-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2020; 10(6): 123-130
doi:10.5923/j.sports.20201006.01
Received: Oct. 5, 2020; Accepted: Oct. 28, 2020; Published: Nov. 15, 2020

Effect of Perceived Fatigue and Workload on Two Mobile Balance Tests
Jordan W. Stafford, Scott E. Ross, Louisa D. Raisbeck, Christopher K. Rhea
Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC, USA
Correspondence to: Christopher K. Rhea, Department of Kinesiology, University of North Carolina at Greensboro, Greensboro, NC, USA.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Mobile balance assessments using sensors in portable devices to objectively measure postural control have become popular in recent years. However, there is a current gap in the literature with respect to how perceived fatigue and perceived workload affect these mobile balance assessments. The purpose of this study was to measure postural control with two objective mobile balance assessments (one for static balance and one for dynamic balance) before and after a standardized fatigue protocol. Healthy participants (N=30, 33.6±14.2 years) completed perceived fatigue/workload assessments along with mobile static and dynamic balance tests before a fatigue protocol (including sprints, pushups, and step-ups) and again four times after the fatigue protocol in windows approximately 9 minutes apart. Outcome measures at each timepoint included the Rating of Perceived Exertion (RPE) for perceived fatigue, NASA Task Load Index (NASA-TLX) for perceived workload, and objective metrics from the Balance Tracking System (BTrackS) Balance Test (static balance assessment) and the AccWalker smartphone app (dynamic balance test). Repeated measures MANOVA/ANOVAs and Spearman’s rho correlations were used to examine the relationship between perceived fatigue/workload and balance before and after the fatigue protocol. The BTrackS Balance Test was affected acutely after fatigue, while AccWalker showed no changes after fatigue. RPE and NASA-TLX were significantly correlated, but nearly all balance metrics were not associated with perceived fatigue/workload. Perceived fatigue and workload acutely affect the BTrackS Balance Test, but not AccWalker, which may help with the selection of a balance test based on the desired assessment characteristics and administration time relative to physical exertion.
Keywords: Balance, Mobile, App, Fatigue
Cite this paper: Jordan W. Stafford, Scott E. Ross, Louisa D. Raisbeck, Christopher K. Rhea, Effect of Perceived Fatigue and Workload on Two Mobile Balance Tests, International Journal of Sports Science, Vol. 10 No. 6, 2020, pp. 123-130. doi: 10.5923/j.sports.20201006.01.
1. Introduction
- Postural control is defined as the ability to maintain upright stance, which is accomplished through a complex and dynamic process that integrates both internal and external factors [1,2]. Humans are, to some degree, inherently unstable, which affords the flexibility to respond to unexpected perturbations that occur in daily life. Thus, a certain level of instability contributes to our ability to functionally interact with the environment and complete tasks associated with activities of daily living or those more specialized in nature. In a healthy system, the postural control response is ideally proportionate to the disturbance to maintain upright stance (i.e., balance) [3,4]. When postural control is compromised, it will exhibit delayed timing and/or reduced magnitude in response to a disturbance [5,6]. It is well documented that postural control instability increases when the neurosensory systems contributing to postural control (vision, vestibular, and proprioceptive) are compromised [7]. Many balance tests have been developed to characterize changes in balance due to natural aging, injury, or disease.The assessment of balance can be characterized as objective or subjective. Traditionally, objective balance tests were confined to laboratory settings due to the need for specialized sensors to be in a controlled environment (i.e., a force plate affixed to a level surface). Alternatively, subjective balance tests were developed to assess postural control outside the laboratory—such as the Balance Error Scoring System (BESS). However, questions about the validity and reliability of the BESS have been raised due to its subjectivity [8-11]. To meet the need of an objective balance test that could be used outside the laboratory, numerous mobile balance tests have been developed [12-23]. While the validity and reliability for some mobile balance assessments have been described, these characteristics are not reported for many of these mobile apps [15]. Moreover, it is unclear the extent to which internal factors that may be present during testing, such as fatigue, may influence the assessment of balance with these mobile devices. Assessing fatigue in conjunction with postural control would help identify the strengths and limitations of mobile balance tests.There is currently no standardized way to objectively measure fatigue. As a result, researchers typically rely on self-reported measures of perceived exhaustion or perceived workload as a surrogate to fatigue. The Rating of Perceived Exhaustion (RPE) has a long history of being used in this context [24]. For the purposes of this paper, fatigue will be referred to as “perceived fatigue” to convey it is the participants’ feeling of fatigue and not an objectively measurable variable, such as heart rate. Relative to perceived workload, the NASA Task Load Index (NASA-TLX) is a multidimensional assessment of the perceived workload associated with a task [25]. The NASA-TLX considers the physical, mental, and emotional factors required to complete a task, and it has been previously used to assess perceived workload in motor behavior tasks [26-29]. Using both RPE and the NASA-TLX as surrogates of perceived fatigue and workload would help address the aforementioned limitation with mobile balance assessments.A commonly used mobile balance assessment is the Balance Tracking System (BTrackS; Balance Tracking Systems, Inc, San Diego, California), which employs a portable force plate interfaced with a tablet or laptop to reliably [30] and validity [31] assess static postural control. Normative data for BTrackS from more than 16,000 people who were 5-100 years old have been published [32]. This mobile balance assessment has been commonly used with athletic populations [33], for which fatigue could be a factor at the time of testing. BTrackS has been shown to be more fatigue resistant than the subjective BESS test [34]. However, the effect of fatigue on the BTrackS balance metric [center of pressure (CoP) excursion] was still observed within 5 minutes of the fatigue protocol. While BTrackS is a viable mobile balance assessment option, it relies on a static balance task. Dynamic postural control is required in many real-world tasks and it may provide a more ecologically valid method to assessment balance. To address the need of an objective and dynamic balance test, a smartphone app was developed that measures postural control while the participant performs a stepping-in-place task [14,35,36]. This test (termed AccWalker) has been shown to be a reliable and valid way to measure postural control [35], as well as a clinically useful tool to identify balance deficits after head trauma [14]. However, the extent to which fatigue affect this dynamic balance test is unknown. The effect of perceived fatigue on the postural control has previously been examined [34,37] and showed the time course that could be expected for balance to return to baseline levels after a fatiguing protocol. However, there were limitations to this previous work. First, both studies used RPE to assess postural control deficits after a fatiguing protocol, but neither study examined the extent to which an increase in RPE related to an increase in postural instability. Second, neither study included a measure of perceived workload, which would add a different dimension of perceived fatigue to the assessment. Third, both studies only used a static postural control task while on a force plate. Therefore, the purpose of this study was to examine the effects of perceived fatigue (measured by RPE and the NASA-TLX) on objective mobile balance tests (i.e., BtrackS Balance Test and AccWalker). It was hypothesized that (1) a decline in postural control will be observed immediately after the fatigue protocol, but will return to baseline levels after 9 minutes and (2) the magnitude of the immediate postural control decline will be associated with an individual’s level of perceived fatigue.
2. Methods
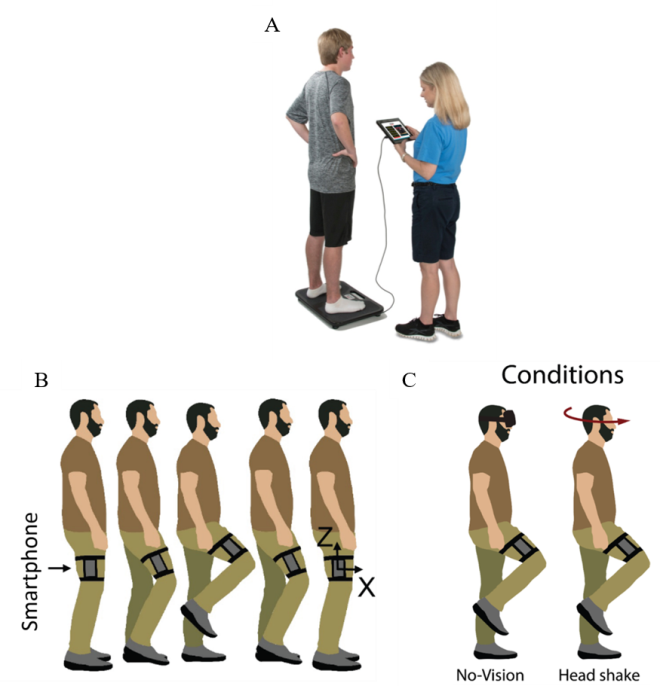
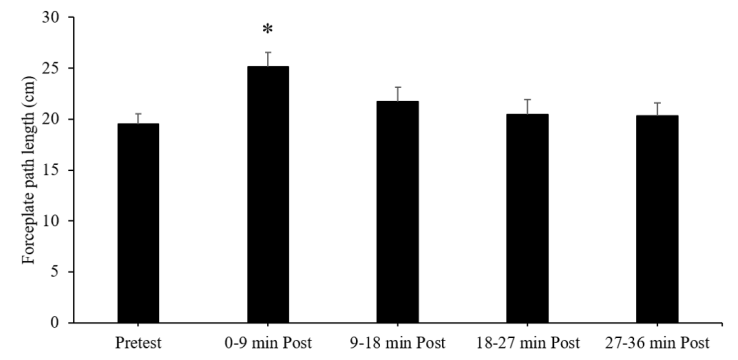
- Participants (N=30, 33.6±14.2 years, 21 females / 9 males) were recruited from the local community. Inclusion criteria included a self-report of current participation in at least three hours of vigorous physical activity per week and no current musculoskeletal injuries. Prior to data collection, participants read and signed an informed consent form. The study protocol and consent form were approved by the local university Institutional Review Board. All participants had on athletic clothes/shoes and completed the same testing protocol: (1) one pre-test assessment of perceived fatigue and postural control, (2) a fatiguing protocol that took approximately 14-minutes to complete, and (3) four post-test assessments of perceived fatigue and postural control spaced out over four windows that were 9-minutes in duration each, which was the shortest window duration possible to complete all of the perceived fatigue and postural control assessments (Figure 1). The postural control assessment in the pre- and post-tests included the BTracks Balance Test and the AccWalker smartphone app.
 | Figure 1. Timeline of experimental procedure protocol |
3. Results
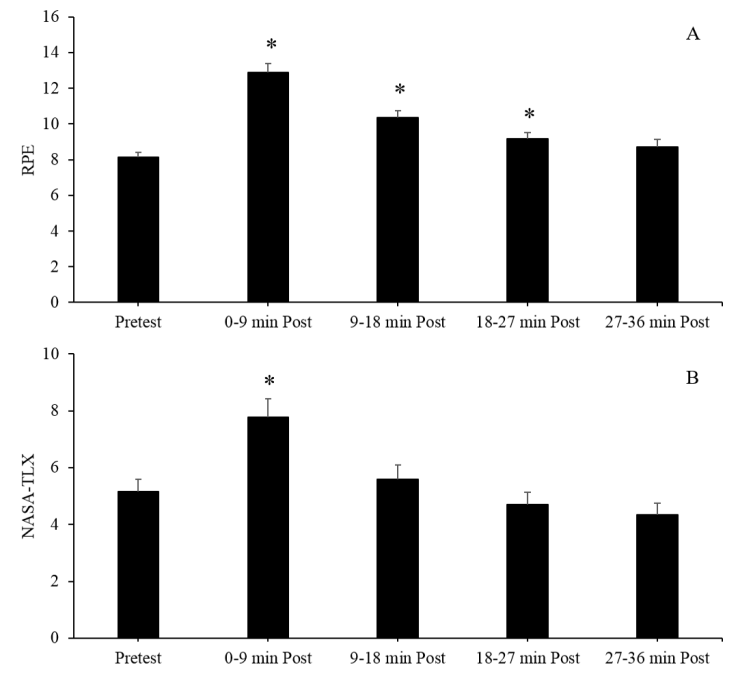
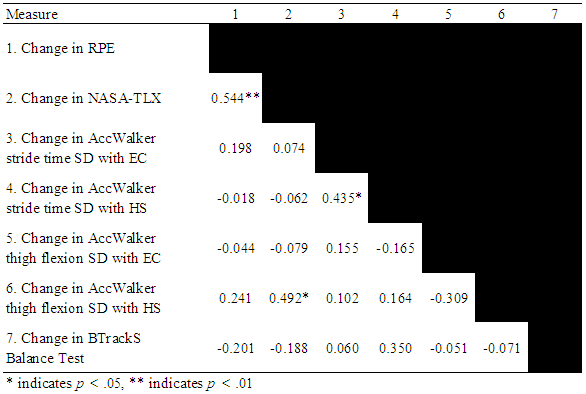
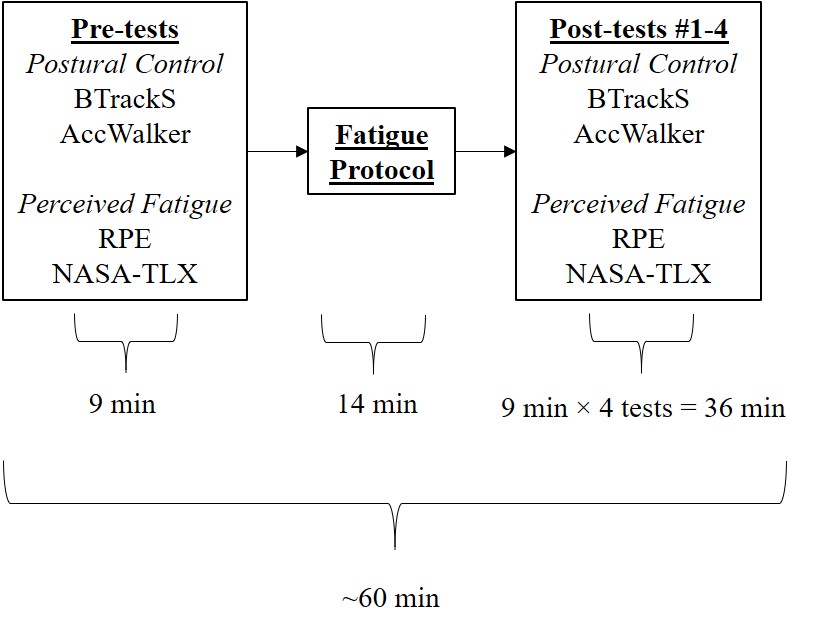
- For perceived fatigue, the MANOVA indicated there was a change across time points, F(8,17) = 11.70, p < .001, Wilk's Λ = 0.154, partial η2 = .846. The follow-up univariate ANOVAs showed both RPE, F(2.05, 49.31) = 36.28, p < .001, partial η2 = .602, and NASA-TLX, F(1.98, 47.46) = 14.16, p < .001, partial η2 = .371, changed across the time points. For RPE, the pairwise comparisons showed a significant increase between the pre-test (8.1±1.6) and the 0-9 min post-test (13.0±2.8). RPE remained elevated at the 9-18 min and 18-27 min post-tests (10.4±2.3 and 9.2±1.9, respectively), returning to the baseline level at the 27-36 min post-test (8.8±2.1) (Figure 3A). For the NASA-TLX, the pairwise comparisons showed a significant increase between the pre-test (5.3±2.4) and the 0-9 min post-test (7.7±3.7), then returning back to baseline levels at the 9-18 min, 18-27 min, and 27-36 min post-tests (5.6±3.1, 4.7±2.4, and 4.4±2.2, respectively) (Figure 3B).
|
4. Discussion
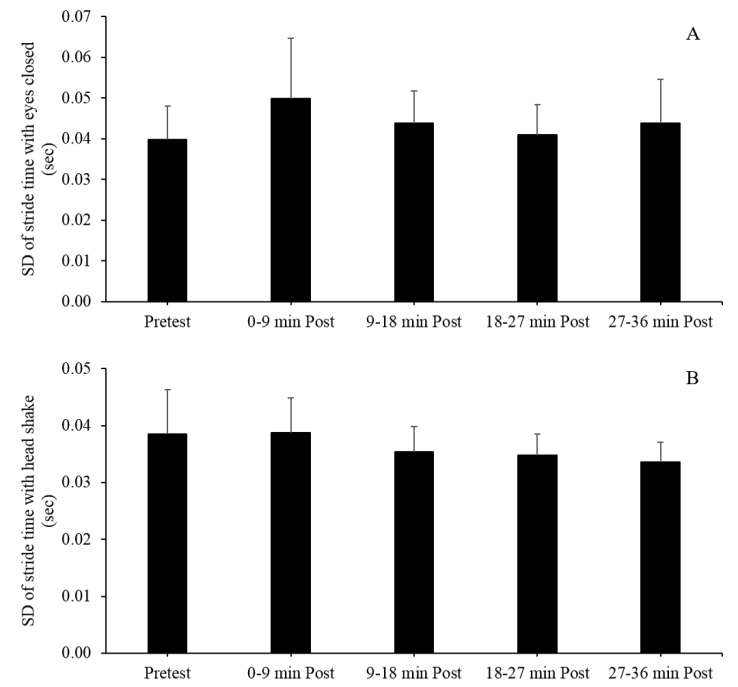
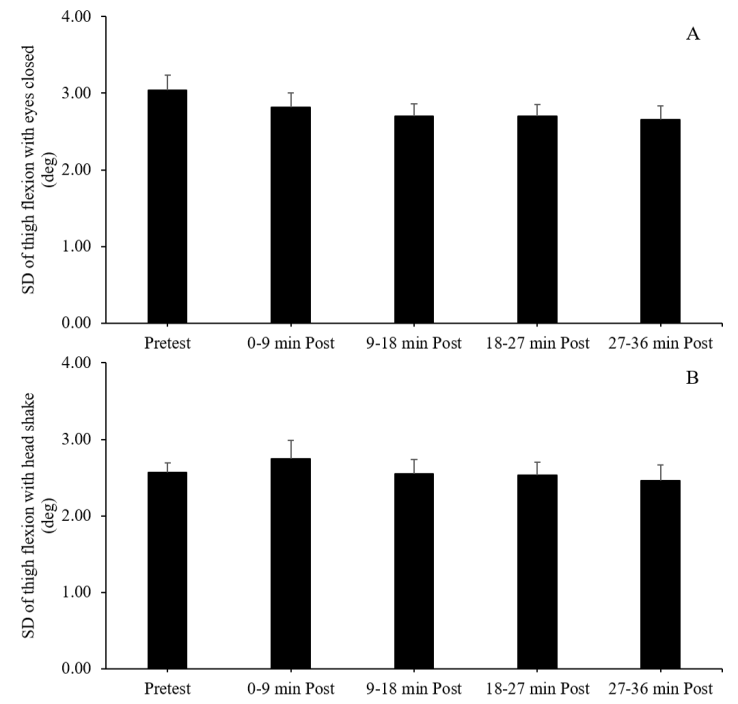
- The purpose of this study was to examine the effects of perceived fatigue and workload (measured by RPE and the NASA-TLX) on objective mobile balance tests (i.e., BtrackS Balance Test and AccWalker). Two hypotheses were tested. Hypothesis one stated that a decline in postural control would be observed immediately after the fatigue protocol but will return to baseline levels after 9 minutes. Data from the BtrackS Balance Test supported this hypothesis, but AccWalker data showed no changes after the fatigue test. Hypothesis two stated the magnitude of the immediate postural control decline would be associated with an individual’s level of perceived fatigue. Data from only one pair of variables (NASA-TLX and AccWalker thigh flexion SD) provided support for this hypothesis. Collectively, the data showed that the BtrackS Balance Test is acutely affected by perceived fatigue, whereas AccWalker showed no changes in performance after the fatigue protocol. The first step in this study was to show that the fatigue protocol led to an increase in perceived fatigue and workload, which was observed in both RPE and the NASA-TLX. Specifically, RPE was elevated up to 27 minutes after the fatigue protocol, but the NASA-TLX was only elevated up to 9 minutes after the fatigue protocol. While a similar elevation in fatigue and workload was observed acutely — evidenced by the positive correlation in the change in RPE and NASA-TLX tested in hypothesis two—the rate at which perceived physical fatigue (indexed by RPE) and perceived workload (indexed by NASA-TLX) recover appear to be at different after the fatigue protocol. Some studies using subjective/perceived fatigue measures have used both RPE and NASA-TLX to measure how fatigue affects manufacturing tasks [38] and cycling tasks [39]. To our knowledge, this is the first study comparing the relation between perceived physical fatigue and perceived workload after a physically demanding protocol and our data suggest they degrade at different rates after physical exertion. The relatively fast rate of recovery in the NASA-TLX measure may indicate that cognitive workload may be less affected by a more physically fatiguing task. In addition, the NASA-TLX asks more questions, therefore, it may elicit a more specific profile of fatigue instead of the single numeric measure afforded by RPE.The BTrackS Balance Test and AccWalker test are both mobile balance assessments that objectively measure postural control. The BTrackS Balance test uses a portable force plate, which measures the displacement of the CoP over 20 second trials and the total distance travelled by the CoP was used to quantify postural control. There was a significant increase in the total excursion of the CoP between the pre-test and first post-test, indicating that perceived fatigue was related to a decrease in postural control as assessed by the BTrackS Balance Test. As predicted, postural control retuned to the pre-test level after the first post-test window, suggesting that effect of fatigue the BTrackS Balance Test lasts less than 9-minutes. This observation supports previous findings by Benedict, Hinshaw, Byron-Fields, Baweja and Goble [34], who showed that the BTrackS Balance Test performance returned to pre-fatigue levels within 5-minutes after the same fatigue protocol used in the current study. Our study design only allowed for nine-minute windows in the post-test session due to the duration required to complete the BTrackS Balance Test, AccWalker, RPE, and NASA-TLX assessments. Thus, our data supports previous work [34], but their study had a shorter time resolution to identify when the BTrackS Balance Test returned to pre-fatigue levels. A unique contribution of the current study is the inclusion of the NASA-TLX, as the previous work only included RPE as a perceived fatigue assessment [34]. The observation that the NASA-TLX remained elevated in the 9-18 minute and 18-27-minute windows, during which time the BTrackS Balance Test returned to pre-fatigue levels, suggests that perceived workload and static postural control on a force plate may fluctuate independently. Perhaps the most interesting finding was no significant changes in AccWalker postural control measures. It is important to note the AccWalker uses stride time SD and peak flexion SD as the metrics for postural control, whereas the BTrackS Balance Test which uses center of pressure movement. Thus, there is a fundamental difference in the movement characteristics derived from each test. The tests also differ in task difficulty, where the BTrackS Balance Test is a static postural control test and AccWalker is a dynamic postural control task. Both tests have been shown to be valid/reliable [30,31,35], resistant to practice effects [35,40], and shown to have clinical utility in identifying balance changes after head trauma [14,41]. While performance on the BTrackS Balance Test has been shown to return to pre-fatigue levels within 5-minutes [34], this presents a challenge in athletic populations who may need a more immediate assessment of postural control after physical exertion. An objective test of postural control that has appropriate clinical sensitivity and is not affected by perceived fatigue would be desirable for clinicians who work with athletic populations. The findings of the current study suggest AccWalker fits within those constraints, as the two variables previously shown to change after head trauma (stride time SD and thigh flexion SD) [36] did not change after the fatiguing protocol used in this study. This is a desirable outcome, suggesting that a change in AccWalker performance is likely due to neurosensory mechanisms rather than perceived fatigue or workload.The second hypothesis explored whether the magnitude of the increased in perceived fatigue scaled with the change in postural control. The findings suggest that this is not the case, except for thigh flexion SD in the head shake condition with the NASA-TLX. The head shake condition has been anecdotally reported as more difficult than the eyes closed condition in the current and previous studies, which may account for the positive association between these two metrics. This observation highlights the role of perceived workload in physical tasks, which may help increase the sensitivity of identifying neuromotor dysfunction in some clinical populations. The positive association between AccWalker stride time SD in the eyes open and head shake conditions suggest that both metrics are similarly affected by perceived fatigue, albeit rather minimally due to the observations from hypothesis one. A limitation of this study was that we did not include a measure of perceived fatigue or workload immediately after the fatigue protocol. This would have allowed for a measure of perceived fatigue and workload at the time subject finished the fatigue portion rather than after the first set of postural control measures—around 9 minutes post-fatigue. Given the first mobile balance test (BTrackS or AccWalker) occurred immediately after fatigue, this may have provided a more representative amount of perceived exertion or workload for the first post-test. Another limitation is some subjects mentioned verbally to the lead investigator they felt the head-shake task became easier with each administration. This supports the previous observation that a small learning effect is expected between the first and second administration of the head shake condition [35]. Thus, while the fatigue protocol was expected to increase the SD of the AccWalker variables, the fact that the first post-test was the second administration of the test suggest that the expected increase in SD may have been negated by a decrease in SD from the learning effect. The learning effect was minimized by providing a practice trial before the pre-test. Nevertheless, it may have reduced AccWalker’s ability to identify fatigue effects. This observation is tempered by the lack of change in the eyes closed condition after fatigue, which was not shown to have a learning effect from the first to second administration [35]. Thus, it is likely that any learning effects played a rather minimal factor in the performance on the AccWalker test. Lastly, the post-test window duration that was required to complete the two postural control tests and the two perceived fatigue tests was larger than previous research who explored similar questions. Specifically Fox, Mihalik, Blackburn, Battaglini and Guskiewicz [37] used 3-5 min windows and Benedict, Hinshaw, Byron-Fields, Baweja and Goble [34] used 5-minute windows. The 9-minute windows used in this study reduced our ability to precisely identify when perceived fatigue began to have a lesser effect on postural control.
5. Conclusions
- The BTrackS Balance Test and the AccWalker dynamic balance assessment provide clinicians a way to objectively measure postural control, which builds upon previously developed subjective tests used in this context. The data show that perceived fatigue and workload acutely affect the BTrackS Balance Test, but not AccWalker. It may be that the AccWalker is not sensitive enough to changes in postural control to detect the deficits that occur. These findings may help clinicians working with civilian, military, and athletic communities better select the test most appropriate for them based on their desired assessment characteristics (static or dynamic balance) and administration time relative to physical exertion.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML