-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
International Journal of Sports Science
p-ISSN: 2169-8759 e-ISSN: 2169-8791
2015; 5(4): 151-155
doi:10.5923/j.sports.20150504.06
Proximal and Distal Rupture of the Biceps of the Arm in Athletes
Benigno Zenteno M. D.
Escuela de Medicina Universidad Durango Campus Chihuahua
Correspondence to: Benigno Zenteno M. D., Escuela de Medicina Universidad Durango Campus Chihuahua.
| Email: |  |
Copyright © 2015 Scientific & Academic Publishing. All Rights Reserved.
OBJECTIVES. -To help become familiar to all Sports Professionals with this type of injuries in athletes. Remarking the difficulty to realize the clinical and imaging diagnosis. Emphasizing arthroscopy as an essential tool for the diagnosis in proximal lesions. And to offer the current modalities of management and in the distal injury to suggest one incision and the utilization of biodegradable material as fixation devices. Conclusions. - The injuries of the biceps tendon are primarily diagnosed with clinical and auxiliary imaging devices, but it is often necessary the arthroscopic corroboration in proximal lesions. The current techniques for fixation of the long head are various, but alike the distal injuries, the early fixation with biodegradable screws give an option biomechanically stable and promote the integral rehabilitation of the athlete.
Keywords: Biceps, Tendon injuries, Athletes
Cite this paper: Benigno Zenteno M. D., Proximal and Distal Rupture of the Biceps of the Arm in Athletes, International Journal of Sports Science, Vol. 5 No. 4, 2015, pp. 151-155. doi: 10.5923/j.sports.20150504.06.
1. Introduction
- One of the more important and disturbing questions of an athlete with a biceps injured is: what is the percentage of the tear? And what will be the deficiency if I do not have a surgical reconstruction? The answer to these questions by the treating physician is controversial and imprecise including those using sophisticated imaging studies. [1, 2, 7, 10, 11, 14, 18, 19].An adequate arthroscopic inspection of the affected shoulder, is one of the more important steps for the diagnosis and treatment of chronic tendinitis in the proximal insertion of the biceps tendon, which can evolve to a partial rupture, or the absence of the insertion of the long head in the glenoid. [2, 10, 15].At the other end of the extremity, the distal tendon rupture of the biceps is an uncommon reported lesion, but there is a general consensus that it will leave sequel in the sports practitioner if it is not managed surgically [4, 5, 16]. Avoiding this kind of reconstructions by some surgeons for their potential complications reported previously in the literature [9, 12, 16, 19].The objective of these case presentations is to provide a clear idea of the usefulness of arthroscopy for the proximal injury in athletes, as a diagnostic and therapeutic tool, and at the same time the current modalities in their management. Related to the distal pathology, to offer a simple and effective approach for the sports people with this lesion. And concluding that if they are treated adequately, the athletes can return to their sports at the same level before their injuries.
2. Case 1
- A 38 year male tennis player and weight lifter, felt a “cracking” in his right dominant shoulder, with no previous pain at all, this event occurred after weight lifting in the “preacher” bench curl. After that, he noticed a difference in volume of his arms (Fig 1). At office consultation an imprecise ultrasound diagnosis was presented, and we decided to realize and arthroscopic procedure, where we found a complete rupture of the long head of the biceps reflected by an absence of the insertion of the tendon in the glenoid (Fig. 2).
 | Figure 1. 38 Years Tennis Player |
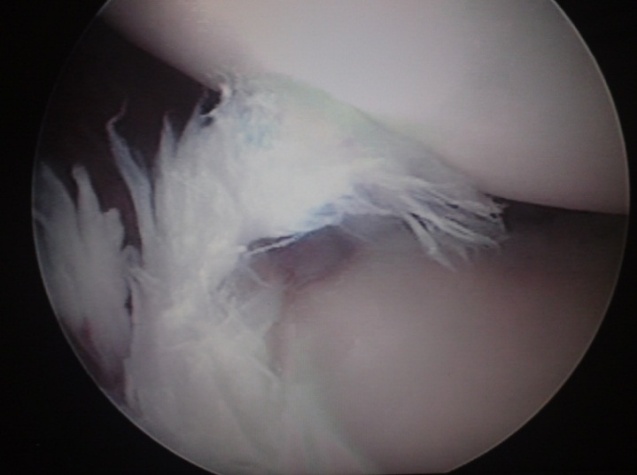 | Figure 2. Arthroscopic Findings |
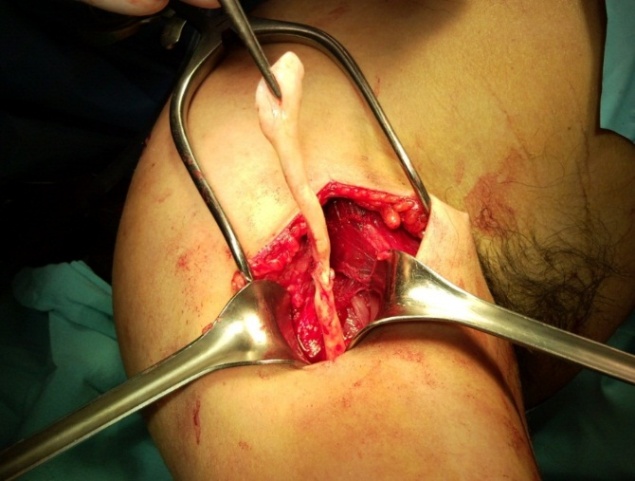 | Figure 3. Surgical Findings. Subpectoral Approach |
 | Figure 4. Fixation with Biodegradable screw |
3. Case 2
- A 60 year old right handed swimmer, with an average swimming f 2 Km. 4 times a week during 40 years, started with pain in the left shoulder 1 year before consultation. Three months before her office appointment the pain was present during all day and required constant analgesic administration. She noticed a “deformation” of the arm (Fig. 6), limitation of the arc of motion and crepitation during abduction.At physical examination we found pain in the ventral portion of the left shoulder, corresponding to the intertubercular groove of the humerus, positive “Popeye” and Speed signs, and negative “bear hug sign” [10, 11].The MRI reported: Injuries of the subscapular and long head of the biceps, without mentioning the supraspinatus tendon.At arthroscopy the findings were: Partial rupture of the subscapular tendon, and a complete rupture of the long head of the biceps at the glenoid insertion (Fig. 7). In the sub acromial space, a complete rupture of the supraspinatus tendon was found.A sub acromialarthroplasty was performed for a grade III acromion. And a biotenodesis of the long head of the biceps was performed with a biodegradable screw at the intertubercular groove level of the proximal humerus. The supraspinatus tendon was repaired with a “mini-open” incision with two metal anchors. 2.6 years after the surgery she is swimming again at the same level previous to her ailments (Figure 8). UCLA classification: 33 points.
 | Figure 5. 2.8 years After the surgery. Playing Tennis And lifting weights |
 | Figure 6. A 60 Year old swimmer, Long head biceps rupture |
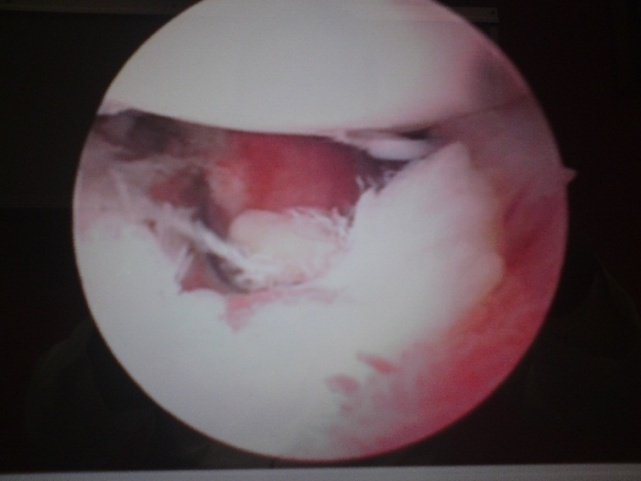 | Figure 7. Arthroscopic Findings of the female Swimmer |
 | Figure 8. 2.6 Years After the Surgery |
4. Case 3
- A 48 year, Male boxer and “weight lifter”, presented with a history of been fighting and when he hit the contrary on his pelvis, felt a sudden pain in his left arm, followed by edema and ecchymosisin the elbow (Fig. 9). After a sonographic examination a “partial injury of the biceps” was reported in the “musculo-tendinous” portion.
 | Figure 9. 48 year Boxer with a Complete distal Biceps Rupture. Left arm |
 | Figure 10. Aponeurotic expansion of the biceps |
 | Figure 11. Distal left biceps 3 Years after the surgery Left arm |
 | Figure 12. Same Patient in figure 11 with the right proximal Biceps tendon repaired with subpectoral technique. 2.6 Years after the surgery |
5. Discussion
- The complaints of the “shoulder” are common in athletes that use frequently the arms for their respective sports. This broad anatomic area is full of pathologic conditions, which etiology is in the majority of cases an “abuse” of the joints, with the development of “fatigue” and the loss of the appropriate biomechanics of the long head of the biceps which acts as a depressor of the humeral head and also being primordial in the acceleration and deceleration movements of the arm. [3, 6].The correct diagnosis is not easy to realize, mainly in partial injuries where the false negatives studies are reported [21]. The lesions located at the “entrance” of the intertubercular groove are difficult to diagnose including those studied with a “high resolution” MRI. [1, 7, 10, 11, 14, 18].The only precise diagnostic tool for the ruptured long head of the biceps is the “arthroscope”, but must be handled by “expert orthopedic arthroscopic surgeons” [10].The surgeon must have enough dexterity and experience to inspect adequately the long head of the biceps including the extra-articular portion in the “entrance” at the intertubercular groove and be prepared during the same surgical procedure to handle any kind of injury, e.g.: tenotomy, biceps fixation to the humerus, including a sub pectoral incision if this is necessary, mentioning the literature this last option as the safest for athletes [2, 3, 6, 17].Talking about the distal biceps, the diagnosis is neither easy as in the proximal injury. Some authors recommend the Hook test, but we found it difficult to elicit in the acute injured athlete because of the presence of pain an edema in the area [22]. We trusted more in the history of the patient, with an eccentric extension load applied to the elbow [16], pain in the injured area and the presence of ecchymosis at the forearm (Figure 9). Because of these positive clinicals signs we decide to take the patients to the operating room despite the diagnosis of “partial” tear made by the sonographic radiologic reports [19].We found the trend from people attending athletes to suggest “not repair these distallesions”, maybe based on the uncommon of the injury and also thinking about the complications reported in the literature, e.g: the iatrogenic injury of the median and musculocutaneousnerves [9].Nonetheless, no matter the controversial issues related to these problems of the distal biceps , the current approach in sports people is to repair as soon as possible these lesions in athletes, with an anatomic fixation, to offer the patient the maximum muscular strength, avoiding also a lack of flexion or supination in the future [4, 8, 12].The utilization of biodegradable materials provides the athlete the advantage of enough biomechanic strength of the biotenodesis implant, without the disadvantages of the “metallic screws” or other kind of non-degradable materials. The current biodegradable screws allow the athlete to obtain an integral rehabilitation because of the early mobilization of the injured arm. [5, 19].In conclusion if we diagnose and treat adequately these athletes we can return them to their previous levels in their sports with minimum morbidity and this results are maintained in the long term follow up.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML