies were included in the meta-analysis. The PRISMA checklist was applied for the critical appraisal of the studies included, and all articles were examined as full texts.
3. Results
3.1. Systematic Review
- In this systematic review, collected data of 10 clinical studies have been documented and analysed. We focused mainly on prior studies comparing the muscle activity in athletes with chronic ankle instability, after a sequence of ankle sprains, to those with no ankle injury. All injured-athletes were compared to healthy controls. Differences in muscle activation between the two groups have been retrieved and documented. Measurement of lower limb kinetics was performed by using surface electromyography (EMG) on the following muscles: medialis gastrocnemius (MG), rectus femoris (RF), tibialis anterior (TA), peroneus longus (PL), soleus (SOL) and in some cases vastus lateralis (VL), biceps femoris (BF), medial hamstring (MH). The muscle co-contraction index (CCI), which monitors the agonist and antagonist muscles contributing to stabilizing the ankle joint, the Cumberland Ankle Instability Tool (CAIT) and the Identification of Functional Instability Scale (IdFAI) were analysed as well.Table 1 presents the collected information of each study, ordered by the year of publication. Data such as type of study, number of participants, mean age, measured EMG amplitude of specific muscles, Cumberland Ankle Instability Tool (CAIT) score and the task/test that participants had to complete in order to assess the muscular activation, have each been collected and summarised. The participants were in their early to mid-twenties, stated a CAIT- score of <19 and most of them were asked to perform the stop, jump and landing test. The muscle activation of CAI and non-CAI athletes was measured either by surface electromyography (sEMG) and ankle kinematics (dorsiflexion–plantar flexion angle, inversion-eversion angle and internal-external rotation angle) or motor evoked potential (MEP), evident in the study of Nanbancha et al [12].
3.1.1. Results of Systematic Review
- The first article, that of DeJong et al [13], showed a decrease of CAIT of gluteus medius, decreased FAR measures, FAAM-ADL and FAAM-Sport scores. The idFAI scores were increased and no significant differences were seen in the gluteus maximus muscle. The CAI-athletes revealed a kinesiophobia after all. In the study of Delahunt et al [14], a significant increase of iEMG amplitude (pre- IC) in tibialis anterior and soleus was noticed. The study of Koldenhoven [15] on the other hand, resulted in laterally deviated COP (stance phase) and corresponding increases in peak pressure. Significantly lower sEMG amplitude of tibialis anterior and higher sEMG of peroneus longus, gastrocnemius medialis, gluteus medius. Li et al [16] presented following results in the pre-landing phase: less ankle stability (lower CAIT and greater IdFAI scores), lower muscle activation of peroneus longus, greater gastrocnemius lateralis activation and significantly greater ankle muscle co-contraction in the frontal plane. In the landing phase the muscle activation of tibialis anterior, rectus femoris and vastus longus was greater. Moreover, Lin et al [17] showed that in the running task (pre-landing phase) the ankle inversion angle was significantly higher with a lower dynamic ankle joint stiffness. The stop-jump landing test (post landing) revealed a greater ankle inversion and lower peak ankle eversion angle. In addition, Nanbancha et al presented lower CAIT score and MEP concerning tibialis anterior and peroneus longus, longer latency duration concerning tibialis anterior and gastrocnemius medialis. A significant lower muscle activity of peroneus longus in athletes with CAI was displayed as well, something that was common in the study of Santilli et al [18].Simpson and his co-authors [19] demonstrated a greater maximum inversion angle in athletes with chronic ankle instability, less inversion angle at initial contact (IC), less muscle activity of the tibialis anterior and lastly a prolonged latency of the peroneus brevis muscle. Additionally, Son et al [20], found a decrease in plantar flexion, inversion and hip abduction angle, a reduction in muscle activity of the tibialis anterior, peroneus longus, vastus longus, gluteus maximus and medius, gastrocnemius medialis and finally an increase in knee and hip flexion angle. The last study being that of Tretriluxana et al [21], displayed a decreased electromyography of the muscle peroneus longus. In general, the pre-initial contact (200 ms prior) tasks appeared to have:Ø Decreased electromyography of peroneus longus, tibialis anterior, gastrocnemius medialis, vastus longus and gluteus maximus and mediusØ Decrease in plantar flexion, inversion and hip abduction angleØ Increased knee and hip flexion angleØ Prolonged latency of tibialis anterior and gastrocnemius medialis As opposed to the post initial contact (landing phase) tests where following was evident: Ø Slower dynamic ankle joint stiffness Ø Prolonged latency of peroneus brevis Ø Greater ankle inversion Ø Lower peak ankle eversion angle
3.2. Meta-Analysis
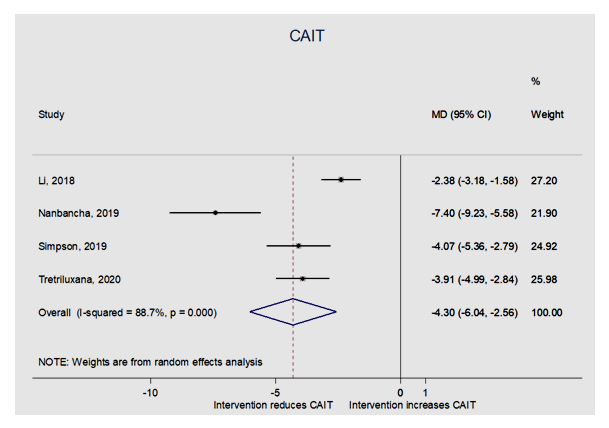
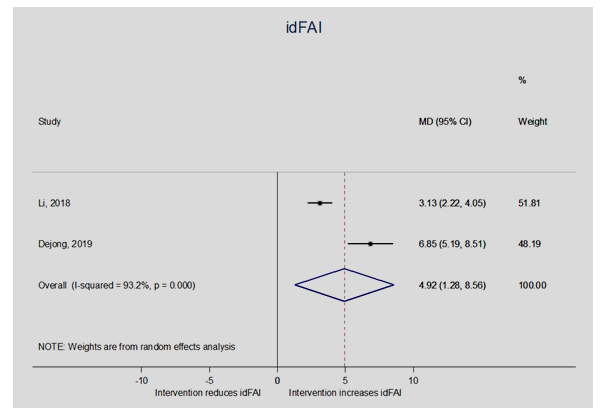
- A meta-analysis was executed on the following 4 outcomes as presented on Table 2 (see Table 2): Cumberland Ankle Instability Tool score (CAIT), Identification of Functional Ankle Instability score (idFAI), co-contraction index (CCI) in sagittal and frontal plane and lastly the Questionnaire of Functional Ankle Ability Measure-Sport Subscale score (FAAM-sport).
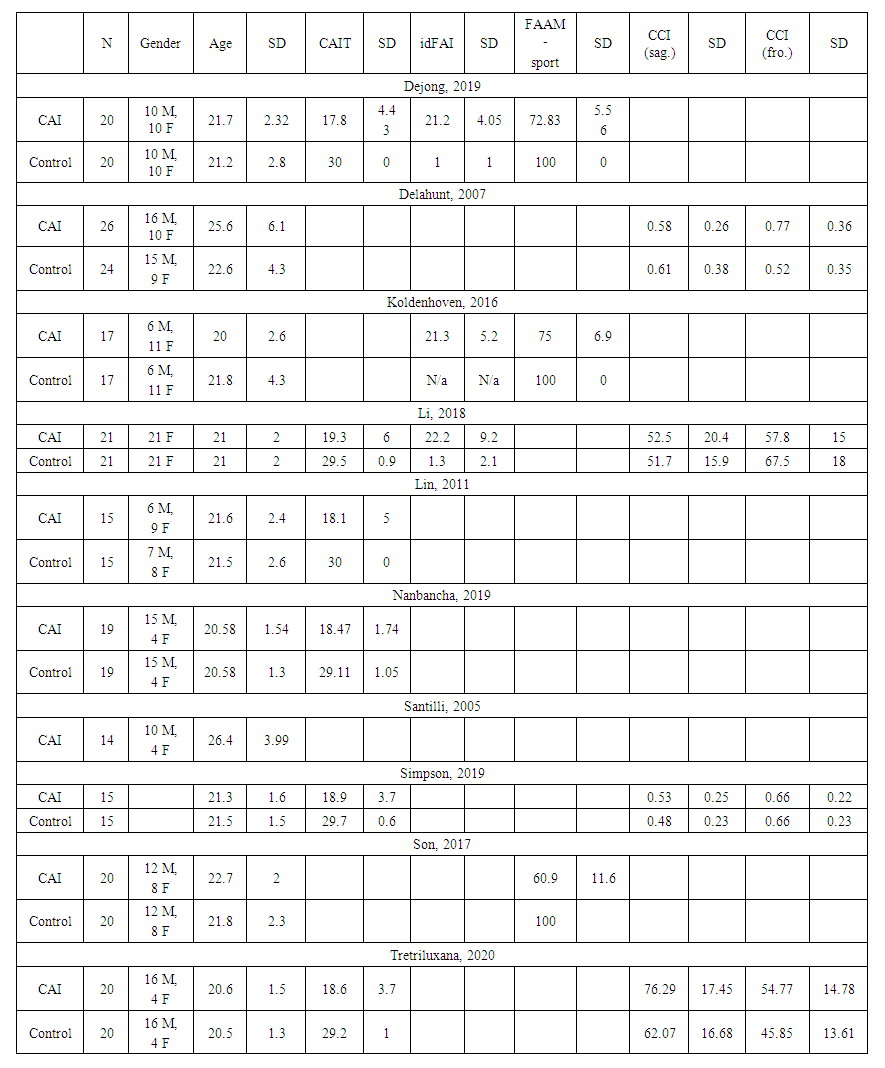 | Table 2. Data collection of CAIT score, idFAI, CCI in sagittal and frontal plane, FAAM-Sports |
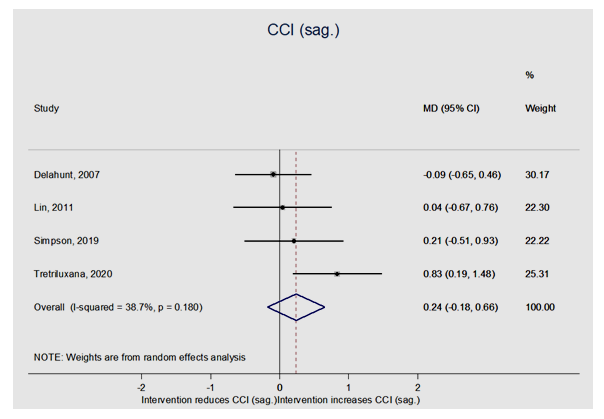 | Figure 3. Data synthesis of the 4 studies measuring the CCI in sagittal plane, however with no statistical significance seen |
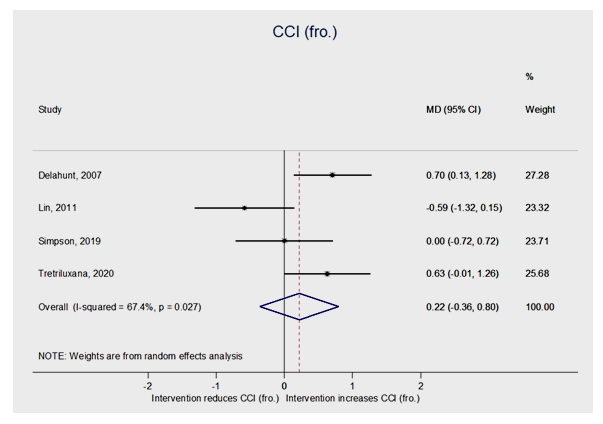 | Figure 4. Data synthesis of the 4 studies measuring the CCI in frontal plane; with no statistical significance as well |
4. Discussion
- The purpose of this study was to evaluate the effect of CAI on gait analysis and muscle activity of athletes. As anticipated, athletes with chronic ankle instability (CAI), displayed different muscular activation in regard to non-CAI athletes. In our meta-analysis, athletes with CAI showed significant lower CAIT scores compared to the non-CAI group. The mean difference with a 95% CI was -4.30 (-6.04; -2.56). The idFAI was significantly higher in CAI-athletes with a mean difference and 95% CI of 4.92 (1.28; 8.56). Due to alterations in biomechanics of lower extremities during high-impact movements (i.e., movements often seen in athletic manoeuvres), the chronic ankle instability shows different neuromuscular control when compared to athletes with no injuries. In the study of Lin et al, this difference is described as a”deficit in feedback neuromuscular control”, where the central nervous system adjustment procedure is delayed. The reason behind the deficient feedback in neuromuscular control being the inability of the ankle to execute the motion normally hence remaining inverted. In addition, the muscles around the ankle joint seem to adapt for maintaining the joint stability in athletes with CAI, through decreasing the activation of the tibialis anterior muscle (TA).Thus said, less ankle stability (lower CAIT and greater IdFAI scores) and lower maximum voluntary isometric contraction (MVIC) moments for ankle dorsiflexors and evertors are documented in athletes with chronic ankle instability. In the pre-landing phase, 200 milliseconds prior to initial foot contact, CAI-athletes displayed altered muscle activation when compared to non-CAI athletes. The EMG demonstrated reduced peroneal longus activation and greater activation of gluteus lateralis. In similar studies, peroneal, gluteus maximus and medius strength-deficits are frequently reported for CAI-patients. A tendency of increased vastus lateralis-activation has also been noticed. The ankle muscle co-contraction was therefore significantly greater in the frontal plane. Differences in muscle activation of the ankle joint were also present in the landing phase. The EMG captured a greater activation of the following muscles: tibialis anterior, rectus femoris and vastus lateralis. There was a tendency of reduced biceps femoris activation and the co-contraction index (CCI) of the ankle muscles was greater in sagittal as well as frontal planes. In our meta-analysis however, we had no statistical significance in both frontal and sagittal planes. Moreover, knee muscle activations such as increase in knee extensor motions and co-contraction ratio (CCR) CAI patients adopted landing positions of less inversion, less plantarflexion, more knee and hip flexion, and less hip abduction angle during the initial contact to mid-landing phase (0%–25% of stance) compared with copers and controls. While increased activation of the tibialis anterior in athletes with CAI could increase the ankle stability in the landing, it could also hinder the ability of ankle energy absorption and further influence the knee biomechanics and muscle activations. Therefore, the changes in ankle muscle stimulation may result in some atypical knee muscle loadings, such as greater co-contraction ratio (CCR) of quadriceps to hamstrings, which was confirmed in our study too.
5. Study Limitations
- There were some limitations to the present study. On the one hand, we have an all-female study which may limit the generalizability of the results to female athletes with CAI and on the other hand they are two studies without any gender-information. Our meta-analysis was limited by the small sample size of the studies. The results could possibly lack of power to adequately justify our findings. There is a need for more research on this topic, with studies that will have a larger sample of patients and use modern technologies to measure gait parameters and muscle activity. Therefore, our results should be considered with a mild degree of alertness in regards to the sample size.
6. Conclusions
- In conclusion, the results of this study confirm altered muscle activation in the lower extremities and different gait pattern in athletes with Chronic Ankle Instability (CAI) when compared to the control groups (coppers). In general, a significant lower CAIT score by CAI athletes was noticed in each of the ten studies relative to non-CAI athletes. Alterations such as reduced peroneal longus activation in the prelanding phase and increased co-contraction of ankle muscles in the landing phase were noticed in athletes with CAI [22]. The modified muscle movements, whether they are reduced or increased, in athletics during exercises may act as a protecting and stabilizing mechanism. Some suggestions involved exercises that stabilize and strengthen the lower limb muscles or proximal musculature during gait-training, but there is a need for more research on this topic, with studies that will have a larger sample of patients and use modern technologies to measure gait parameters and muscle activity.
Conflicts of Interest
- None
Funding
- The project MEGATRON (Megadata analysis of robot-assisted base and 3D camera system for improved kinetic rehabilitation - subproject 1: Implementation and Evaluation - MIS 5047227) is co-funded by the European Union and the Hellenic Republic.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML