-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2017; 7(2): 73-80
doi:10.5923/j.sports.20170702.08

Cardiovascular Evaluation of Adults Aged 40 Years and above Involved in Leisure-Time Physical Activity: Experience of Yaoundé-Cameroon
Ngongang Ouankou Christian 1, Imele Metenou Hermann Eugene 2, Menanga Alain Patrick 2, Hamadou 3, Ouankou Mérimée Débozard 4, Ama Moor Vicky Jocelyne 5, Wawo Yonta Edvine 2, Ngu Blackett Kathleen 2, Kingue Samuel 2
1Medicine and Specialties Unit, University Hospital Center (UHC), Yaoundé, Cameroon
2Department of Internal Medicine and Specialties, Faculty of Medicine and Biomedical Sciences (FMBS), Yaoundé, Cameroon
3Medical Services, Fire Service, Yaoundé, Cameroon
4Cardiological and Médical Center, Yaoundé, Cameroon
5Biochemistry Laboratory, University Hospital Center (UHC), Yaoundé, Cameroon
Correspondence to: Ngongang Ouankou Christian , Medicine and Specialties Unit, University Hospital Center (UHC), Yaoundé, Cameroon.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Objective: The objective of this study was to describe abnormalities found at cardiovascular evaluation of a group of adults aged at least 40 years, involved in leisure-time physical activity. Methodology: This was a cross-sectional population-based study conducted in Yaoundé-Cameroon. For each individual, clinical examination, fasting blood glucose, lipid profile and 12-lead resting electrocardiogram (ECG) were done. Results: Study population size was 486. Men represented 53% of our study population. The average age was 49.1 ± 7.1 years. Females were as aged as males. 13.1% were symptomatic at effort. Two subjects had a cardiac murmur and one a gallop rhythm. 6.6% were smokers, 1.8% had a family history of premature sudden death, 53.1% were obese and 31.2% overweight, 24.5% had high blood pressure, 5.3% diabetes mellitus and 27.1% dyslipidemia. 6.4% of subjects had a moderate to very high absolute cardiovascular risk (ACVR). Women’s ACVR was statistically identical to men’s. Those presenting symptoms during effort had an ACVR superior to that of non-symptomatic subjects. 57.5% of ECGs were abnormal. 28.6% of ECGs presented abnormalities suggesting risk cardiopathies (group 2 abnormalities). The proportions of such ECGs were higher for the symptomatic subjects and those above 50 years, and there was no gender difference. Conclusion: The cardiovascular evaluation of the leisure-time sportsmen and sportswomen aged at least 40 years discloses many abnormalities suggestive of a significant risk of exertion-related acute cardiovascular events. Women seem to be as much at risk as men. Symptomatic individuals and those aged at least 50 years appear to be more at risk.
Keywords: Leisure-time physical activity, Adults aged 40 years and above, Acute cardiovascular events, Sudden death, Cardiovascular evaluation
Cite this paper: Ngongang Ouankou Christian , Imele Metenou Hermann Eugene , Menanga Alain Patrick , Hamadou , Ouankou Mérimée Débozard , Ama Moor Vicky Jocelyne , Wawo Yonta Edvine , Ngu Blackett Kathleen , Kingue Samuel , Cardiovascular Evaluation of Adults Aged 40 Years and above Involved in Leisure-Time Physical Activity: Experience of Yaoundé-Cameroon, International Journal of Sports Science, Vol. 7 No. 2, 2017, pp. 73-80. doi: 10.5923/j.sports.20170702.08.
Article Outline
1. Introduction
- The regular practice of physical activity of moderate to vigorous intensity is highly recommended to prevent acute cardiovascular events (ACE) [1-4]. However, it has been shown that moderate to vigorous muscular exertion (VME) increases the risk of ACE (myocardial infarction, silent myocardial ischemia), including sudden cardiac death, in individuals harbouring cardiovascular disease [5, 6]. The athlete (between 12 and 35 years) presents a risk of sudden death (SD) 2.5 times higher when compared to his sedentary homologue of the same age [7]. SD incidence is higher in sportsmen after they reach 40 years, especially if previously sedentary or practicing sports after a long interruption [8]. The causes of non-traumatic SD in athlete are cardiovascular in over 90% of cases [9]. Before 35 years, the problem is usually due to a congenital cardiac abnormality, usually unknown, such as hypertrophic cardiomyopathy [10]. After 35 years, coronary disease (CD) is the leading cause of sports-related cardiovascular accidents (85% of ACEs), not only in highly trained senior athletes, but also in people not accustomed to making such efforts [11-15]. As such, it is of prime importance during check-up for sporting activity to detect CD in sportsmen aged 40 and over. Ideally, a complete screening comprising search of cardiovascular risk factors (CVRFs), clinical examination, resting-ECG, and tests enabling evaluation of the coronary reserve such as maximal exercise testing, will facilitate the disclosure of individuals at risk of coronary events during VME [16, 17]. This study was carried out to describe abnormalities found at clinical examination, in biology and resting-ECG in sportsmen and sportswomen aged 40 years and older. More specifically, it aimed to: determine CVRFs prevalences, evaluate the absolute cardiovascular risk (ACVR), describe the physical and electrocardiographic abnormalities and compare the differences among the groups.
2. Material and Methods
2.1. Study Population and Setting
- This was a cross-sectional population-based study conducted in Yaoundé-Cameroon. Approval was obtained from the ethical committee of the Faculty of Medicine and Biomedical Sciences (FMBS). The sites chosen were: Parcours vita, the environs of the Omnisport stadium and Biyem-Assi district; places highly frequented by recreational sportsmen aged at least 40 (mainly joggers, brisk walkers, aerobics practitioners). Included in the study was any adult of at least 40 years, practicing a minimum of one hour recreational sporting activity per week and having given written consent. Any person whose last meal was less than eight hours before the screening, or had consumed alcohol, tobacco or caffein less than three hours before recruitment, or having decided to withdraw from the study was systematically excluded.
2.2. Data Collection
- The screening was conducted by trained medical personnel using a pre-established questionnaire. Personal and family histories were taken. CVRFs, level of physical activity (PA) in the socio-professional life evaluated using the World Health Organization (WHO) criteria [18], any undertaking of a medical check-up prior to starting sports, and any symptomatology on exertion were assessed. The physical examination of the subject was performed. Anthropometric parameters were measured in accord with WHO STEPwise approach to surveillance (STEPS) procedure [19]. Blood pressure (BP) was measured following the Heart foundation protocol [20] with a validated digital BP monitor (Omron® HEM-712C). Fasting venous blood was collected for blood glucose and lipid profile. The samples were conserved in a cooler, and then carried to the biochemistry laboratory of the University Hospital Center (UHC). 12-lead resting ECG was done with a portable electrocardiograph CARDIO – M® Ver 5.04M, according to the American Heart Association (AHA) recommendations [21]. Biological tests on the blood samples were carried out in the UHC laboratory using enzymatic and colorimetric methods. The reagents employed were of Biolabo® brand. Optical densities were read with a spectrophotometer Mindray® BA-88A. HDL-cholestérol dosage was measured in the supernatant after precipitation of chylomicrons, LDL and VLDL by phosphotungstic acid and magnesium chloride. The LDL-cholesterol level was calculated by the mean of the Friedwald formula: LDL = total cholesterol (TC) – HDL – triglycerides (TG)/5 if TG level was less than 3,6 g/l. The ACVR was assessed using the WHO/ISH (International Society of Hypertension) risk prediction chart for the corresponding sub-region of the participant [22]. ECGs were interpreted using the AHA guidelines [23-27] by the college of physicians of the research team.
2.3. Definitions
- Hypertension was defined as BP ≥ 130/80 mmHg for participants with associated condition(s) or end organ damage, and for all others as BP ≥ 140/90 mmHg, or as the taking of BP-lowering medications over the last 15 consecutive days. Obesity was defined as a body mass index (BMI) ≥ 30 kg/m2 and/or a waist circumference (WC) ≥ 102 cm for men and ≥ 88 cm for women, and overweight as a BMI ≥ 25 kg/m2 and < 30 kg/m2 and/or WC ≥ 94 cm and <101.9 cm in males or ≥ 80 cm and < 87.9 cm in females. Respondents were classified as:- smokers if they consumed tobacco at the time of investigation or had stopped less than 3 years before; diabetic if they had a venous glycaemia ≥ 1.26 g/l, or if they were on hypoglycemic medications; and dyslipidemic if they had TC > 2.70 g/l, and/or LDL > 1.90 g/l, and/or TG > 1.50 g/l, and/or HDL level < 0.41 g/l, or if they were on lipid-lowering drugs. Premature SD was defined as SD before 55years for the father or brother, and before 65 years for the mother or sister (SD of the infant included).Electrocardiographic abnormalities were classified into two groups according to the European Society of Cardiology (ESC) [28]: group 1:-common and training-related ECG changes and group 2:-uncommon and training-unrelated ECG changes. Abnormal ECGs were classified into two types: type 1: - ECGs presenting only group 1 abnormalities and type 2:-ECG presenting at least one abnormality of group 2 with or without that of group 1.
2.4. Data Analysis
- Data analysis was done with SPSS (Statistical Package for the Social Sciences) version 19.0. The means were compared with the One-Way ANOVA test and the frequencies with the Pearson Khi-square and Fisher exact tests. A ‘p’ value < 0.05 was considered significant.
3. Results
3.1. Characteristics of the Study Population
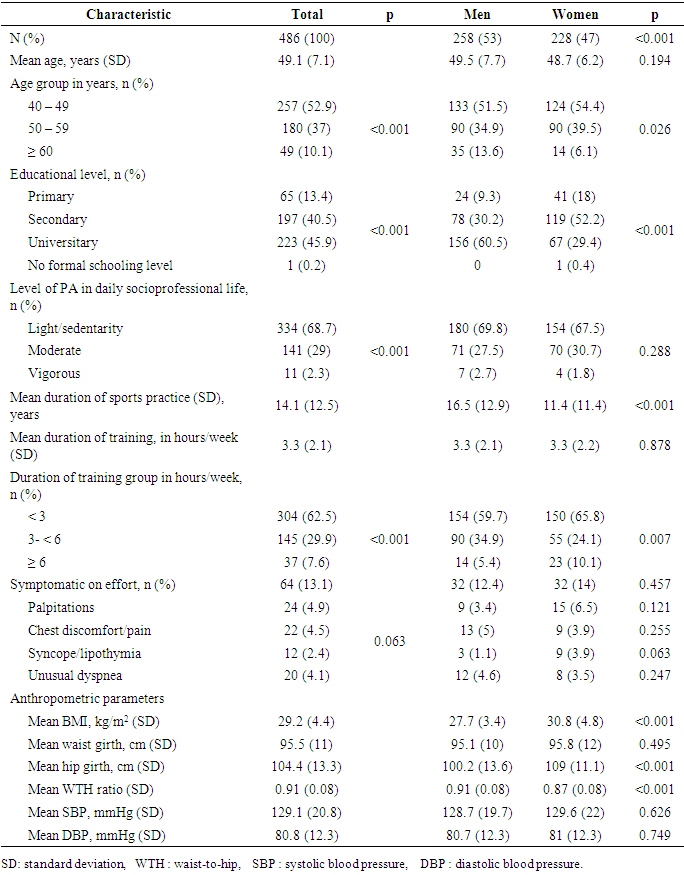
- The study population consisted of 486 subjects, 98.6% of them being Cameroonians. The mean age was 49.1± 7.1 years and males were predominant (53%). Only 2.8% had undertaken medical screening before beginning recreational PA. Main reasons advanced for undertaking leisure-time PA were: health keeping (62.1%), weight loss (18.1%), medical advice (11.3%) and entertainment (8.5%). Activities undertaken were: brisk walk (53.3%), jogging (25.8%), aerobics (11.6%), football (4.3%) and others (5%).Over 2/3(68.7%) of the participants were physically inactive in their daily socio-professional lives. This high frequency of sedentary individuals could be attributed to the fact that most of our subjects held administrative offices. Only 2.8% of the subjects had undergone medical screening prior to leisure-time PA undertakings. This figure shows the ignorance of dangers consequential upon sports of our study population. 13.1% of participants complained of symptoms during exertion (table 1). This percentage of symptomatic subjects (SS) aligns with that of Schmied and al, in 2012 on 210 Gabonese footballers: 9% SS on effort [29].
|
|
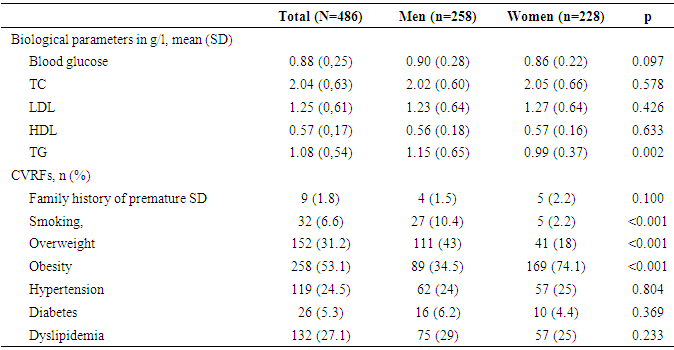
3.2. Cardiovascular Risk Factors (table 3)
- Tobacco consumptionAmong the study population, 6.6% were tobacco consumers with a higher prevalence in men (10.4% vs 2.2%, p < 0.001). Unpublished data from a national survey indicate that the overall prevalence of smoking is approximately 6.4% in Cameroon, with a higher frequency in males (8.2%) than in females (1.0%) [30]. Fezeu and al. in 2003 found a prevalence of tobacco consumption of 5.3% in Yaoundé with also a higher frequency in males (8%) than in females (3%) [31]. The difference between our findings can be due to the fact that they only consider as smokers people who used to smoke at the moment of the study, ex-smokers excluded.Premature SDA family history of premature SD was found in 1.8% of the study population. Overweight and obesity84.3% were either obese or overweight with higher frequency in women than men (92.1% vs 77.5%, p < 0.001). 53.1% were obese and women too were more affected than men (74.1% vs 34.5%, p< 0.001). Kamadjeu and al. in 2005 in their study conducted in 4 urban districts of Cameroon (Yaoundé, Douala, Garoua and Bamenda) found a lower prevalence than ours (40.1% of participants were either obese or overweight, 14.3% were obese); but they also found that women had a higher frequency of obesity than men (19.5% vs 6.5%, p< 0.001) [32]. This difference can be explained by the relatively young age of their subjects (mean age: 31.7 years) when compared to ours (mean age: 49.1 years), giving the fact that the prevalence of overweight and obesity increases greatly with age.High blood pressureHypertension was found in 24.5% of the subjects and there was no difference between males and females (24% vs 25%, p=0.804). Kengne and al. in 2004 in Douala found a prevalence of 20.8% and there was also no difference between genders in their study [33]. The gap between our frequencies could be explained by the relatively young age of their subjects (15 to *99 years) when compared to ours (40 years and older).Diabetes mellitusDiabetes mellitus was present in 5.3% of the participants. Sobngwi et al in 1998 in Yaoundé reported the same result (5.3%) [34]. Dyslipidemia27.1% of participants were suffering of dyslipidemia. To date there are no published studies on the national prevalence of dyslipidemia in Cameroon. In an unpublished study conducted by Keumami et al in 1998 in Garoua, 17.5% of subjects were dyslipidemic [35]. The young age, the preferential consumption of cotton oil and the low tobacco’s consumption of their subjects as compared to ours could explain this difference.There was no statistically significant difference between men and women for the prevalence of diabetes (p=0.369), neither that of dyslipidemia (p=0.233).
|
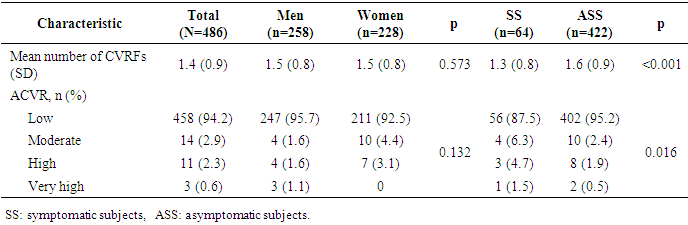
3.3. Cardiovascular Risk (table 4)
- The average number of CVRFs (all participants) was 1.5 ± 0.8 and women had as many CVRFs as men (p=0.573). 5.8% of the study population had a moderate to high and 0.6% a very high ACVR. The ACVR of females was identical to that of males (p= 0.132) (table 4). As was demonstrated across Europe in the EUROASPIRE III survey, modifiable lifestyle factors have aggravated and especially young women have taken up smoking habits and women have a higher increase in the prevalence of diabetes and hypertension than men, with its consequences for CVD incidence and prevalence [36]. Parallel with the rise in blood pressure and cholesterol levels after menopause there is almost a doubling in the prevalence of stroke among middle-aged women (35-54 years) [37].The ACVR of SS was greater than that of asymptomatic subjects (ASS) (p=0.016). SS thus have a higher risk of ACE when compared to ASS.
|
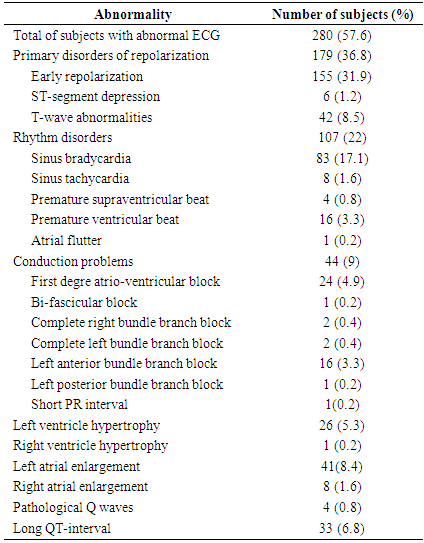
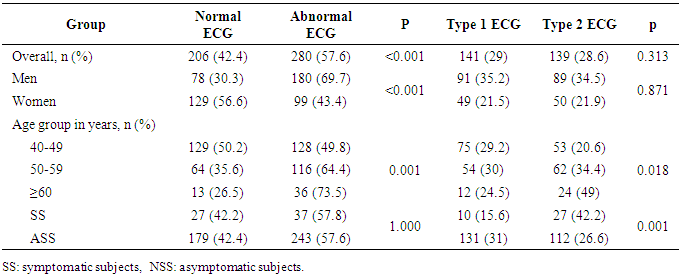
3.4. 12-Leads Resting Electrocardiogram
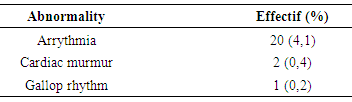
- Over half (57.5%) of the individuals had an abnormal ECG. Primary disorders of repolarization were the most frequent abnormalities (36.8%), followed by rhythm disorders (22%), conduction problems (9%), left atrial enlargement (8.4%), prolonged QT interval (6.8%), left ventricle hypertrophy (5.3%), right atrial enlargement (1.6%), pathological Q waves (0.8%) and right ventricle hypertrophy (0.2%). We found one case of atrial flutter, a Lown-Ganong-Levine syndrome, a bi-fascicular block, two complete left bundle branch blocks and six cases of significant ST-segment depressions (table 5).
|
|
4. Conclusions
- Cardiovascular assessment of recreational sportsmen and sportswomen aged 40 years and above in Yaoundé, reveals a non-negligible risk of exertion-related acute cardiovascular events. Women are as much concerned as men. Symptomatic individuals as well as people aged 50 years and above are those most concerned. More reliable studies must be carried out in order to determine the relevance of systematic cardiovascular screening for middle-aged/senior individuals, defined as older than 35 years, who are contemplating exercise or who are already engaged in nonprofessional competitive or recreational leisure sporting activity in Sub-Saharan Africa. The recommendations of the European Association for Cardiovascular Prevention and Rehabilitation (EACPR) concerning such a screening [38] are advisable.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML