-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2020; 10(3): 57-61
doi:10.5923/j.sports.20201003.01

COVID-19: Sedentary Isolation – A Bad Combination
Trish Sevene1, Kent J. Adams1, Mike Climstein2, 3, Joseph M. Berning4, Carole Carson5, Chad Harris6, Joe Walsh7, Mark DeBeliso8
1California State University Monterey Bay, Seaside, California, USA
2Southern Cross University, Gold Coast, AUS
3The University of Sydney, Sydney, AUS
4New Mexico State University, Las Cruces, New Mexico, USA
5Advanced Care Hospital of Southern New Mexico, Las Cruces, New Mexico, USA
6Metropolitan State University of Denver, Denver, Colorado, USA
7Sport Science Institute, www.sportscienceinstitute.com
8Department of Kinesiology and Outdoor Recreation, Southern Utah University, Cedar City, USA
Correspondence to: Mark DeBeliso, Department of Kinesiology and Outdoor Recreation, Southern Utah University, Cedar City, USA.
| Email: |  |
Copyright © 2020 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The COVID-19 virus outbreak was declared a pandemic by the World Health Organization (WHO) as of March 2020. Hand washing and a 2-meter social distancing became the norm worldwide as front-line mitigation interventions. Subsequently many States in the U.S. and countries worldwide adopted a more aggressive mitigation strategy known as “shelter-in-place”. The “shelter-in-place” intervention also known as “stay at home” requires individuals to stay at home except trips for essential needs and to work remotely for businesses considered as non-essential. However, there are concerns regarding the “stay at home” isolation effects on an already sedentary (inactive) world population. The authors provide a pointed summary of scientific literature identifying the potential ramifications of large sectors of the population becoming both isolated and sedentary. Likewise, the authors suggest straightforward strategies for physical activity that could help mitigate the negative ramifications of isolation and sedentary behavior. The authors consider their remarks as promoting the value of physical activity and not as professional medical advice. If you are feeling isolated or alone, seek the council of your health care provider.
Keywords: Pandemic, Sedentary, Physical activity, Corona, Mitigation
Cite this paper: Trish Sevene, Kent J. Adams, Mike Climstein, Joseph M. Berning, Carole Carson, Chad Harris, Joe Walsh, Mark DeBeliso, COVID-19: Sedentary Isolation – A Bad Combination, International Journal of Sports Science, Vol. 10 No. 3, 2020, pp. 57-61. doi: 10.5923/j.sports.20201003.01.
Article Outline
1. Introduction
- A pandemic due to the outbreak of the COVID-19 virus was declared by the World Health Organization (WHO) as of March 2020 [1]. The mortality rate due to the COVID-19 virus differs by country but was reported by the WHO on 3rd March 2020 to be 3.4% globally [2]. This figure has met with a high degree of scepticism both in terms of its accuracy and interpretation [3]. In an effort to mitigate the transmission of the COVID-19 virus the Centers for Disease Control and Prevention (CDC) have recommended hand washing (soap and water ≥ 20 seconds or hand sanitizer with ≥ 60% alcohol) and social distancing (≈2 meters) [4]. Others have summarized further mitigation strategies [3] and some have adopted aggressive self-isolation measures. Many states in the United States and many countries worldwide have expanded the recommendation of social distancing to a “shelter-in-place” or “stay at home” order [5].
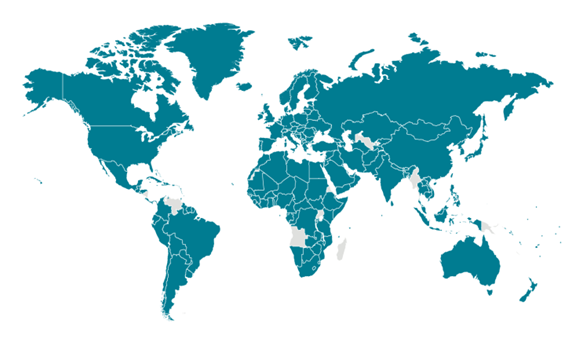 | Figure 1. Global Map as of April 20, 2020. Source: Centers for Disease Control and Prevention [3]. Locations with confirmed COVID-19 cases are colored green |
2. Sedentary Isolation
- The “stay at home” order requires all non-essential businesses to close and employees to work remotely while students continue their education via online platforms [5]. For many the “stay at home” order is essentially a relegation to an environment of social isolation. Social isolation however has been widely recognized to have a profound impact on an individual’s health and ultimately longevity [9]. For example, mental health including anxiety [10], depression [11], schizophrenia [12] and dementia and Alzheimer’s disease [13] has been shown to be strongly related to social isolation. Additionally, social isolation has also been shown to increase the risk of major chronic diseases such as blood pressure control/hypertension, obesity and a weakened immune system [14,15]. A large-scale study of 32,000 individuals found that social isolation significantly increased the risk of cardiovascular disease by 90% and the risk of non-fatal stroke was doubled [16]. Furthermore, Kawachi and colleagues [16] reported those individuals socially isolated had a 50 percent increased risk for mortality. There is also evidence that social isolation in early life predicts future physical inactivity, it is therefore prudent to initiate physical activity/exercise strategies for adolescents and young adults, so as to minimize the development of long-term behaviors that will be detrimental to health [17].Sedentary behavior is also widely recognized as a major contributor to global health problems and premature mortality [6,8]. Inactivity is related to a host of diseases (e.g., type 2 diabetes mellitus, obesity, hypertension, heart disease, stroke, depression, sarcopenia) and events (e.g., falls, musculoskeletal injuries), including eight types of cancer [8] and has associated economic cost of well over $100 billion in the U.S. alone [8]. In contrast, physical activity has many benefits (both acute and chronic) on physical and mental health (e.g., reduced stress and anxiety, improved sleep, decreased pain, reduced postpartum depression, improved musculoskeletal and cardiovascular fitness, improved blood pressure, increase ability to perform activities of daily living, better management of chronic disease symptoms, improved insulin sensitivity, reduced falls and fractures, and improved quality of life) [6,8,18]. A further advantage of physical activity is the beneficial effects on the immune system [19]. The immune system has been shown to be responsive to and stimulated by physical activity, by both acute and repeated bouts of exercise. The benefits derived from an acute bout of exercise are dependent upon the intensity and duration of the bout. The immune system’s adaptive response to exercise has elevated importance for those individuals who are older and those with chronic disease.For example, a threshold of 60 percent of heart rate range ((220 – age in years) * .6 intensity)) for a short duration of up to 45 minutes has been shown to exhibit significant benefits to immunity [20]. Enhanced immunosurveillance has been shown in exercise bouts of less than 60 minutes however it requires a higher intensity of aerobic exercise, specifically moderate to high intensity. The mechanism is that the acute exercise stimulates the immune system cells and components between the lymphoid tissues and blood compartment. Although this benefit is transient in nature, a cumulative effect is seen when the exercise bouts are continued over time and results in improved immunosurveillance [20]. Unfortunately, the overlap between diseases related to social isolation and those related to sedentary behavior is dangerously clear. This bad combination increases mental and physical health risk, both acutely and chronically.
3. Physical Activity Recommendations
- Physical activity recommendations are well-established [6,8]. In general, for adults they are as follows:• move more, sit less; small bouts have impact throughout the day• accumulate at least 150 minutes per week of moderate intensity activity (e.g., anything that increases your heart rate; walking briskly; dancing; general yard work) or 75 minutes per week of vigorous intensity activity (e.g., jogging; energetic dancing; heavy yard work), or a combination of both• perform muscle strengthening activities that involve all major muscle groups 2-3 days per week (e.g., use an implement that creates resistance to movement through a full range of motion)Please see links [6,8] for specific guideline modifications for pre-school aged children, children and adolescents, older adults, those pregnant or in postpartum period, and adults with chronic health conditions and adults with disabilities.
4. Movement Matters, Now What?
- COVID-19 restrictions have resulted in the mandatory widespread closure in health and fitness facilities; thus, individuals are limited to home activity/exercise programs to maintain and improve mental health and physical fitness. That said, the guidelines provided by HHS [8] and WHO [6] can be met in isolation while abiding by the stay at home order. First a sedentary isolated individual should attempt to “move more, sit less”. Recent advancements in movement science have shown that short bouts (i.e., bouts of any length) of activity provide health benefits [8] and that prolonged sitting is unhealthy [8,21,22]. This is a critical point. The benefits going from being sedentary to active (in any duration) are cumulative, with each bout contributing to the overall positive effect [8]. Certainly, if a sedentary isolated individual can complete more physical activity, that is preferable. But it should be remembered, research supports the impact of short bouts of physical activity accumulating over time. With regard to this, it is inadvisable to sit in one place too long. For example, a sedentary isolated individual could do sit-to-stands or push-ups during TV commercials. They could take a break from reading or working and play with children or pets. They can turn off the Zoom video and “move” while listening to their meeting. In the event of a social or work call, they can get up and “walk and talk”; bottom line, they should get up and move. Small bouts of activity are beneficial to health.Second, in order to accumulate moderate intensity activity, a sedentary isolated individual should get on their feet; step in place or better yet, walk. Given the social distancing rules in effect, walking is an allowable, low cost, effective mode of physical activity which can help alleviate the detrimental effects, both mental and physiological, of social isolation. Hanson and Jones [23] completed a systematic review and meta-analysis that included 42 studies and over 1,800 participants. They reported that walking resulted in significant reductions in resting blood pressure (systolic and diastolic), resting heart rate, decreased body fat, and total cholesterol. Participants also reported significantly improved physical functioning and a reduction in depression scores. None of the studies reported any adverse effects associated with the walking. Walking in one’s neighborhood has been promoted by communities during stay at home orders. It is important that appropriate measures are undertaken to protect from disease exposure if walking in public. As an alternative, yards, rooms, and stairs are examples of places one can accumulate physical activity. The great outdoors is still open; if possible and safe to do so, a sedentary isolated individual should get out and enjoy it.For muscle strengthening activities, a sedentary isolated individual should think about bodyweight exercises first (e.g., push-ups, body weight squats, lunges); trying to stress each major muscle group (e.g., legs, chest, back, shoulders, arms) for 10-15 repetitions. If this is too easy, they can try adding resistance with various implements in their house (e.g., milk/water jugs; dog/cat food bags; cat litter). Wearing backpacks containing filled water bottles or tinned food, can provide additional resistance for body weight exercises such as squats and lunges.One may ask, can home exercise be effective in the prevention of, or at least slow the rate of decline of common chronic diseases? Uchida and colleagues [24] recently investigated the efficacy of an unsupervised resistance training program (using Therabands, shoulder abduction and shoulder flexion) and fast walking (3,000 steps/d) in older adults. They found that after six months, participants increased their upper extremity muscle strength and total exercise time. This simple exercise regime conformed to the WHO recommendations for dose (i.e., time) of physical activity/exercise and would be economical and easy to adopt for most individuals. Also, Cornwell and Waite [25] suggest that socialization with people who exhibit healthy behaviors may reinforce such behaviors, promote health-related information, better nutrition and increased physical activity/exercise. While one is physically distant when staying at home, if available having a workout buddy on a digital platform (e.g., Zoom) helps provide meaningful social contact and motivation for physical activity. Encourage family members staying at home to be physically active with you (e.g., have a dance party).And, if you have not been physically active before, it is a great time to start. Time is often the number one reason someone gives for not being active. So, during isolation, take advantage of the extra time in your day, get active, and create new health habits.As always, use common sense in your activity intensity and choice. Start low, go slow. Progress gradually. Realize the risks of inactivity outweigh the risks of being physical active. [26] If you have chronic conditions or symptoms, consult with your health care professional for guidelines on appropriate physical activities. Consider a telemedicine check-in with your health care professional if available to you.
5. Connections to the Past
- One may ask about what we learned from past pandemics in relation to sedentary isolation. Conditions were different during Pandemics of the past [27,28]. For example, the 1918 Spanish Influenza Pandemic happened during the First World War [28]. Critical cases of the flu may have been impacted by factors such as military service, sanitation, insects, overcrowding, and weather [28]. But comorbidities associated with inactivity were not considered as sedentary lifestyles were relatively rare. At the time, high levels of obligatory physical activity were the norm. Additionally, inactivity during isolation would have been difficult. Necessities of all kinds were not delivered or available via a drive thru. Therefore, conditions related to both acute and chronic inactivity are unique to modern outbreaks. In essence, two pandemics are colliding with compounding effect.But, like past pandemics, COVID-19 is teaching us valuable lessons that we need to heed for a healthier response to the next pandemic [29]. For example, like obesity being a recognized risk factor for severe complications and death caused by influenza A/pdmH1N1 [30], we are learning that comorbidities like diabetes, obesity, hypertension, sarcopenia, etc. matter in terms of an individual’s risk to succumb to COVID-19 or related complications [7]. Many of these co-morbidities are strongly associated with a sedentary lifestyle and can be combatted by physical activity [6,8,31]. To quote Sun-Tzu, “in the midst of chaos, there is also opportunity.” Inactivity has been labeled a pandemic by many [31], and the associated death toll is estimated in the millions world-wide [31]. We must take the power of physical activity seriously as a tool to increase resilience and fight disease. As we have gained insight from past pandemics, learning from the current co-pandemic of COVID-19 and physical inactivity will increase preparedness for the next public health crisis we face [29]. Sedentary isolation is a deadly combination.
6. Summary
- Sedentary isolation is a bad combination, harming both physical and mental health. While the stay at home order is in place, embrace physical activity and attempt to meet the science-based physical activity guidelines put forth by the HHS and WHO. New habits may be formed, leading to positive lifestyle changes and ultimately improved health and fitness. While physical isolation and social distancing are necessary, sedentary behavior is not. Get up and move! It does a body and mind good!
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML