-
Paper Information
- Next Paper
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
American Journal of Sociological Research
p-ISSN: 2166-5443 e-ISSN: 2166-5451
2012; 2(5): 107-112
doi: 10.5923/j.sociology.20120205.03
The Difficulty and Significance of NursingPracticeUsing Complementary and Alternative Medicine (CAM)
Masako Nagase, Mayumi Takaya
Juntendo University, Faculty of Health Care and Nursing
Correspondence to: Masako Nagase, Juntendo University, Faculty of Health Care and Nursing.
| Email: |  |
Copyright © 2012 Scientific & Academic Publishing. All Rights Reserved.
Japan’s national healthcare system is based solely on modern medicine. This study aims to clarify the expectations surrounding CAM and the factors hindering the practice of CAM in nursing. The informants for the interview survey were five nurses who have had professional training in aromatherapy. We asked them about their expectations ofCAM and about the difficulty of nursing care as a CAM practitioner. Whether or not informants were using CAM in their work, they understood the difficulty nursesface in attempting to practice CAM therapy.We found thatapproval of the boss and co-workers is indispensable for using CAMin nursing care. In addition, the practitioner must show evidence that the therapy works. Informants spoke of the difficultyofshowing evidence when it is not possible to do a clinical study. On the other hand, the view on the value of CAMnursing may be revisedif nurses can show the evidence for its efficacy and if the therapy can become more widespread.Nursing science may be able to contribute to the evidence, and healthcare system reform could facilitate its wider use.
Keywords: Nursing Care, Complementary and Alternative Medicine, Feasibility, Aromatherapy, Lymphatic Drainage
Cite this paper: Masako Nagase, Mayumi Takaya, "The Difficulty and Significance of NursingPracticeUsing Complementary and Alternative Medicine (CAM)", American Journal of Sociological Research, Vol. 2 No. 5, 2012, pp. 107-112. doi: 10.5923/j.sociology.20120205.03.
Article Outline
1. Introduction
- Over the past decade, there has been a growing interest in complementary and alternative medicine (CAM) in nursing[1][2]. As of 2009, 581 nursing articles about CAM had been published in the Japan CentraRevuoMedicina, which accounted for 5.4% of all articles (14,483), including both medicine and psychology[1]. Although the proportion of nursing articles is still very low, the number of nursing articles increased 5 times from 1998 to 2007, suggesting an increasing awareness of CAM in nursing practice.According to Snyder, nurses provide holistic care, which could include CAM[3]. In Japan, however, such practices as aromatherapy and reflexology, which are part of CAM, are not considered to be a part of nursing care.Many nurses, however, consider that it is important to adopt CAM in clinical nursing[4][5][6], and many of them actively participate in seminars to study CAM[5][6]. In our survey[7], which involved nurses working at university hospitals in the Tokyo Metropolitan Area, the results indicated a growing awareness of CAM, especially aromatherapy, reflexology, and music therapy. However, of the 92.7% of nurses who considered it important to adopt CAM in nursing, those who have actually administeredit accounted for only 52.1%.One of the reasons for the relative scarcity of CAM practice may be that an appropriate social network is lacking[8]. A social network fulfils the function of providing social mechanisms that affect individual behavior and thoughts,and by which people determine their social actions; that is, action are influenced less by personal qualities, such as interests and abilities, and more by other members of the social network—in the context of nursing, then, by other nurses.Our report[7] also showed an association between the use of CAM and social networks;nurses might receive support from friends or colleagues who share their interest in CAM. On the other hand, we found no association between an interest in CAM and its practice, suggesting that the determination to perform CAM is more closely affected by relationships with colleagues rather than by personal factors, such as an interest in or learning of CAM. Another possible reason is that the efficacy of CAM has not been “scientifically” proven, which has led people either to have negative views about CAM or to have suspended judgment[9][10][11]. In fact, clinical nurses consider that professional knowledge and skills as well as scientific evidence are essential in order to use CAM in nursing practice[7].As Snyder pointed out, if nursesare supposed to function as “holistic” nursing practitioners, it is inevitable that they will have an interest in and expectations for CAM interventions. Despite the many problems that exist in using CAM in nursing practice, it may be necessary to create an environment where CAM can be practiced if it is considered a necessary nursing intervention. Thus, this study searched for causes of the difficulties in using CAM in nursing practice.We administered an interview survey involving nurses who try to acquire professional knowledge of and skills with aromatherapy or lymphatic drainage for regular use in clinical settings.
2. Purpose
- The purpose of this paper is toclarify the difficulty of using CAM therapy in routinenursing practice. In addition, wediscuss the significance of CAM therapy use and what it means for nursesto lettheir bosses and colleaguesknow that they use CAM therapy.<Definitions>Complementary and alternative medicine: Aromatherapy, lymph drainage and music therapy; general terms for treatments complementing or substituting conventional medicine.Therapy: Refers to individual therapies that form a part of CAM.
3. Method
3.1. Selection of Target Population
- In order to participate in the survey, informants had to (a) be registered nurses, (b) have learned about at least one CAM therapy, such as aromatherapy or lymph drainage, and have the knowledge and techniques to practice it, regardless of formal qualification; and (c) use the therapy routinely or intend to use it.
3.2. Ethical Considerations
- Before the interview, we explained to informants the purpose of the study, the methods, and ethical considerations, after which they gave written consent. A withdrawal form was also distributed in advance for informants who might wish to leave the study after the interview. This study was approved by the Ethics Committee for the Faculty of Health Care and Nursing,Juntendo University.
3.3. Data Collection
- Method: Semi-structured interviews were conducted, during which informants’ statements were recorded with an IC recorder and transcribed later. Each interview lasted about 60 minutes. The interview questions, which were divided into two groups, are as follows:a. Personal experience of therapy effectivenessWhen did you get an opportunity to study these therapies?Why do you think these therapies should be introduced into nursing care?b. Howhave nursing care treatments been structured;how should they be structured?How do colleagues or other workers feel?Which areas do you think have been well implemented?Which areas do you think are not well implemented?
3.4. Analysis
- Our method was analytic induction.We classified the interview content based on the following factors: feasibility of implementation, results obtained from trial practice, and opportunities for introducing this therapy into nursing care.Then, we coded each person’s response. We then categorized it to detect any similarity between the codes.
4. Results
- The nurses who participated in this study are described as A, B, C, D, and E. The categories and subcategories are shown in [ ] and <>.
4.1. General Overviewof the Informants
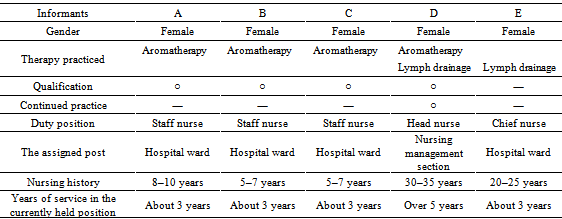
- The informants were five female nurses, consisting oftwo nurses who have job titles (chief nurse and head nurse) and three staff nurses. Only DusesCAM in routine work.Of the five nurses, only D has been regularly providing complementary therapies (Table 1).
|
4.2. Motivation for Learning CAM Therapy
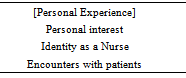
- The nurseswere motivated by their own [personal experience], which drove them to acquire the professional therapeutic knowledge, skills, and certification to practice in clinical settings. Table 2 shows the elements included in [personal experience].
|
4.3. Causes of Difficultiesin Regular Use ofCAM
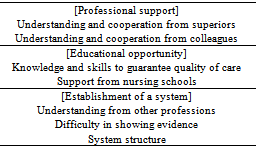
- Factors that encourage the use of complementary therapy in nursing practice were determined to be [professional support], [educational opportunity], and [establishment of a system] (Table 4).Regarding [professional support], informants stated that approval and support from a head nurse and nurses holding administrative positions greatly affected the implementation of complementary therapy in clinical settings, indicating the need of <understanding and support from the boss>. Informants C and D related their experiences concerning support:At the time, our head nurse said that he or she would love to cooperate, which was a great help. The nurse came to this ward because he or she wanted to practice aromatherapy...I thought about what I could do, and I wanted to take care of C andX, who were transferred here...They said that they wanted to convey the message that aromatherapy can be safely used in nursing care and that it was suitable for other staff to use in nursing care. (C)Regarding massage I provide for patients using essential oils, a physician once laughed at me, saying, “Is this a part of nursing care?” or “Is this something a nurse has to do?” At that time, our nurse manager stood up for me…(snip)…There may be many problems to overcome for a young nurse to adopt complementary therapy, but I think it is possible, by obtaining theunderstanding of a head nurse, to conduct it as a part of the hospital service, or negotiating with other physicians. (D)
|
4.4. Feelings Regarding Treatment Efficacy
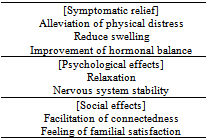
- Table 3 shows the effects of therapy identified from participants’ responses.
|
5. Discussion
- In this study, the informants were motivated by their [personal experience], which drove them to acquire professional knowledge of CAM to practice in clinical settings. However, no systematic and strategic approach was observed in the process of initiating complementary therapy. This may be one of the factors hampering the adoption of CAM.The first reason that nurses have difficulty in adoptinga systematic and strategic approach may be that the direct medical care provided must be based on physicians’ competence. CAM therapy sometimes infringes on a physician’s practice, depending on its purpose and the types of therapy. Therefore, in order to integrate CAM into nursing practice, it is essential to show strategically that complementary therapies are a part of nursing practice that does not infringe on areas of a physician’s practice.The informants in this study saw or experienced [symptomatic relief], [psychological effects], and [social effects] by means of complementary therapy. However, they also stated that [symptomatic relief] is generated only by [psychological effects] and [social effects]. Complementary autonomy between nurses and physicians was maintained by strategically confining the purpose of nursing practice to providing holistic care to patients. When roles and tasks overlapped among multiple health care providers, such strategic confinement was used to maintain relationships so that they could respect each other, implement their own tasks, and cooperate with other workers[12]. However, if complementary therapy does not threaten to infringe on other clinical areas of practice, a systematic and strategic approach may not be necessary for adopting CAM.The second reason is that nursing care involves “social action.” Within a structure, the concepts or interests of people who have administrative positions often influence the organizational aims. Informant A stated that the implementation of complementary therapy is possible if staff nurses assume that the use of aromatherapy is to achieve [symptomatic relief] or [psychological effects], even if
6. Conclusions
- The consent of the boss and cooperation of colleaguesare necessary for a nurse to use CAM as a common practice. In part, such cooperation is necessaryfor using CAM because of the time it takes;therefore, a particular time must be foundfor using CAM therapy. Study participants felt that CAM would need to be institutionalized so that it could be made a part of a nurse’s regular duties.Nurses’ use of CAM suggests the possibility of a medical change, though, and the science of nursing is beginning to promote it. Perhaps the evidence that is neededfor using CAM therapy safely will be produced through further studies.
ACKNOWLEDGEMENTS
- We would like to thank the nurses who participated in this study. This study was carried outin 2010-2011with the aid of the Collaborative Research Fund of the Faculty of Nursing and Medical Care.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-Text HTML
Full-Text HTML