-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2018; 6(4): 59-63
doi:10.5923/j.rog.20180604.01

Review of Cervical Screening in a Nigerian Tertiary Hospital
Egbodo CO1, Edugbe AE2, Akunaeziri AU3, Ayuba C.1, Oga EO4, Shambe HI1, Kahansim ML1, Ocheke AN1
1Department of Obstetrics and Gynaecology, Jos University Teaching Hospital, Jos, Plateau State, Nigeria
2Fertile Ground Specialist Hospital, Zaramanganda, Jos, Plateau State, Nigeria
3Department of Obstetrics & Gynaecology, Federal Medical Centre, Keffi, Nasarawa State, Nigeria
4Department of Obstetrics and Gynaecology, Dalhatu Araf Specialist Hospital, Lafia, Nasarawa State, Nigeria
Correspondence to: Oga EO, Department of Obstetrics and Gynaecology, Dalhatu Araf Specialist Hospital, Lafia, Nasarawa State, Nigeria.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

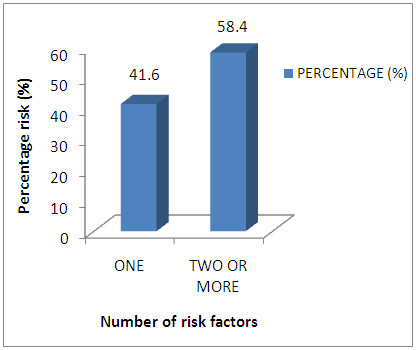
Background: Cervical cancer is the commonest gynaecological cancer in developing countries due to poor uptake of screening services. Objective: To determine the prevalence and pattern of abnormal Pap smears and the relationship of the abnormal smears with risk factors for the development of cervical cancers. Materials and Methods: Retrospective analysis of data from the cervical cancer screening centre of the Jos University Teaching Hospital (JUTH). Results: Of the 3875 women screened, 1418 (36.6%) had abnormal smears with low grade squamous intra-epithelial lesion (38.2%) being the commonest lesion. Among those with abnormal smears, 590 (41.6%) had one risk factor each and 828 (58.4%) had two or more risk factors while those women who were 50 years and above constituted the highest number with abnormal smears. Conclusion: This study showed that only few women access cervical screening services and amongst those who accessed the services, a large proportion had abnormal smears. Also, the likelihood of having abnormal cervical smears increased with the number of risk factors and advancing age. There should therefore be more awareness campaigns and cervical screening services should be made accessible and affordable for all women.
Keywords: Cervical screening, Cancer, Abnormal smears
Cite this paper: Egbodo CO, Edugbe AE, Akunaeziri AU, Ayuba C., Oga EO, Shambe HI, Kahansim ML, Ocheke AN, Review of Cervical Screening in a Nigerian Tertiary Hospital, Research in Obstetrics and Gynecology, Vol. 6 No. 4, 2018, pp. 59-63. doi: 10.5923/j.rog.20180604.01.
1. Introduction
- Available evidence indicates that cervical cancer is the second most common cancer in women worldwide and it is responsible for about 12% of cancers in women [1, 2]. However, in developing countries it is the commonest cancer [1]. In Nigeria the estimated incidence rate of cervical cancer is 25/100,000 women, with an estimated 8000 new cases of cervical cancer diagnosed in the country each year [2, 3]. Worldwide about half (½) a million new cases are diagnosed each year with more than one-quarter (¼) million deaths each year, yet cervical cancer is both preventable and curable [3].Developed countries have been successful in controlling the incidence of invasive carcinoma of the cervix, whereas low income countries have failed dismally in this respect [2, 4]. The success of the developed countries is largely attributed to the widespread and systematic use of the Pap smear. In Sweden, for example, more than 80% of women are regularly screened. In contrast, less than 1% of women have ever been screened in any developing country [3].George Nicholas Papanicolaou (1883-1962) laid the original foundation for the prevention of cervical carcinoma over half (½) a century ago when he described a cytological method for the detection of pre-invasive lesions popularly referred to as the Pap smear test [3-6]. Since then other screening methods have been described but the Pap smear test remains an effective approach to cervical cancer screening worldwide [2, 7-9]. These newer methods include human papilloma virus (HPV) DNA testing, Cervicography, speculoscopy, polar probe, visual inspection (aided and unaided), computer based screening techniques like papnet, autopap and autocyte screen [4, 10-16]. To date, cervical cancer screening and Pap smear that have significantly reduced the rates of cervical cancer in high and middle income countries are still poorly applied in Africa [2]. Part of the low acceptance of secondary prevention services for cervical cancer in Africa include the lack of awareness of cervical cancer and the role of screening, inappropriate health seeking behaviour of women, poor organization of health services, low priority accorded to women’s health by policy makers and high cost of screening. Screening programs in most developing countries remain opportunistic and on a small scale [3-5]. We therefore sought to determine the number of women who access cervical screening services at the Jos University Teaching Hospital, the prevalence and pattern of abnormal Pap smear and the relationship between abnormal Pap smear results and the risk factors for cervical cancer in these women.
2. Materials and Methods
- A retrospective review of data obtained in the cervical cancer screening centre of Jos University Teaching Hospital from 1st January 2012 to 31st December 2013 was done having obtained ethical clearance from the institutional ethical committee. Information such as age, marital status, sexual history, cigarette smoking, use of oral contraceptive pills, parity, previous history of sexually transmitted infections and the cytology results were retrieved. The data was analyzed using Epi Info 3.5.2 version of 2010.
3. Results
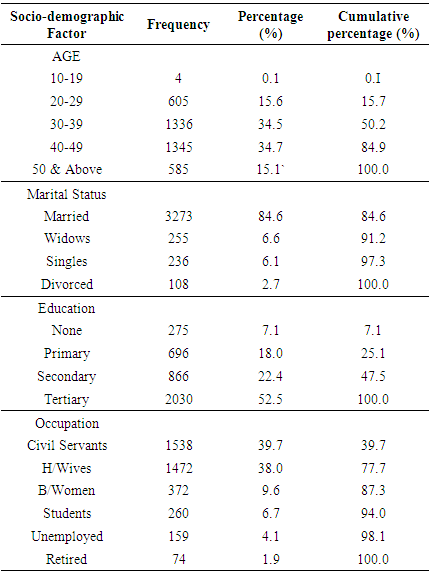
- During the study period, there were 3875 women who presented at the Jos University Teaching Hospital Cervical Cancer Screening Unit and were screened. The frequency distribution of the socio-demographic status of the patients screened is shown in table 1 below.
|
|
|
 | Figure 1 |
|
4. Discussion
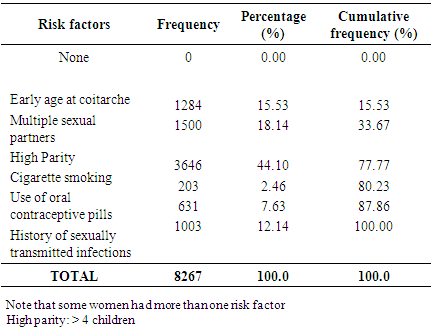
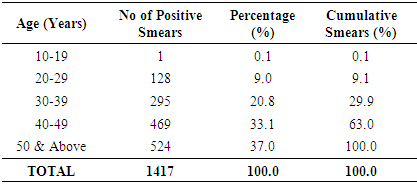
- This study was carried out in Jos University Teaching Hospital (JUTH) to determine the pattern of abnormal Pap smears in women screened in the cervical cancer screening centre within a period of 2 years. Within this period, 1547 women were screened in 2012 and 2328 were screened in 2013 giving a total of 3875 women screened. The increased number of 2013 over 2012 could be attributed to the increasing awareness of the existence of the centre in JUTH.It was observed that majority of the women were in the age range of 40-49 years (34.7%) closely followed by the age range of 30-39 years (34.5%). Only 0.1% of the women were below 20 years of age which showed a significant difference from a study by Khattack et al in which 38% of women screened were below the age of 20 and 62% were above this age [9]. It was also observed that more than half of the women screened within this period had tertiary education (52.5%) and 22.5% had secondary education. This further emphasizes the role of education in the control of cervical cancer [1, 2, 7]. Those with no formal education were those mostly referred from the gynaecological clinic where they were on follow up for other conditions. All the women screened had at least one risk factor for the development of cervical cancer. Multiple epidemiological studies in literature had shown an association between cervical cancer and multiple independent risk factors [10-12]. The risk factors assessed in this study were socio-economic status, cigarette smoking, previous history of sexually transmitted diseases, multiple sexual partners, early age at first intercourse before 20 years of age, parity and use of combined oral contraceptive pills [1, 3, 4, 15]. The cytology results showed that 2454 (63.4%) of the women whose results were assessed had negative smears while 1417 (36.6%) had positive smear which was similar to the one obtained by Khattack et al in which 61.6% and 38.4% had negative and positive smears respectively [9]. However, this was significantly different from the results obtained by Leeson in which 85.0% of the smears were negative [1]. This could be due to differences in geographical location and sample size. The pattern of the abnormal smears showed that 38.2% had low grade squamous intra-epithelial lesions (LSIL) and 25.5% had high grade squamous intra-epithelial lesions (HSIL). The least were those of suspected infiltrative cancers (2.3%). These results vary significantly with an earlier study in Enugu, Nigeria where 14.1% of the patients had suspected invasive cancers [3]. However, there was marked difference in the sample size which could be responsible for this wide difference. Also, 13.9% of the women with abnormal smears were grouped as others which included inflammatory cells, yeast cells and inadequate smears. The prevalence of HSIL in South Africa was found to be 2.5% and those of infiltrating cancers was 0.5% and in a study in Taiwan the prevalence of LSIL was 38%, HSIL was 36%, invasive cancer was 1.0% [4, 10]. Even though there was significant difference between the South Africa study and this one there is similarity between this study and the later from Taiwan. The Taiwan study by the Taiwan Cooperative Oncology Group (TCOG) had a higher sample size and was carried out over a period of 5 years [10].The number of women with abnormal smears were observed to increase with increasing number of risk factor as those with abnormal smears and one risk factor each were 589 (41.6%) while those with abnormal smears and two or more risk factors were 828 (58.4%). This further strengthens the effect of multiple risk factors in the development of cervical cancers [10, 11]. The abnormal smears were also observed to increase with advanced age. Those in the age group of 50 years and above had the highest number of abnormal smears as 524 (37.0%) of them had positive smears and this number represents 89.2% of the total women in the age group. This agrees with earlier studies which showed this pattern [1, 9, 17, 18]. In this study it was also observed that good education, high socio-economic status as well as young age had positive influences on cervical screening in this centre. This showed that women who are less likely to be reached by a screening program are those that are older, poorer, less educated and unemployed or are working in the non-formal sector [4]. In JUTH, patients with single abnormal Pap smear are evaluated and treated for potential underlying conditions like infection or atrophic vaginitis before repeat cytology 3 to 6 months later. If changes persist, they are then referred for colposcopy. If colposcopy is abnormal, management is based on colposcopy findings, age of the patient, reproductive wishes of the patient, presence of other gynaecological conditions and likelihood of compliance with management. Patients with ASCUS, ASC-H and LSIL are managed expectantly with cervical cytology smear every 3 months. Patients with CIN II and CIN III are offered any of the following: cold knife conization, large loop excision of the transformation zone (LEETZ) or hysterectomy (for those with completed family size). Patients with invasive cancer following colposcopy are treated with either radical surgery, radiotherapy (with or without chemotherapy) or combined surgery and radiotherapy.This study showed that the relationship between premalignant lesions of the cervix and multiple independent risk factors cannot be over emphasized as abnormal smears were more in those with multiple risk factors. Also, a large proportion of women screened had positive smears which further emphasize the need for more screening centres in order to pick those cases early when cure is still possible. It is therefore imperative to set up more screening centres for cervical cancers by the government as well as non-governmental organizations involved in the campaign against cervical cancers. The low level of turn out for screening among those women of low socio-economic status and low education may be related to the cost of screening. More women may turn up for screening if this is made affordable and accessible with more screening centres established especially in the primary health care centres where a significant number of women seek health care services. The limitations of this study include that it was a retrospective study with its attendant setbacks and that this was a tertiary hospital based study and therefore the results may not reflect the findings in the general population.
5. Conclusions
- This study showed that only few women access cervical screening services and amongst those who accessed the services, a large proportion had abnormal smears. Also, the likelihood of having abnormal cervical smears increased with the number of risk factors and advancing age. There should therefore be more awareness campaigns by health workers, government and non-governmental organizations to increase the uptake of cervical cancer screening. Cervical screening services should be made accessible and affordable for all women.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML