-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2018; 6(2): 37-40
doi:10.5923/j.rog.20180602.03

The Value of Absence or Reversed of End Diastolic Flow Velocity in Umbilical Artery in Predicting Fetal Distress and Intrauterine Grow Restriction in Preeclampsia
Tran Danh Cuong1, Pham Thi Mai Anh2, Nguyen Thi Mai Phuong3, Phan Truong Duyet1
1Hanoi Medical University, Vietnam
2Haiphong Hospital of Obstetrics and Gynecology, Vietnam
3Haiphong University of Medicine and Pharmacy, Vietnam
Correspondence to: Tran Danh Cuong, Hanoi Medical University, Vietnam.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

The cross-sectional study among 484 patients who were diagnosed with pre-eclampsia at National Hospital of Gynecology and Obstetrics and Haiphong provincial hospital of Obstetrics and Gynecology from September 2013 to December 2016. Objective: The study evaluates the value of absence or reversed of end-diastolic flow velocity in the umbilical artery in a prediction of fetal distress and intrauterine grow restriction in preeclampsia. Results: The incidence of fetal distress and intrauterine grow restriction in case of absence of end diastolic flow in the umbilical artery is 96.3%, in case of reversed of end diastolic flow is 100%. Conclusion: Absence of end-diastolic flow velocity or reverse flow in umbilical artery is a negative predictor of perinatal outcomes.
Keywords: Pre-eclampsia, Doppler umbilical artery, Absence of end-diastolic flow velocity, Reverse flow
Cite this paper: Tran Danh Cuong, Pham Thi Mai Anh, Nguyen Thi Mai Phuong, Phan Truong Duyet, The Value of Absence or Reversed of End Diastolic Flow Velocity in Umbilical Artery in Predicting Fetal Distress and Intrauterine Grow Restriction in Preeclampsia, Research in Obstetrics and Gynecology, Vol. 6 No. 2, 2018, pp. 37-40. doi: 10.5923/j.rog.20180602.03.
Article Outline
1. Introduction
- Pre-eclampsia (PE) is a disorder of pregnancy characterized by the onset of high blood pressure and a significant amount of protein found in the urine. Pre-eclampsia usually begins after 20 weeks of pregnancy in women whose blood pressure had been being normal. Once it occurs earlier, it is associated with worse maternal and fetal complications. It is one of the leading causes of maternal and perinatal mortality and morbidity worldwide. However, the pathogenesis of pre-eclampsia is partially understood but the well-known outcome is that the disease will be reduced immediately if the fetus and the placenta are removed from the mother. Therefore, PE is considered a global health problem. The objectives of this biggest organization is to develop the early diagnosis and available treatment of PE at 1st trimester prenatal care and to evaluate the efficacy of methods of prevention for PE’s complication. One of the most available methods is Doppler ultrasound of umbilical artery. That’s the reason why we conducted this study with the aims to evaluate the value of absence or reversed of end-diastolic flow velocity in umbilical artery in the prediction of fetal distress and intrauterine grow restriction in patients with pre-eclampsia.
2. Subject
2.1. Studied Population
- The pre-eclampsia women and their babies diagnosed and treated at National hospital of Obstetrics and Gynecology and at Haiphong provincial hospital of Obstetrics and Gynecology from September 2013 to December 2016. There were 484 patients who were eligible for our study in the studied period. Inclusion criteria Patients who had satisfied following symptoms had been recruited for our study: • ≥ 28 weeks gestational age, • One fetus• Live fetus• Oedema• Diastolic tension ≥ 140 mmHg, systolic tension ≥ 90 mmHg • Level of proteinuria ≥ 0,3 g/l (at 24-hour urine protein test) or ≥ 0,5g/l (at random point).Exclusion criteriaMultiple pregnancies, malformation fetus, maternal history: cardiac distress, renal distress, diabetes.
2.2. Main Outcomes, Definitions, and Data Analysis
- Pregnant women provided following basic information: • Antenatal information: name, age, occupations, number of pregnancies, arterial pressure, level of oedema.• Blood chemistry test for evaluation of liver and kidney function. Complete blood count for evaluation of number of red blood cells, white blood cells, platelets. Basic coagulation test.• Assessment of level of proteinuria for classification of PE.• Doppler ultrasound of umbilical artery to determine its pattern within 24 hours before termination of pregnancy.• Postnatal: fetal age, birth weight, Apgar score, colour of amniotic fluid.Pre-eclampsia diagnosis criteria Diagnosis and classification of PE and severe PE (WHO, 2011) [1]. Evaluation of fetal distress: A fetus is considered as a fetal distress if it has one of this two postnatal signs below [2]:• Apgar score at 1 minute after birth < 7.• Meconium in amniotic fluid.• Evaluation of intrauterine growth restriction: if his/her birth weight less than the 10th percentile following Phan Truong Duyet (2005). Evaluation of Doppler of umbilical artery: in this study, we researched the morphology of these below [3]: • Absence of end diastolic flow velocity (AEDF): The umbilical arterial velocity is seen reducing to zero at end diastole.• Reversal of umbilical artery end-diastolic flow (REDF): a low wall filter setting (<100 Mhz) and an acute insonation angle of <30% is recommended.Data analysisBy SPSS 16.0, evaluate the value of Doppler ultraound of umbilical artery in predicting of fetal distress and intrauterine growth restriction by calculating the percentages and by comparing the differences between these percentages by Chi-square test.
2.3. Ethical Approval
- Ultrasound is actually presumed to be safe in prenatal settings. It did not waste time or money of the patients in ultrasound. This study was approved by the Ethical Committee of National Hospital of Obstetrics and Gynecology. Participants were informed of the study purpose and were asked to give a written informed consent to confirm their participation. Participants could withdraw anytime and their information was kept confidentially.
3. Results
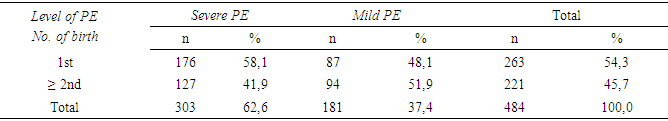
- The prevalence of severe PE is 62.6%, among that 58.1% is nulliparous mothers and 49.1% is multiparous ones. Oppositely, the rate of mild PE in nulliparous mother is 48.1%, is less than that of the multiparous mother (Table 1).
|
|
|
4. Conclusions
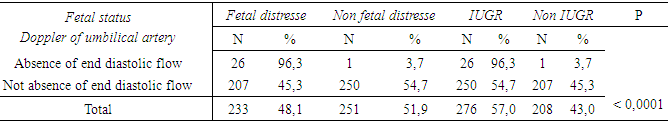
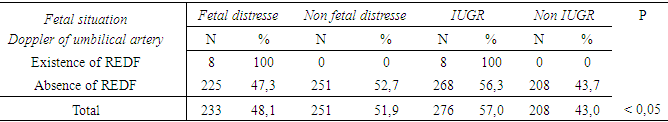
- According to table 1, the incidence of the 1st pregnancy in PE is 54.3% which is higher than the 2nd and over (45.7%). The prevalence of severe PE in the women who gave birth for the 1st time is higher than in the one for the 2nd and over (58.1% and 49.1%, respectively). The explanation may be based on the hypothesis about the immune response in the pathology of PE that it is more common and usually worse at the first exposure of fetal antigens from the follicle cells. Therefore, systematical immuno-activation may be one cause of preeclampsia.In our study, in 27 patients of the absence of end-diastolic flow velocity in fetus, there are twenty-six cases (97.3%) had distress fetal and also IUGR, just only one normal infant was. It is found in our study that 100% of reversal of umbilical artery end-diastolic flow was fetal distress and IUGR (8/8 patients).This result is equivalent to other studies [4-6]. Overall, the incidence of fetal distress in case of absence of reversed of end diastolic flow velocity is 83.3%, of disorder of acid-base balance in the newborn is 88.0%, of neonatal respiratory distress is 53.0%, of malnutrition is 98.0% and of IUGR is 25.0%.In the study of Nicolaides et al, they determined blood gas of umbilical blood in 59 cases of IUGR within the Doppler ultrasound of umbilical artery (the middle cerebral artery to umbilical artery resistance index ratio = 1). The results indicated that 88% of this test had abnormal blood gas, 42% of this test had a low blood oxygen level, 37% of these infants had asphyxia and 9% of these infants had metabolic acidosis [7].Karsdrop (1994) also reported that in 245 cases of the absence of reversed of end-diastolic flow velocity in fetus, the incidence of perinatal mortality is 28% and 96-98% of this infants need to be admitted to the Neonatal Intensive Care Unit [8].Maulik D & al conducted a study including 1,126 cases of absence of reversed of end diastolic flow velocity, the incidence of stillbirth is 17%, of perinatal mortality is 28% and most of this is caused by complications such as neonatal respiratory distress, IUGR, premature birth or congenital anomaly [9].Futhermore, the study of Khushali Granhi et al. in 2015 in 100 IUGRs, there were eight patients has absence of reversed of end-diastolic flow velocity in fetus and the incidence of stillbirth and perinatal mortality is 50%, that is similar to the results of Battaglia (1993) [10, 11].According to Dao Thi Hoa (2016), 62.5% of absence of reversed of end diastolic flow velocity was fetal distress and the umbilical blood pH of the newborn ≤ 7,15 [12]. Therefore, all these studies have shown that Doppler ultrasound of umbilical artery is the best predictive positive value for predicting fetal distress. The most typically abnormal Doppler of umbilical artery is absence of reversed of end diastolic flow velocity and it is a negative sign of fetal prognosis. This may be due to the reversal of umbilical artery end-diastolic flow just occurs in severe fetal distress which has serious circulatory disorders that end of some of the diastolic flow along the blood wall, and it also has a severe effect on the fetal heartbeat and leads to impaired cardiac activity. Increased flow through the tricuspid valve and through the pulmonary artery, reduced flow through the mitral valve, so it damages the left ventricular function and leads to congestive heart failure. In this study, the incidence of fetal distress and C-section is so high about 75% and about 32.3%-41.0% of this newborn resulted in perinatal death [4]. Others authors confirmed also that absence of reversed of end diastolic flow velocity is the worst prediction for the fetus and it often occurs at the late period of pregnancy [13]. Numbers of studies were conducted to determine the duration from the appearance of the pathologic Doppler ultrasound of umbilical artery to the certain signs of fetal distress but they were almost unsuccessful because such signs last from several hours to several weeks and maximum nine weeks.
5. Conclusions
- The absence of end-disastolic flow velocity in fetus, especially reversal of umbilical artery end-disastolic flow is a bad predition sign for the fetus. The prevalence of fetal distress and intrauterine grow restriction is 100% in case of reversal of umbilical artery end-disastolic flow and it is 96.3% in case of absence of end-disastolic flow velocity in fetus.
ACKNOWLEDGMENTS
- We would like to thank the participants for their cooperation and the medical staffs from the Vietnam National Hospital of Obstetrics and Gynecology and Haiphong provincial hospital of Obstetrics and Gynecology who gave valuable support to this study.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML