-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2015; 5(6): 221-227
doi:10.5923/j.sports.20150506.01

Remotely-Guided Feedback Enhances Exercise Training Adherence and Physical Performance in Firefighters
Brett A. Dolezal, Jordan G. Waite, Eric V. Neufeld, David M. Boland, Christopher B. Cooper
Departments of Medicine and Physiology, David Geffen School of Medicine at UCLA, Los Angeles, USA
Correspondence to: Eric V. Neufeld, Departments of Medicine and Physiology, David Geffen School of Medicine at UCLA, Los Angeles, USA.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

This study examined the influence of guided, individualized text message-based feedback (GTF) versus unguided, generic text message-based feedback (UTF) on adherence to an exercise training protocol and select physical performance parameters in a cohort of firefighters. Over one month, firefighters at two separate fire departments (n=16) donned wearable physiological status monitors (PSMs) and engaged in unsupervised aerobic exercise for at least 30 minutes three times weekly. Self-administered baseline measures included body mass (BM), body fat percentage (%BF), and maximal oxygen uptake (VO2max) derived from a standard firefighter treadmill protocol. Data was remotely captured from the participants while exercising, securely transferred and processed using a digital health network (DHN). Firefighters were randomized into two groups: those that received GTF and those that received UTF. According to the discretion of the investigators, appropriate text message-based feedback was sent depending on participant group and individual exercise performance. Multiple metrics were monitored during training including heart rate, time in a target heart rate zone (%THRZ) and % adherence to training (%ADHR). The GTF group showed greater increases in exercise time, %THRZ, and %ADHR in conjunction with, decreased BM and BF%, and greater improvements in VO2max. All reported p-values were p<0.01. This study shows that GTF resulted in greater adherence to exercise training and improved fitness measures in firefighters over UTF.
Keywords: Exercise Adherence, Firefighter, Text Message-Based Intervention
Cite this paper: Brett A. Dolezal, Jordan G. Waite, Eric V. Neufeld, David M. Boland, Christopher B. Cooper, Remotely-Guided Feedback Enhances Exercise Training Adherence and Physical Performance in Firefighters, International Journal of Sports Science, Vol. 5 No. 6, 2015, pp. 221-227. doi: 10.5923/j.sports.20150506.01.
Article Outline
1. Introduction
- Although advances in technology may have resulted in the unintended removal of physical activity from daily life, over the past few years researchers, healthcare professionals, and fitness practitioners have embraced these same technologies as a means of facilitating active, healthy lifestyles. This emerging digital health arena has the potential to greatly extend the reach of healthcare or fitness professionals. While a person can be physically present in only one place at a time, automated text messages, e-mails, social media, and integrated websites allow for simultaneous feedback to countless individuals around the world. Furthermore, continued technological advances have seen a burgeoning industry for wearable activity monitors that provide an integrated acquisition and analysis platform for unobtrusive monitoring of physiological data. This represents a major groundswell of change which is transforming the faces of both the clinical healthcare and consumer fitness industries [1].A number of systematic reviews postulate that technology-assisted interventions are indeed feasible and efficacious in promoting physical activity, weight loss and cardiometabolic health [2-5]. Studies that focused on one or two forms of media (e.g., e-mail and/or websites) arrived at similar conclusions [6]. Key characteristics of successful interventions appear to be clear instructions and specific, personalized feedback that incorporate some form of social support [7, 8]. Additionally, a substantial amount of research has specifically examined the efficacy of text message-based interventions in a variety of populations and arrived at positive outcomes [9-13]. Very recently, Hall et al. (2015) found the majority of text message-based interventions utilizing social-cognitive behavioral models to be effective in improving risk factors for and managing symptoms of a wide variety of health parameters and illnesses [14].The majority of research to date has focused on clinical settings with little investigation into the effects of these interventions on individuals in a workplace environment. Men and women whose careers are defined by responding to emergency situations, such as firefighters and other first responders, often exhibit the same cardiovascular risk factors as the general population, albeit compounded by stressful and physically demanding work requirements [15]. Recently, the UCLA Exercise Physiology Research Laboratory, in collaboration with the Department of Homeland Security, developed the Physiological Health Assessment System for Emergency Responders (PHASER) program in an effort to identify a comprehensive risk assessment of firefighters and design mitigation strategies leveraging digital health technology to reduce the disproportionately high number of firefighter line-of-duty deaths attributed to cardiovascular and cerebrovascular events [16]. Subsequently a 'call to action' for the first responder community to embrace lifestyle changes, which targeted exercise initiatives to offset the high prevalence of adiposity and lack of cardiovascular fitness, gave birth to a low-cost, remote physiological monitoring system called PHASER-Net. This system architecture, described fully in Batalin et al. (2013), connects first responders to healthcare and fitness practitioners via smartphones, wearable physiological status monitors, and a secure web portal for meaningful and actionable communication of biometric data and feedback [17].One facet of the risk reduction effort is focused on improving adherence to cardiovascular exercise routines, which builds on established social-cognitive models associated with changes in health behavior. Using the PHASER-Net system, the present study aimed to assess the influence of guided or unguided text message-based feedback on 1-month of exercise training adherence and physical fitness among career firefighters.
2. Methods
2.1. Participants
- Sixteen active-duty career firefighters (from two metropolitan city fire departments in the southwestern United States) voluntarily participated in this 1-month intervention. Firefighters were randomized into one of two groups: individualized, guided text message-based feedback (GTF; n=8) or a control that included unguided text message-based feedback (UTF; n=8). The study was approved by the UCLA Institutional Review Board and all participants gave written informed consent. Participants completed standard health, medical, and exercise history forms following enrollment and prior to data acquisition.
2.2. Remote Data Capture
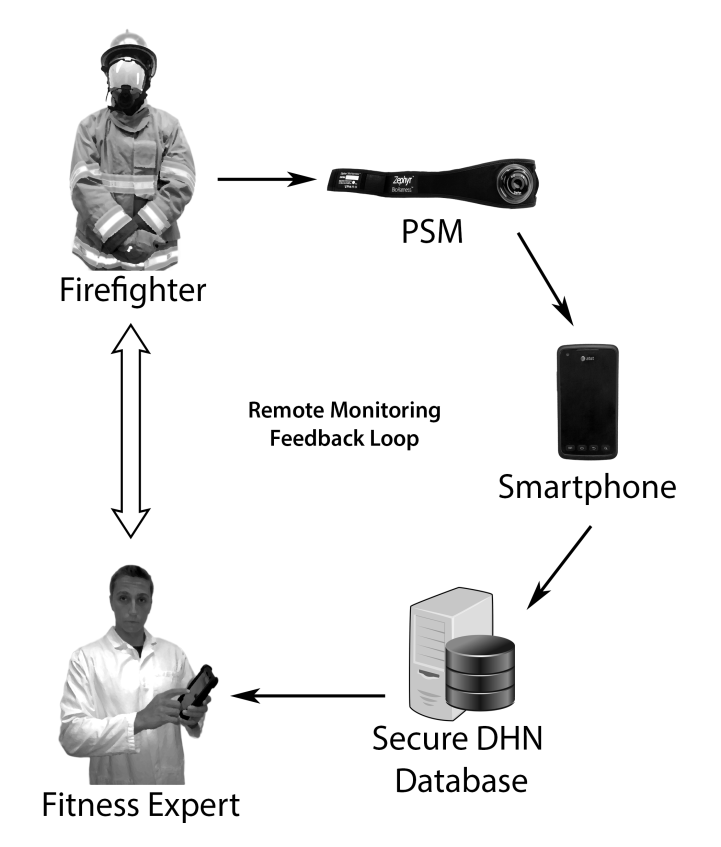
- Prior to study initiation, each subject completed a detailed, step-by-step instructional tutorial on how to use the PHASER-Net architecture including donning the physiological status monitor (PSM) affixed to a chest strap (BioHarness-3; Zephyr Technologies, Annapolis, MD).This commercially manufactured wearable multi-sensor system was worn for baseline and post-test assessments and during exercise sessions [17] [18]. The device captures, logs, and visualizes vital signs and tri-axial accelerometry metrics via Bluetooth enabled devices (e.g., Android smartphone). These data are transmitted via a secure internet protocol and uploaded to an encrypted, secured web server at the UCLA Exercise Physiology Research Laboratory for data analytics. Based on training session data, a study associate can send appropriate feedback to the firefighter via text-based messaging incorporated within the network (see Figure 1).
2.3. Baseline and Post-Assessments
- Baseline and 1-month post-assessments were remotely self-administered following strict guidelines and included body mass (BM), body fat percentage (%BF), and maximal oxygen uptake (VO2max).Prior to assessment of BM and %BF, the participants were instructed to remain euhydrated and abstain from heavy exercise for 12 hours beforehand. After a web-based explanation of the measurement procedure, the participant stood upright with the ball and heel of each foot on two metallic footpads with both hands gripping a bar with metallic electrodes using a recently validated, octopolar, multi-frequency bioelectrical impedance analysis scale (InBody R20 scale, Biospace, Inc, Seoul Korea) [19]. The instrument measured BM and %BF within 30 seconds and the data was automatically synchronized and uploaded to PHASER-Net.The PHASER-Net system also contains functionality for the participant to self-administer a submaximal VO2max treadmill test based on the Fire Service Joint Labor Management Wellness-Fitness Initiative (WFI) [20]. The system guides the participant through the steps required to perform the test, while collecting heart rate data, monitoring for test termination criteria and computing an estimated VO2max upon test completion. In short, the WFI treadmill test is a modified ramp protocol with 1-minute intervals of alternate increases in speed (0.5 mph) and gradient (2%). The test is terminated when the participant has reached 85% of their age-predicted maximum heart rate as measured via PSM for at least 15 seconds. For both groups, individualized target heart rate zones (THRZs) were developed based on participant’s initial VO2max assessment from an automated algorithm developed in PHASER-Net [17]. On a weekly basis thereafter, THRZs were manipulated within PHASER-Net based on the prior week’s training results. The goal was to increase the THRZ intermittently to progressively challenge the cardiovascular system throughout 1 month of training.
2.4. Exercise Training
- Participants were asked to don the PSM and exercise three times weekly, preferably every other day, for four consecutive weeks. Throughout the exercise sessions, participant smartphones provided a visual display of real-time exercise duration, and heart rate with upper- and lower-limit demarcation lines indicating the THRZ to which they should adhere. Session metrics also included exercise duration, the duration of time spent within the target heart rate zones (%THRZ), and the percent adherence to training (%ADHR) out of 12 sessions.Prior to the first day of training, all participants were given web-based instructions to help them attain a level of cardiovascular exercise that comports with the American College of Sports Medicine Physical Activity Guidelines [21]. In addition to informing the participants of the exercise guidelines, this type of instruction allowed the participant greater flexibility in chsoosing cardiovascular exercises that accommodated existing facilities and equipment.
2.5. Text Message-Based Feedback
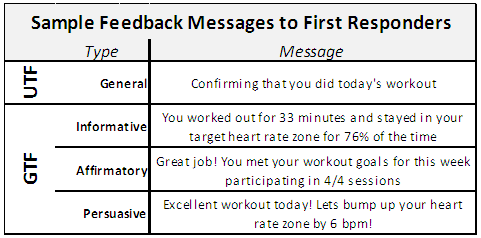
- During the course of the 4-week study, participants in both groups received 20 daily guided or unguided text message-based feedback that either utilized positive reinforcement techniques including informative, affirmatory, and persuasive content (i.e., guided) or, conversely, unguided messages that remained neutral and generic in nature.
2.6. Data Analysis
- Baseline and 1-month data are reported with descriptive statistics. Changes in all outcome variables were assessed by dependent t-tests. Comparisons for differences between groups were assessed with independent t-tests. Statistical significance was accepted at P<0.05.Due to the small sample size, all results were confirmed by rank-based testing using bootstrap techniques. Rank-based testing has been suggested for small sample sizes as it minimizes the impact of outlier results. This approach involved combining the results from both groups and ranking them 1-16 for each variable. The difference in mean rank for each group was then calculated and 95% confidence intervals were determined by resampling to replicate the experiment 10,000 times, calculating a new difference in group means for each replication. Statistical significance was measured by running a null hypothesis significance test with α=0.05 to ensure the observed difference in means did not fall within the values possible from a true null hypothesis.
3. Results
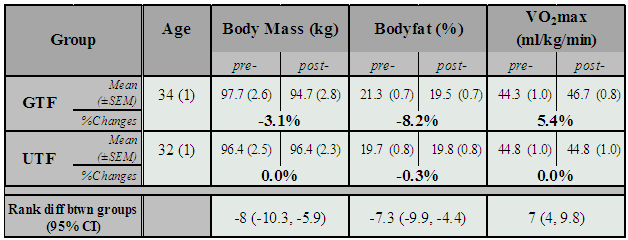
3.1. Fitness Outcomes
- The two groups were well matched in terms of age and fitness at baseline. The GTF group demonstrated significant improvements in each of the fitness outcome measures (P<0.01, see Table 2), while the UTF group did not show significant changes in any of the measures. Furthermore, the percentage change for each fitness outcome was greater for the GTF group compared to the UTF group (P<0.01). The greater improvements observed in the GTF group were corroborated by rank-based testing.
|
|
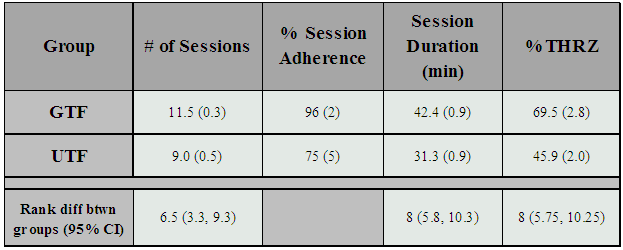
3.2. Exercise Adherence
- The GTF group compared to the UTF group demonstrated increased %ADHR in terms of number of sessions, duration of training, and achievement of target heart rate (P<0.01). The group receiving individualized feedback (GTF) had a 21% better session adherence rate, exercised 11 minutes longer, and spent 24% more time in their THRZ. Significant differences between the groups in each measure were also observed with rank-based testing techniques where the mean rank of the GTF group was 8 places higher than the UTF group in both session duration and time spent in THRZ.
4. Discussion
- Employing specific, guided text message-based feedback via PHASER-Net proved efficacious for improving exercise adherence and performance in firefighters when compared to those receiving unguided feedback. Specifically, participants demonstrated greater improvements in cardiovascular fitness and decreases in body fat percentage, both known to attenuate the risk of morbidities, especially cardiovascular disease, obesity, and diabetes [22, 23]. Our findings demonstrate that the inclusion of individualized feedback prompted more frequent and more effective exercise sessions. A major limitation to our study is the small sample size; however, we used rank-based testing and bootstrap replication techniques to in addition to standard two-group testing of the means, to attempt to control for this limitation. While these statistical techniques indicate that our results are indeed due to true differences, larger studies should be conducted. Additionally, our study design organized all participants at one fire station into the GTF group and all participants at another station into the UTF group. This was done because the organizational realities of the fire departments did not allow for separating the groups. Certainly, it is possible that one fire station created a more motivating and supportive work environment or that a difference in mission load may have affected our data. Recognizing this, it is important that larger, multi-center studies be conducted in the future to confirm these results in firefighters.Despite these limitations, our results are concordant with conclusions drawn from other studies that explored the efficacy of tailored versus untailored messages via a text-message delivery system: that is, individualized feedback increases motivation and positive behavioral outcomes [24, 25]. The benefits of tailored feedback, however, are not limited to text messaging. Bull et al. (2001) found that individuals were more likely to adhere to suggested changes in behavior from printed health educational materials specifically tailored to them rather than a general audience [26]. In short, guided feedback is more salient and relevant than unguided feedback, and as a result, has a greater probability of being remembered after the message is shown. This phenomenon would help explain why the GTF participants in this study showed a greater increase in the total time spent exercising and the percentage of workouts completed. The increase in these two parameters suggests an elevation in the intrinsic desire to exercise. If extrinsic motivation (specific, guided text messages) is able to directly augment intrinsic motivation, especially long term, this presents an alternative argument to one of the most prevalent criticisms of digital health [27, 28]. Future studies will be needed to develop convincing evidence that such a phenomenon is achievable. There are several other criticisms that tend to be levelled at digital health research studies. Participant adherence is a common problem—the potential benefits of digital-health based interventions persist only as long as subjects continue to properly use the given technology [27]. From a methodological standpoint, the majority of current digital health research struggles to maintain the internal validity of a randomized control trial while simultaneously possessing the generalizability of an observational study [28]. With these points in mind, counterarguments cannot completely negate the potential benefits of extrinsic motivation on both adherence to fitness regimens and athletic performance. Considering a minority of individuals has the means to hire a professional trainer for individual encouragement every time they engage in exercise, text message-based interventions provide an attractive alternative. This technology could be especially valuable for at-risk occupational groups, notably firefighters, since failure to maintain an appropriate level of aerobic conditioning can result in disastrous consequences [15].One noteworthy study [29], investigated the effects simply implementing intentions on the level of physical exercise in volunteer firefighters In the experimental group, participants composed on paper where, how and when they would exercise. The investigators concluded that implementation intention formation promotes an increase in physical exercise in volunteer firefighters who do not exercise regularly. Inciting healthy behaviors in firefighters has an added benefit: positive behavioral changes regarding health and exercise that occurred in only a few firefighters quickly propagated throughout the entire fire station [30]. Emphasizing the importance of physical activity in a couple members of the team led to long-term alterations that spread to new hires and showed up in firefighter-sponsored public health awareness campaigns.In addition to occupational benefits, exercise shows promise as an intervention in clinical settings. Several investigators, for example, postulate exercise to be a necessary adjunct to the more traditional treatment for stimulant use disorders [31, 32]. Utilizing digital health technology helps overcome some of the collective barriers (e.g., lack of supervision, high cost, logistical) noted in drug rehabilitation programs [33].One of the most prevalent forms of technology-assisted exercise is the download and self-use of smartphone-based fitness applications. The majority of these, however, do not incorporate multiple components of behavior change techniques to motivate behavior change and promote sustainability [34]. In order to create effective health behavior interventions, Fishbein et al. (2003) suggest that behavior change is mediated by (i) attitudes about the behavior (i.e., perceived costs versus benefits); (ii) perceived norms (e.g., social support, community); and (iii) sense of self-efficacy about performing the behavior [35]. By incorporating messages within different categories to facilitate these components of behavior change theory, text message-based interventions are expected to improve and sustain changes in physical activity levels. In summary, individualized feedback in combination with wearable activity sensors, which may themselves stimulate long-term engagement in desired behaviors, can maximize health outcomes by incorporating elements of education, flexibility, and motivation.
5. Conclusions
- Although exercise has been shown to have definitive health benefits for the vast majority of the general population, sedentary behavioral habits still pervade modern society and amplify the risk of cardiovascular disease. Accumulating evidence continues to demonstrate that digital health interventions—monitored by healthcare professionals and/or fitness practitioners (i.e., experts)—provide efficacious methods of facilitating behavioral changes through the use of wearable sensors. This study showed that guided, when compared to unguided text message-based feedback, greatly increased firefighters’ exercise adherence and performance which may ameliorate their risk for premature death and many lifestyle diseases. By incorporating digital health technology to broaden access to exercise, individualize prescribed regimens, and facilitate adherence, common limitations recognized in the first responder community can be diminished.
ACKNOWLEDGEMENTS
- The research presented in this paper was funded by a contract with the Department of Homeland Security Science and Technology Directorate (as part of the UCLA PHASER program). We are very appreciative of the participants who so ably and enthusiastically participated in this study.
References
| [1] | Dolezal, B. A., Abrazado, M., Batalin, M. A., Smith, D., & Cooper, C. B. (2014). Deployment of remote advanced electrocardiography for improved cardiovascular risk assessment in career firefighters. Telemed J E Health, 20(7), 660-663. |
| [2] | Connelly, J., Kirk, A., Masthoff, J., & MacRury, S. (2013). The use of technology to promote physical activity in Type 2 diabetes management: a systematic review. Diabet Med, 30(12), 1420-1432. |
| [3] | Allen, J. K., Stephens, J., & Patel, A. (2014). Technology-assisted weight management interventions: systematic review of clinical trials. Telemed J E Health, 20(12), 1103-1120. |
| [4] | Lee, S., & Lindquist, R. (2015). A review of technology-based interventions to maintain weight loss. Telemed J E Health, 21(3), 217-232. |
| [5] | Widmer, R. J., Collins, N. M., Collins, C. S., West, C. P., Lerman, L. O., & Lerman, A. (2015). Digital health interventions for the prevention of cardiovascular disease: a systematic review and meta-analysis. Mayo Clin Proc, 90(4), 469-480. |
| [6] | Sriramatr, S., Berry, T. R., & Spence, J. C. (2014). An Internet-based intervention for promoting and maintaining physical activity: a randomized controlled trial. Am J Health Behav, 38(3), 430-439. |
| [7] | Eckhardt, M. R., Kerr, J., & Taylor, W. C. (2015). Point-of-Decision Signs and Stair Use in a University Worksite Setting: General Versus Specific Messages. Am J Health Promot, 29(5), 291-293. |
| [8] | Yang, C. H., Maher, J. P., & Conroy, D. E. (2015). Implementation of behavior change techniques in mobile applications for physical activity. Am J Prev Med, 48(4), 452-455. |
| [9] | Collins, T. C., Dong, F., Ablah, E., Parra-Medina, D., Cupertino, P., Rogers, N., & Ahlers-Schmidt, C. R. (2014). Text messaging to motivate exercise among Latino adults at risk for vascular disease: a pilot study, 2013. Prev Chronic Dis, 11, E192. |
| [10] | Maddison, R., Pfaeffli, L., Whittaker, R., Stewart, R., Kerr, A., Jiang, Y., . . . Rawstorn, J. (2015). A mobile phone intervention increases physical activity in people with cardiovascular disease: Results from the HEART randomized controlled trial. Eur J Prev Cardiol, 22(6), 701-709. |
| [11] | Fassnacht, D. B., Ali, K., Silva, C., Goncalves, S., & Machado, P. P. (2015). Use of text messaging services to promote health behaviors in children. J Nutr Educ Behav, 47(1), 75-80. |
| [12] | Yan, A. F., Stevens, P., Wang, Y., Weinhardt, L., Holt, C. L., O'Connor, C., . . . Luelloff, S. (2015). mHealth text messaging for physical activity promotion in college students: a formative participatory approach. Am J Health Behav, 39(3), 395-408. |
| [13] | Shaw, R. J., Bosworth, H. B., Silva, S. S., Lipkus, I. M., Davis, L. L., Sha, R. S., & Johnson, C. M. (2013). Mobile health messages help sustain recent weight loss. Am J Med, 126(11), 1002-1009. |
| [14] | Hall, A. K., Cole-Lewis, H., & Bernhardt, J. M. (2015). Mobile text messaging for health: a systematic review of reviews. Annu Rev Public Health, 36, 393-415. |
| [15] | United States Fire Administration (2014). Fire Fighter Fatalities in the United States in 2013. |
| [16] | Storer, T. W., Dolezal, B. A., Abrazado, M. L., Smith, D. L., Batalin, M. A., Tseng, C. H., & Cooper, C. B. (2014). Firefighter health and fitness assessment: a call to action. J Strength Cond Res, 28(3), 661-671. |
| [17] | Batalin, M., Yuen, E., Dolezal, B., Smith, D., Cooper, C., & Mapar, J. (2013). PHASER: Physiological Health Assessment System for Emergency Responders [unpublished]. |
| [18] | Dolezal, B.A., Barr, D., Boland, D.M., Smith, D.L., Cooper, C.B. (2015). Validation of the firefighter WFI treadmill protocol for predicting VO2 max. Occup Med (Lond), 65(2): 143-146. |
| [19] | Dolezal, B.A., Boland, D.M., Carney, J., Abrazado, M., Smith, D.L., Cooper, C.B. (2014). Validation of heart rate derived from a physiological status monitor-embedded compression shirt against criterion ECG. J Occup Environ Hyg, 11(12): 833-839. |
| [20] | Dolezal, B.A., Lau, M., Abrazado, M., Storer, T.W., & Cooper, C.B. (2013) Validity of two commercial grade bioelectrical impedance analyzers for measurement of body fat percentage. Journal of Exercise Physiology online, 16(4), 74-83. |
| [21] | Garber, C. E., Blissmer, B., Deschenes, M. R., Franklin, B. A., Lamonte, M. J., Lee, I. M., . . . Swain, D. P. (2011). American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc, 43(7), 1334-1359. |
| [22] | Cornelissen, V. A., Fagard, R. H., Coeckelberghs, E., & Vanhees, L. (2011). Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension, 58(5), 950-958. |
| [23] | Pattyn, N., Cornelissen, V. A., Eshghi, S. R., & Vanhees, L. (2013). The effect of exercise on the cardiovascular risk factors constituting the metabolic syndrome: a meta-analysis of controlled trials. Sports Med, 43(2), 121-133. |
| [24] | Fjeldsoe, B. S., Marshall, A. L., & Miller, Y. D. (2009). Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med, 36(2), 165-173. |
| [25] | Bauer, S., de Niet, J., Timman, R., & Kordy, H. (2010). Enhancement of care through self-monitoring and tailored feedback via text messaging and their use in the treatment of childhood overweight. Patient Educ Couns, 79(3), 315-319. |
| [26] | Bull, F. C., Holt, C. L., Kreuter, M. W., Clark, E. M., & Scharff, D. (2001). Understanding the effects of printed health education materials: which features lead to which outcomes? J Health Commun, 6(3), 265-279. |
| [27] | Patel, M. S., Asch, D. A., & Volpp, K. G. (2015). Wearable devices as facilitators, not drivers, of health behavior change. JAMA, 313(5), 459-460. |
| [28] | Beedie, C., Mann, S., Jimenez, A., Kennedy, L., Lane, A. M., Domone, S., . . . Whyte, G. (2015). Death by effectiveness: exercise as medicine caught in the efficacy trap! Br J Sports Med. |
| [29] | Hammer, R.L. (2010). The Effects of Implementation Intentions on Volunteer Firefighter Exercise Behavior: A Randomized Control Study. |
| [30] | Mabry, L., Elliot, D. L., Mackinnon, D. P., Thoemmes, F., & Kuehl, K. S. (2013). Understanding the durability of a fire department wellness program. Am J Health Behav, 37(5), 693-702. |
| [31] | Dolezal, B. A., Chudzynski, J., Storer, T. W., Abrazado, M., Penate, J., Mooney, L., Cooper, C. B. (2013). Eight weeks of exercise training improves fitness measures in methamphetamine-dependent individuals in residential treatment. J Addict Med, 7(2), 122-128. |
| [32] | Mooney, L. J., Cooper, C., London, E. D., Chudzynski, J., Dolezal, B., Dickerson, D., . . . Rawson, R. A. (2014). Exercise for methamphetamine dependence: rationale, design, and methodology. Contemp Clin Trials, 37(1), 139-147. |
| [33] | Read, J. P., Brown, R. A., Marcus, B. H., Kahler, C. W., Ramsey, S. E., Dubreuil, M. E., . . . Francione, C. (2001). Exercise attitudes and behaviors among persons in treatment for alcohol use disorders. J Subst Abuse Treat, 21(4), 199-206. |
| [34] | Conroy, D. E., Yang, C. H., & Maher, J. P. (2014). Behavior change techniques in top-ranked mobile apps for physical activity. Am J Prev Med, 46(6), 649-652. |
| [35] | Fishbein, M., Hennessy, M., Yzer, M., & Douglas, J. (2003). Can we explain why some people do and some people do not act on their intentions? Psychol Health Med, 8(1), 3-18. |
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML