-
Paper Information
- Next Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2018; 6(3): 47-51
doi:10.5923/j.rog.20180603.02

Instrumental Vaginal Delivery at Jos University Teaching Hospital (Juth): Forceps Versus Vacuum Extraction, a Four Year Retrospective Review
Egbodo CO1, Edugbe AE2, Akunaeziri AU3, Ayuba C.1, Oga EO4, Shambe HI1, Kahansim ML1, Ocheke AN1
1Department of Obstetrics and Gynaecology, Jos University Teaching Hospital, Jos, Plateau State, Nigeria
2Fertile Ground Specialist Hospital, Zaramanganda, Jos, Plateau State, Nigeria
3Department of Obstetrics & Gynaecology, Federal Medical Centre, Keffi, Nasarawa State, Nigeria
4Department of Obstetrics and Gynaecology, Dalhatu Araf Specialist Hospital, Lafia, Nasarawa State, Nigeria
Correspondence to: Oga EO, Department of Obstetrics and Gynaecology, Dalhatu Araf Specialist Hospital, Lafia, Nasarawa State, Nigeria.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

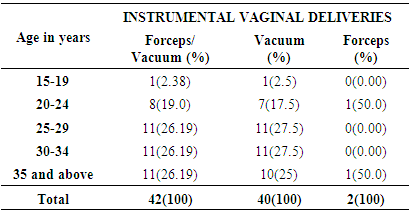
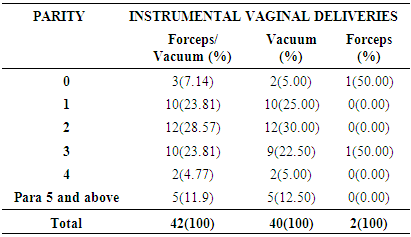
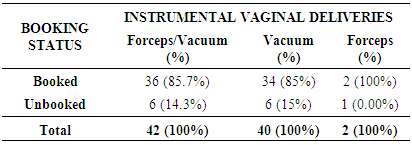
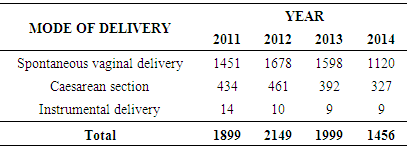
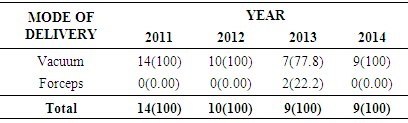
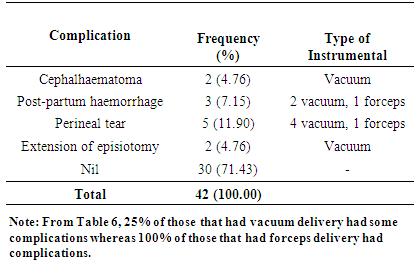
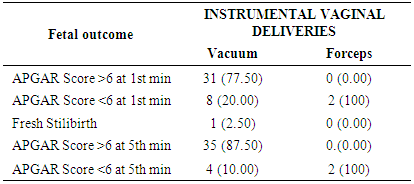
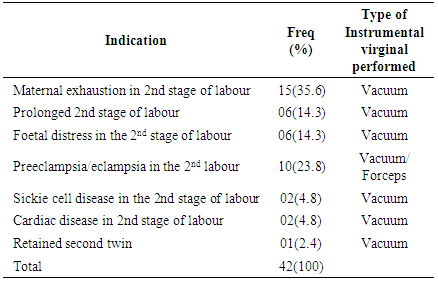
Background: Instrumental vaginal delivery, either with forceps or vacuum-assisted, is used to facilitate childbirth and to avoid caesarean section delivery (CS) and its associated morbidities. Nevertheless, instrumental techniques are associated with a greater tendency for birth injury than spontaneous delivery. There is a need to maintain and improve the skills for this procedure through training and research in order to improve the benefits for both mothers and their babies. Objectives: 1. To determine and compare the incidence of vacuum versus forceps. 2. Indications of instrumental vaginal delivery. 3. Compare the foetal and maternal outcome of vacuum and forceps deliveries. Materials and Methods: This was a retrospective review on instrumental vaginal deliveries (vacuum extraction and forceps delivery) carried out between 1st January 2011 and 31st December 2014. The hospital records of all the patients who had vacuum or forceps delivery were obtained and data on age, parity, booking status, and type of procedure performed, APGAR scores of babies delivered and complications were entered into a proforma and analyzed using SPSS software for Windows version 16.0. Results: During this study period, there were 7,503 deliveries out of which 42 (0.56%) were instrumental deliveries. The rates were 0.53% and 0.03% for vacuum and forceps deliveries respectively. Unbooked patients were 6 (14.3%) while 36 (85.7%) were booked. The commonest indication was material exhaustion (35.6%). Mean birth weight of babies were 3091.84g. The perinatal outcome showed that 77.5% had Apgar scores of 7 and above at one minute. This was increased to 87.5% at the 5th min. the mean blood loss was 310mls. Thirty of the mothers were free of complications. The commonest complication was perineal tear ac-counting for 11.9%. Conclusion: The rate of instrumental vaginal deliveries in this institution is low and indications for the procedure are similar to those found elsewhere. It is also evident from this studies that forceps delivery is a dying saving art as compared to vacuum delivery, therefore, obstetricians should be trained properly so as to optimize their benefit. There is significant difference in terms of foetal and maternal outcomes between those who had forceps delivery and those who had vacuum delivery.
Keywords: Instrumental vaginal delivery, Vacuum and Forceps deliveries, Jos, Nigeria
Cite this paper: Egbodo CO, Edugbe AE, Akunaeziri AU, Ayuba C., Oga EO, Shambe HI, Kahansim ML, Ocheke AN, Instrumental Vaginal Delivery at Jos University Teaching Hospital (Juth): Forceps Versus Vacuum Extraction, a Four Year Retrospective Review, Research in Obstetrics and Gynecology, Vol. 6 No. 3, 2018, pp. 47-51. doi: 10.5923/j.rog.20180603.02.
1. Introduction
- Instrumental vaginal delivery is defined as vaginal delivery accomplished with the aid of instruments which can be vacuum or forceps. [1] it is carried out in the material interest, foetal interest or both. It is a procedure with a long history spanning more than two centuries and had undergone modifications and refinement to the present day. [2]The frequency of instrumental vaginal delivery varies from one country to another, and even in the same country, from one obstetric unit to another. The instrumental delivery (ID) rate thus varies greatly between settings and the ideal rate is unknown [2]. In the Royal College of Obstetricians and Gynaecologist (RCOG) Consultants Conference, operative vaginal delivery rate of 10.5% was reported with a range of 4-20%. The consensus at the conference was to aim lower the rate to an average of 8.5% in the Untied States [2]. In low resource countries IVD should provide a good alternative for delivery. However IVDs are underused in low resource settings [2]. Rate of IVD are low, ranging from 1% or less in Niamey (Niger), Ougadaougou (Burkina Faso) and Bamako (Mail) to 3# in Nouakchott (Mauritania) [4]. In contemporary practice however, there are conflicting reports on the trend in the general rate of instrumental vaginal delivery. Where-are in the US a decline has been reported5 a relatively constant rate is reported in some countries such as Scotland and Australia [6]. Data on IVD rates are scanty in Nigeria. Most studies were done on forceps delivery and its rate ranged from 0.9% to 6% [7]. IVD constitutes 3.6% of all deliveries at the Ahmadu Bello University Teaching Hospital in Zaria [8]. The current rate of forceps delivery in Ibadan is 1.57% [9]. Vacuum delivery rate of 1.5%, 1.6%, 1.7% were reported from Enugu, Ile-Ife and IIorin respectively [10-12]. The choice of which instrument to use varies from locality and depends on the perception of practitioners on the relative safety of the instruments and their experiences. In some areas it depends on the availability of the instruments and the skill of the attending doctor. In other areas such as the USA, legal issues also determine the choice of instrument. In general, African obstetricians have shown more interest in the use of vacuum extraction over forceps [4]. In the USA the vacuum is the instrument of choice [13, 14]. Whereas the forceps is the preferred instrument in Eastern Europe and South America [15].Studies have compared neonatal complications between vacuum and forceps, and they showed that neonatal complications were more with vacuum whereas maternal complications were more with forceps. A study form Pakistan showed no significant difference in the APGAR score at 5 minutes in forceps and vacuum deliveries [16, 17]. This is supported by the Cochrane systematic review of nine randomized controlled studies that showed that vacuum extractor is no more likely to be associated with low APGAR score at 5 minutes when compared to forceps [18]. However, some other non-randomized controlled studies showed that material complications were more with forceps [16, 19].According to the WHO and other UN agencies, assisted vaginal delivery is one of the six critical functions of basic emergency obstetric care [20]. This means that IVDs are such vital procedures and should be made available and accessible everywhere especially in developing countries where the need is high and caesarean section as alternative is not always available. Broadly speaking, the traditional indications for vacuum extraction are delayed labour, distress on the part of the baby or mother and medical conditions requiring shortening of the second stage of labour [10, 16, 21]. The indications abound, the benefits such as reduction in caesarean section rate, reduction in the cost of delivery and brighter obstetric future are obvious hence the need for more studies in this area to provide practitioners with more information on this procedures to improve its utilization and safety.In order to determine the incidence and indications of IVD at Jos University Teaching Hospital, Jos, Nigeria and to compare the foetal and maternal outcomes of vacuum and forceps deliveries we studied the outcomes of the procedures over a four year period.
2. Materials and Methods
- This was a retrospective study carried out on all patients that had IVD between 1st January 2011 and 31st December 2014. Data were obtained from the hospital records which included the age, parity, booking status, and type of procedure performed, the APGAR scores of the babies and complications in the parturient. The data were analyzed for significance using SPSS software for Windows version 16.0.
3. Results
|
|
|
|
|
|
|
|
4. Discussion
- The overall rate of instrumental delivery (IVD) in this study was 0.56%. The rate of vacuum delivery was 0.53% while the rate of forceps delivery was 0.03%. The low rates was attributed to lack of experienced personnel to carry out the procedure and incomplete delivery documentations. The overall rate is similar to what was reported from other developing countries in West Africa such as Niger, Burkina Faso, and Mali [4]. It is however lower than 3% reported from Nouakchott which may be due to a better health care delivery system compared to what we have in our environment [4]. It is much lower than 3.6% reported from Zaria in Nigeria [8]. It is also very much lower than 8.5% recommended by RCOG [3] and also lower than what is reported from developed countries [2]. The rate of forceps delivery in this study is far lower than 1.57% reported from Ibadan Nigeria [9] with better facilities and more experienced personnel. The vacuum delivery rate is also lower than what is reported elsewhere [10-12].Vacuum is far more commonly used than forceps in this study which in conformity with the reported trend in Africa4. In the US the instrument of choice is the vacuum [13, 14]. The choice of the vacuum for IVD in Africa may be because of simplicity of use and the ease with which the skill to use it is acquired. These may be the same factors which made vacuum the most commonly used instrument in our centre. In the US however legal issues also play a role in determining the choice of which instrument to use for IVD. In North America, forceps has generally been used more frequently than vacuum extraction, whereas the reverse is true in Europe [3]. However, recent developments may have influenced practitioners’ decisions concerning these methods. Meta-analyses of randomized trials comparing maternal and infant outcome between vacuum extraction and forceps deliveries have found that vacuum extraction causes less maternal trauma [15]. Vacuum extraction has also recently gained popularity because of new designs of vacuum cups, presumably with reduced risk of injury to the infant [15].It is obvious from this study that forceps delivery is on the declining trend compared with vacuum delivery probably as a result of disappearing art on how to perform forceps delivery and also fear of possible complications that may arise. In support of this study is the fact that only 25% of those that had vacuum delivery had complications whereas 100% of those that had forceps delivery had complications, even though the numbers of those that had forceps delivery overall were only 2 as against 40 that had vacuum extraction and therefore may not be feasible to draw conclusion. It must be emphasized that forceps delivery cannot be substituted with vacuum extraction considering the fact that medical conditions in pregnancy such as cardiac disease and sickie cell disease to mention a few will benefit better with the use of forceps to shortened the second stage of labour and non involvement of material effort. [15, 16]There was significant difference between forceps and vacuum deliveries in terms of the number of babies delivered with asphyxia i.e APGAR score of 6 or less. This means babies delivered by vacuum have better APGAR scores compared to those delivered by forceps as is evidenced in this study with all the two forceps delivery resulting in asphyxiated babies. A study elsewhere [16, 17] revealed no significant difference and the finding was corroborated by a Cochrane systematic review of nine randomized controlled study [18]. This study also showed that there was a significant difference in material complications between women delivered by forceps when compared to those delivered by vacuum. Those delivered by vacuum sustained less complications (25%) as against 100% for forceps delivery. This is similar to what was reported elsewhere by other workers [16, 19]. Because of the number of those that had forceps delivery in this study as compared to vacuum extraction conclusion thus not be drawn.It was found that there was no significant difference between those delivered by forceps and those delivered by vacuum with respect to their booking status. This is contrary to our expectations, because those who were booked would have been more psychologically prepared and would have been screened for conditions that result in indication for IVD when compared to those who were booked. Parity of women seemed not have determined which instrument was used in carrying out IVD in this study as there was no significant difference between those who had forceps and those who had vacuum with respect to parity. This was also contrary to our expectation, because women of lower parity are more prone to exhaustion, uterine inertia and other conditions that require performing an IVD compared to those with high parity who are more experienced and have more efficient uteri.The indications for IVDs in this study were similar to those reported elsewhere [10, 16, 21]. Material exhaustion in the second stage of labour appear to be taking the lead position for indications and accounted for 35.6%.This study was retrospective and will therefore be limited by factors that are known to influence the strength of retrospective studies which includes, some patients case note could not be retrieved, records on case notes were inadequate, some cases were not documented, and it was a hospital based study and not representative of the general population.The low rate IVDs especially forceps should be improved by training our residents in training on those procedures. Proper and complete documentation of IVDS performed. It is paramount to note also that most of the medical conditions in which maternal effort is not needed should implore the use of forceps, and hence the need to improve on training residence on forceps delivery. Long term effects such as neurological deficits and intelligent quotients of infants and long term complications in mothers will highlight the safety of these procedures as carried out at our centre and these inform the need for a prospective study on this topic.
5. Conclusions
- The rate of instrumental vaginal deliveries in this institution is low and indications for the procedure are similar to those found elsewhere. It is also evident form this studies that forceps delivery is a dying saving art as compared to vacuum delivery, obstetricians should be trained properly so as to optimize their benefits. There is significant difference in foetal and material outcomes in those who had forceps delivery when compared with those who had vacuum delivery.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML