-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2016; 6(4): 146-152
doi:10.5923/j.sports.20160604.03

Fall Determinants and Associated Factors in Older People
Wagner Fabrício L. Taets Silva1, Roberta L. Rica1, Bianca Ramalho1, Alexandre F. Machado1, Fabio Ceschini1, Francisco Luciano Pontes Júnior2, Andrey J. Serra3, Graciele M. Rodrigues1, Alexandre L. Evangelista4, Aylton Figueira Júnior1, Angelica C. Alonso1, Danilo S. Bocalini1
1Translational Physiology Laboratory, Post Graduate Program in Physical Education and Aging Science. São Judas Tadeu University (USJT), São Paulo, Brazil
2Post Graduate Program in Gerontology, Arts, Science and Humanities School (EACH), São Paulo University, São Paulo, Brazil
3Post Graduate Program in Biophotonic Applied in Healthy Sciences and Rehabilitation Science, Nove de Julho University (UNINOVE), São Paulo, Brazil
4Departarment of Physical Education. Nove de Julho University (UNINOVE), São Paulo, Brazil
Correspondence to: Danilo S. Bocalini, Translational Physiology Laboratory, Post Graduate Program in Physical Education and Aging Science. São Judas Tadeu University (USJT), São Paulo, Brazil.
| Email: |  |
Copyright © 2016 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

With aging, the body goes through a natural process characterized by functional and structural changes, which may be accompanied by physical and mental health problems caused often by chronic illnesses that make the elderly frail and more likely to suffer falls. Objective: to identify through literature review the main intrinsic and extrinsic factors associated with falls in the elderly. Methods: a literature search was performed from the databases SciELO, MedLine, Bireme and books. Results: The studies revealed the importance of identification of intrinsic and extrinsic factors in episodes of falls in the elderly. In most studies analysed the major emphasis is given to the root causes as the main causes of these events; however you need to consider environmental factors. Conclusion: during the aging process the older people becomes more prone to suffer falls where these are caused by a multifactorial process.
Keywords: Quality of Life, Falls, Older People, Intrinsic and Extrinsic Factors
Cite this paper: Wagner Fabrício L. Taets Silva, Roberta L. Rica, Bianca Ramalho, Alexandre F. Machado, Fabio Ceschini, Francisco Luciano Pontes Júnior, Andrey J. Serra, Graciele M. Rodrigues, Alexandre L. Evangelista, Aylton Figueira Júnior, Angelica C. Alonso, Danilo S. Bocalini, Fall Determinants and Associated Factors in Older People, International Journal of Sports Science, Vol. 6 No. 4, 2016, pp. 146-152. doi: 10.5923/j.sports.20160604.03.
Article Outline
1. Introduction
- Increased life expectancy is one of the most important achievements of mankind in the twenty-first century, and strongly associated with technological, economic and social advances [1]. This is a worldwide phenomenon, and in Brazil, current figures show that for every two people aged 15 years, there is a person over 60 years [2]. On the other hand, of every 100 people, 20 are elderly with physical or mental limitations, which brings great concern about the quality of life of elderly Brazilians [2]. In this context, increased life expectancy results in new challenges for society, especially regarding physical and mental aspects, because of its association with improved quality of life in this age group [3]. Information on morbidity and functional limitations in the elderly are usually associated with falls and the presence of other chronic diseases, factors promoting change in the perception of quality of life [3]. According to Forsman, Nordmyr & Wahlbeck [4], neurofunctional changes in the aging process are related to increased number of falls, which in turn contributes with increased physical inactivity and physiological diseases [5]. A recent survey of the Brazilian Institute of Geography and Statistics [2] showed that for every 100 thousand inhabitants aged over 60 years, 110.3 die from problems associated with falls.The occurrence of falls is related to intrinsic (of the subject) and/or extrinsic (environmental) factors. The intrinsic factors stand out for influencing most falls in some way, and the main described in the literature are reduction of strength and muscle power due to sarcopenia, changes in gait and postural control, visual, functional and cognitive impairment, and natural aging changes [6] Falls and fractures result in losses in the quality of life of seniors and worsening of physical impairment such as reduced ability to walk, weight gain and loss of cardiorespiratory function [7] Furthermore, physiological changes such as isolation and depression are factors that increase the risk of institutionalization [8-10].The epidemiological characteristics of falls in the elderly demonstrate a history of falls with recurrences in over 30% of seniors over 65 years [11], and after 75 years, falls affect 45% of the elderly [6] Of every ten falls, at least one results in serious consequences such as fractures, bruises and trauma that can cause dependence and even death [12, 7]. In 50% of falls, external factors are among the most important associated causes. On the other hand, in 70% of falls, the interaction of multiple factors would explain this condition, such as health status, low mobility, sedentary lifestyle and low physical fitness [13].The intrinsic causes that lead elders to an episode of fall may be related to the physiological changes of aging, such as disturbances in the vestibular system, vision, hearing, musculoskeletal disturbances, cell proliferation, among others that can result in changes of balance and gait [13]. When associated with pre-existing diseases including cardiovascular, neurological, endocrine, musculoskeletal and sensory disturbances, there may be aggravation of the decline in health [14]. The effects caused by multiple drugs such as anxiolytics, antidepressants, anticonvulsants and antihypertensives also must be considered [15]. Few falls are caused by a single risk factor, and most result from an association of intrinsic and extrinsic risk factors [11, 16]. Extrinsic causes are directly related to architectural barriers, ergonomics and social factors, and these should be especially considered given their significant influence on the falls of seniors. Such influence is more significant because of its relation with the decline in most physiological functions with aging, making the elderly more fragile and less attentive to conditions imposed by the environment itself [17-19].In addition to the aforementioned factors, numerous studies have shown a positive association between the occurrence of falls and inactivity, emphasizing a higher percentage of falls among sedentary seniors with poor self-perception of health and higher use of continuous prescription drugs [9, 20].From these issues, the aim of this review was to identify the intrinsic and extrinsic key factors leading the elderly to suffer a fall.
2. Methodology
- The most relevant original scientific studies were from 1987 to 2015, analyzed in this review, at databases SciELO, MedLine and Bireme combining the following keywords: quality of life, fall, elderly, intrinsic/extrinsic factors. Studies investigating all keywords mentioned with different were considered inclusion criteria.
3. Literature Review
- Causal factors for falls are widely studied to help prevent their occurrence or minimize their deleterious effects that negatively affect the life of the elderly [7]. The proper reception of information by the body through its mechanisms of capture by sensory, cognitive and musculoskeletal components that act integrated can ensure an effective response to the daily demands. However, the different changes accumulated with aging, along with the environment in which the elderly is inserted may predispose the person to falls [21].The relationship between intrinsic and extrinsic factors as causes of falls is confirmed by several authors. However, intrinsic causes must be prioritized because during aging there is a natural and progressive process of functional and structural modifications in the body [8].
3.1. Intrinsic Factors
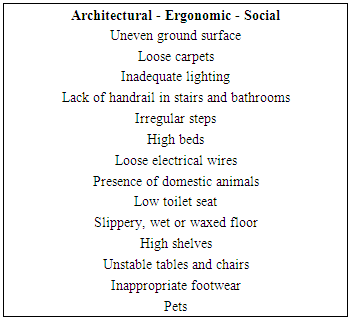
- The loss of proliferative capacity of the cells, reduced muscle mass and bone mineral density, decline in the nervous, musculoskeletal, vestibular and visual systems, loss of painful tactile sensitivity, memory loss, depression and anxiety are determining factors for the appearance of signs of weakness in the elderly, and consequently make them more vulnerable to falls [22, 15]. According to Buckman et al. [23], the most significant intrinsic factors related to falls among the elderly are a prior history of falls, age, female gender, medications, medical conditions, gait disorders, posture maintenance and consequently, reduction of balance, sedentary lifestyle, psychological state, nutritional deficiency, cognitive impairment, visual impairment, and orthopedic diseases.Investigating the intrinsic factors associated with falls in the elderly, there is a significant decline in muscular strength and endurance between the fifth and sixth decade of life [24-26]. This is due to a delay in conduction velocity of motor nerve fibers, leading to decreased muscle power [27]. The maintenance of postural control requires the integration of sensory, nervous and musculoskeletal systems in order that the body center of mass remains in a support base within the limits of stability in a way that the center of gravity moves without changing the support base. When these systems are dysfunctional, the likelihood of falling increases [25]. The muscle weakness establishes a two-way relationship with its functional losses, dependence on caregivers, physical inactivity and acceleration of physiological aging [9].Because of lower social activity, older people move less, which contributes to muscle mass loss natural of aging. Furthermore, less movement also collaborates to the regress of neural adaptations made throughout life, making this population recruit more muscle mass to produce the same power than a young adult during everyday activities. This extra percentage recruited requires greater blood supply, glucose transport and increased mitochondrial density, functions that are reduced in the elderly, and generate greater fatigue and an inactivity cycle [10, 13].The flexibility of lower limbs can be an important factor in determining the risk of falls, especially given its relationship with gait pattern modifications [26]. Unfortunately, there are few studies identifying flexibility as an epidemiological exposure variable for falls in the elderly or presenting this physical quality as a risk factor for falls [27].Furthermore, flexibility tends to decline sharply with age and is associated with falls in the elderly, particularly in terms of mobility loss of hip, knees, ankles and spine, causing changes in gait pattern and difficulties in performing everyday tasks such as using public transportation, moving through ground unevenness (sidewalks, stairs, etc.) or walking [28].
 | Figure 1. Intrinsic factors for fall in older people |
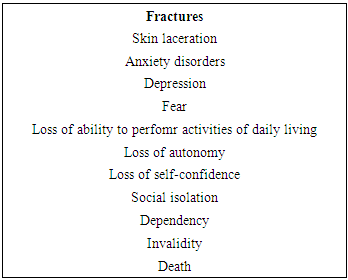
3.2. Extrinsic Factors
- External causes can be distributed into behavioral, socioeconomic and environmental factors. Behavioral factors are potentially modifiable, including excessive alcohol consumption, use of inappropriate shoes, physical inactivity and polypharmacy [34]. By understanding the use of polypharmacy of seniors, it has been proven that some drugs decrease alertness and can cause postural hypotension, a favourable condition for falls [23]. The most influencing socioeconomic factors are low income, low level of life, limited access to health and social services, and lack of social support [34].The magnitude of the influence of environmental factors on the elderly’s risk of falls remains quite controversial. Baltas et al. [35] indicates that 30% to 50% of falls are caused by environmental interference factors. According to Buckman et al. [23], many environmental factors may contribute to falls, among which the following stand out: uneven ground, poor lighting, slippery surfaces, carpets without fixation, stairs, obstacles, lack of handrail support in hallways and bathrooms, inadequate positioning of to the person’s height, inadequate clothes and shoes, public road with irregularities, and inappropriate orthotics.Buckman et al. [23], many environmental factors may contribute to falls, among which the following stand out: uneven ground, poor lighting, slippery surfaces, carpets without fixation, stairs, obstacles, lack of handrail support in hallways and bathrooms, inadequate positioning of shelves in relation to the person’s height, inadequate clothes and shoes, public road with irregularities, and inappropriate orthotics.Among the main extrinsic causes leading to falls of seniors, is the inadequate spatial organization in long-stay institutions (LSI) [9]. According to studies, the environmental conditions of some LSI are not favorable for the maintenance of seniors’ postural balance, such as the uneven ground surface, loose carpets, inadequate lighting, lack of handrails on stairs, uneven steps, high beds, lack of armrest on chairs, loose electrical wires, presence of pets in the house, lack of grab bars in bathrooms, low toilet seat, and slippery floor [36].Environmental factors as determinants of risk of falls in the elderly should also be considered within their home. In addition to environmental conditions found in LSI, there are waxed and wet floors, very high shelves, unstable tables and chairs, and inappropriate footwear, as well as architectural barriers such as unsafe stairs, uneven sidewalks, very high bus steps, among others [37].Buckman et al. [23, p. 6] points out that ‘the most inactive and the most active people are those at increased risk of falling, possibly due to the weakness of the first and the degree of risk exposure of the others’. Both intrinsic and extrinsic factors cause falls, however, regardless of the cause, consequences will be very limiting, and in some cases even fatal. In addition to these potential problems and risk of mortality, the reduction of activities of daily living, decline in health and increased risk of institutionalization generate physical and psychological damage and high costs with caregivers, especially because of increased hospitalizations [17].Given the above, we emphasize that aging is a natural and multifactorial process, and in most cases it can be accompanied by diseases. Hence, the need for an in-depth study about the psychological and physical changes during the aging process, and its relationship with internal and external causes that might favor the seniors’ functional decline, making them more prone to suffer falls [38].
|
3.3. Risks of Fall and Physical Activity
- One of the strategies to minimize losses resulting from the aging process is related to physical activity. Studies show a lower incidence of falls, osteoporosis and other chronic diseases among the elderly who practiced physical activity during adolescence and adulthood (Tuunainen et al., 2013). In their study, Cebolla et al. [6] found reduced muscle strength as the closest factor related to falls. They observed that the elderly with at least an episode of fall in the previous 12 months showed lower strength indices in lower limbs, especially in knee flexor muscles. The benefits of physical activity practice have been increasingly studied within this context, especially the practices related to balance, strength, coordination and speed of movement, contributing to the prevention of falls and greater safety for the elderly [39]. The participation of seniors in mild exercise programs shows significant reduction in the number of falls when compared to sedentary elderly [27, 40].Studies linking exercise, physical activity and risk of falls demonstrate that both inactive and active individuals are at high risk of falling [35]. The study of Karlsson, Nordqvist & Karlsson [41] followed 5,995 individuals for 4.5 years and observed a higher risk of falls in physically active individuals. Probably this is due to the greater exposure to risk factors such as uneven ground, and more complex and unstable movements. However, individuals with low muscle strength, especially in the lower limbs, had higher risk of falls in everyday situations.Recent studies [35, 39, 24] found an inverse relationship between increased physical activity and risk factors for falls. However, there is no concrete evidence of programs with exercise intervention in individuals with severe visual impairment or mobility problems resultant from stroke, Parkinson’s disease and fractures [42-43].
|
4. Conclusions
- The data obtained in this review led to the conclusion that during senility the elderly become more prone to suffer falls related to intrinsic and extrinsic factors. In most studies, intrinsic causes were emphasized as the main responsible for falls, but they also revealed the importance of extrinsic causes in these events. The study of falls is necessary to think of multifactorial intervention programs that can help to minimize the risk factors presented in a dynamic and complex way in the daily life of seniors. Interventions involve the elaboration of operation strategies with people and the environment, suggesting the need to think about the educational aspects of a population and direct interventions, that is, from preventive counselling until physical exercise and drug therapies.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML