-
Paper Information
- Previous Paper
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2018; 6(1): 16-21
doi:10.5923/j.rog.20180601.03

Knowledge of Obstetric Danger Signs among Pregnant Women Attending Antenatal Care Clinic at Health Facilities within Bureti Sub-County of Kericho County, Kenya
Omari K. Phanice1, Masimba O. Zachary2
1Department Environmental Health Sciences, University of Kabianga, Kericho, Kenya
2Department Health Services, Baringo, Eldama Ravine, Kenya
Correspondence to: Omari K. Phanice, Department Environmental Health Sciences, University of Kabianga, Kericho, Kenya.
| Email: |  |
Copyright © 2018 The Author(s). Published by Scientific & Academic Publishing.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

Knowledge of obstetric danger signs is the first step towards seeking appropriate obstetric care. Although women’s knowledge of obstetric danger signs is essential in the reduction of maternal and child mortality, little is known about the level of maternal knowledge of the obstetric danger signs and its associated factors among women in the rural Kenya. Thus, the aim of this study was to assess the level of knowledge of obstetric danger signs and associated factors among pregnant women attending antenatal care clinics in Bureti Sub-County of Kericho County, Kenya. A facility based, cross-sectional study was carried out from November 2014 to January 2015 among pregnant women attending health facilities within Bureti Sub-County. An exit interview was conducted using a semi-structured questionnaire that had been pre-tested. Collected data was analyzed using SPSS (v16). Descriptive data was summarized using frequencies and percentages whereas Chi squared test was used to determine association between socio-demographic factors and knowledge of obstetric danger signs. All tests were 2 sided and considered statistically significant at p<0.05. The age of respondents ranged between 18 - 43 years. Only 4.7% of the respondents were knowledgeable about obstetric danger signs. Vaginal bleeding was the most mentioned obstetric danger sign during pregnancy (55%), at birth (32.9%) and after delivery (37.6%). There was a declining trend in the proportion of women who were knowledgeable about obstetric danger signs in pregnancy (34.2%), at birth (14.1%), and postpartum (10.1%). Trimester of initiating antenatal care clinic was significantly associated with knowledge of obstetric danger signs (p=0.027); however, age, level of education; parity and marital status were not associated. Knowledge of women about obstetric danger signs was low. There is need for sensitization campaigns to raise awareness on obstetric danger signs organized at community level and in hospitals so as to reach all women irrespective of their social- demographic characteristics.
Keywords: Knowledge, Pregnant, Birth, Postpartum, Obstetric danger signs
Cite this paper: Omari K. Phanice, Masimba O. Zachary, Knowledge of Obstetric Danger Signs among Pregnant Women Attending Antenatal Care Clinic at Health Facilities within Bureti Sub-County of Kericho County, Kenya, Research in Obstetrics and Gynecology, Vol. 6 No. 1, 2018, pp. 16-21. doi: 10.5923/j.rog.20180601.03.
Article Outline
1. Introduction
- Pregnancy is a natural process in which non predictable complications can occur, maternal deaths from preventable causes remain a public health challenge particularly in developing countries. Every day, 830 women die from pregnancy or childbirth-related complications around the world, this amount to 287,000 women yearly and obstetric complications accounts for 75% of all these deaths [1, 2]. Most of these deaths (99%) occur in developing countries, with a greater portion occurring within the Sub-Saharan Africa region [3]. According to the Kenya Demographic and Health Survey of the year 2014, maternal mortality rate is estimated to be 362 deaths per 100,000 live births [4]. There are two causes of maternal deaths i.e. direct obstetric deaths which accounts for 72% of all the deaths and indirect obstetric deaths. Direct obstetric deaths are caused by complications related to pregnancy, delivery and postpartum period; while an indirect obstetric death is caused by pre-existing medical conditions that are made worse by pregnancy or delivery [5]. The medical causes of direct obstetric maternal death include: hemorrhage 28%; complications of unsafe abortion 19%; pregnancy-induced hypertension 17%; infection 11%; and Obstructed labor 11% [1, 5].Knowledge of danger signs during pregnancy, childbirth and the postpartum may improve timely recognition of these signs, a vital step towards addressing the delay in deciding to seek care and delay in reaching health care facilities [6, 7]. Therefore, a considerable number of cases of maternal morbidity and mortality could be prevented. Thus, one of the key strategies for reducing maternal deaths is increasing the knowledge on obstetric danger signs among women, their families and the community. In Kenya, a country where maternal morbidity and mortality is high, there is limited documented evidence on knowledge level of pregnant women on danger signs. The study aimed to fill this gap by assessing pregnant women's knowledge about obstetric danger signs in Bureti Sub-county of Kericho County, Kenya. The findings of this study will add to the evidence base required by public health policy makers in planning, designing and implementing suitable interventions and approaches to raise women’s knowledge on obstetric danger signs.
2. Methods
- The study was part of a larger study investigating birth preparedness and complication readiness among Ante Natal Clinic attendees in Bureti sub county of Kericho county, carried out between November 2014 and January 2015 and whose findings have been published elsewhere [7]. Bureti Sub-county is one of the 5 sub counties of Kericho county Kenya. It lies between latitude 0°25’ and 0°43’ South of the Equator and between longitudes 35°05’ and between 36°35’ to the East. It covers an area of 806 Km2, and it is divided into four administrative divisions with a population of 108 061 persons. Kipsigis ethnic group are the main occupants of the Sub-county and largely earn their living through small scale substance farming, trade, dairy farming and tea farming [8]. The Sub-county has 3 hospitals, 3 health centre and 24 dispensaries. According to the then Ministry of Health classification in the year 2014, the hospitals fell under level 4, health centers under level 3 while dispensaries were under level 1 of healthcare services delivery [9]. An analytic cross sectional study design was adopted for this study. All public health facilities in the subcounty were listed and stratified into the 3 levels of healthcare delivery. Thereafter, one health facility was randomly selected from each of the three levels i.e. level 2, level 3 and level 4. A sample size of 149 was recruited from all pregnant women coming for the second visit and above. Number of respondents participating from each facility was calculated to be proportionate to the monthly workload of pregnant women attending antenatal care clinic at the health facility. An exit interview was conducted on all pregnant women using a semi-structured questionnaire that had been pre-tested to collect information on demographic characteristics and knowledge of obstetric danger signs. Data was collected with the help of trained research assistants who were community health volunteers. Knowledge about obstetric danger signs of the respondents was assessed by asking questions regarding dangers signs during the pregnancy, childbirth and postpartum. Respondents were asked whether they knew of obstetric danger signs for each phase without any prompting. A participant was considered having knowledge of danger signs if she could spontaneously mention at least two danger signs at each phase.Raw data was entered into Ms Access program and analyzed using Statistical Package for Social Sciences (SPSS Version 16) software. Socio-demographic characteristics and knowledge of obstetric danger signs during pregnancy, at birth and postpartum were summarized by frequencies and percentages. Chi square test was used to determine association between socio-demographic factors and knowledge of obstetric danger signs. All tests were 2 sided and considered statistically significant at p<0.05.Ethical clearance for the study was obtained from the Ethical Review Committee of University of Eastern Africa, Baraton. Permission to conduct the study was sought from the Sub-county Medical officer of Health and all Officers In-charge of participating health facilities. Written informed consent was sought from all research participants after explaining the purpose, procedure, benefits and discomforts the study entailed. Participants were also informed of the right to refuse to participate in the study or to withdraw consent to participate at any time without reprisal. Confidentiality of research data was ensured; particularly, questionnaires did not bear any identification information for the individual participant. At the end of every data collection day, questionnaires were collected and locked in a secure place and data stored in a password protected computer. Access to study materials and raw data was restricted to the study team only.
3. Results
3.1. Demographic Characteristics of Respondents
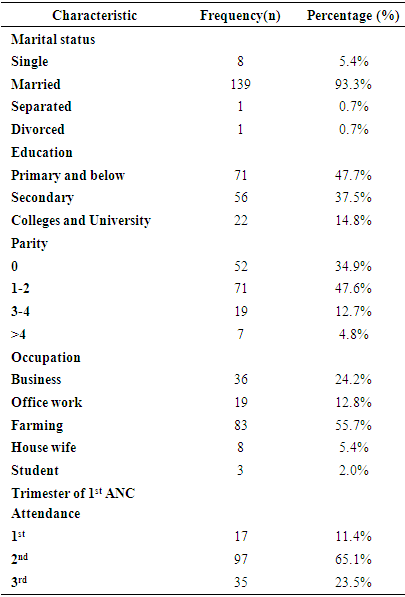
- The age range of respondents was 18 - 43 years, mean age being 24.5 years. Majority of the women, 93.3% (n=139) were married, those who had attained college secondary education and above were 52.3 (n=78). Farming was the most practiced economic activity at 55.7% (n=83). The highest parity was 10 while those who were pregnant for the first time were 34.9% (n=52). A greater proportion of the respondents, 65.1% (n=97) initiated their ANC attendance in the second trimester of pregnancy as shown in Table 1.
|
3.2. Knowledge of Obstetric Danger Signs
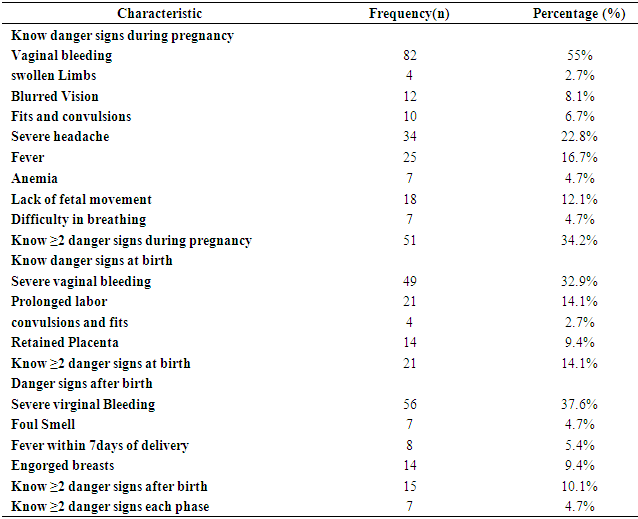
- Vaginal bleeding was the most common mentioned danger sign in pregnancy 55% (n=82), followed by severe headache 22.8% (n=34) and fever by 16.7% (n=25). The least mentioned danger sign in pregnancy was swollen limbs 2.7% (n=4). At birth, the most mentioned danger sign was severe vaginal bleeding 32.9% (n=49). Prolonged labor, which is one of the top five major causes of maternal deaths was mentioned by 14.1% (n=21) of respondents. The least mentioned danger sign was convulsions and fits, 2.7% (n=4). After delivery, severe vaginal bleeding was the most known danger sign, 37.6% (n=56) (Table 2).There was a declining trend in the proportion of women who were knowledgeable about obstetric danger signs in pregnancy, at birth, and after birth. Overall, 34.2% (n=51) of the respondents were able to mention at least two key danger signs during pregnancy, 14.1% (n=21) during child birth and 10.1% (n=15) during post partum. However, when the scores were combined, only 4.7% (n=7) of the respondents could mention at least 2 key danger signs in all the three phases (Table 2).
|
|
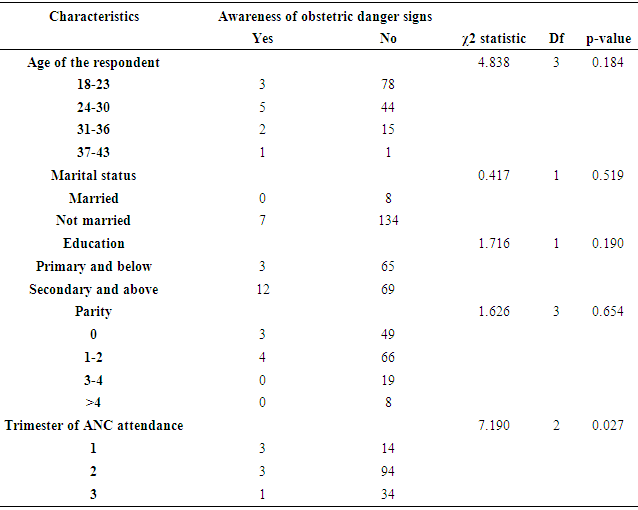
3.3. Factors Associated with Knowledge of Obstetrics Danger Signs
- A greater proportion of those who booked their first ANC visit within their first trimester were significantly more informed of obstetric danger signs compared to those who booked ANC in their second or third trimester (P-value 0.027). A greater proportion of women who had secondary school education and above were more knowledgeable of obstetric danger signs compared to their counterparts with primary school education and below, though, this was not statistically significant. Majority of married women were also more knowledgeable on obstetric danger signs compared to those not married, though this was also not statistically significant. Similarly, age and parity was not associated with knowledge of obstetric danger signs.
4. Discussion
- Women’s knowledge of potential obstetric danger signs is expected to influence their decision concerning what time they decide to seek medical care. Hence, knowledge of obstetric danger signs is likely to help women recognize these signs early when the complications occur and make a quicker decision to seek out health care which makes a difference between life and death. It is therefore important for women to be well-informed of all obstetric danger signs. The findings from this study revealed that only 4.7% of the study participants had knowledge of obstetric danger signs. This proportion was lower compared to earlier studies in Ethiopia which reported 15.5% [10], Egypt 25% [11] and Tanzania 25% [12]. This difference could be due to variation in socio demographic characteristics, geographical variations, health services coverage and use of different sampling technique for the selection of participants across the different studies. There was a general decrease in the number of pregnant women who were able to spontaneously mention at least two danger signs during each phase 34.8%, 14.1% 10.1%. i.e. pregnancy, birth and post partum respectively. These decrease is consistent with findings reported in studies from Raya Kabo district of Ethiopia [13] and rural Uganda [14]. It is highly probable that during pregnancy, a higher percentage of women perceive themselves to be in higher risk of developing pregnancy related complication. This perception in turn drives them to look for more information on potential complications, their management and prevention measures. After birth, the perceived risk most likely reduces, mothers no longer consider themselves at risk hence there is a reduced need to seek for information on post partum complications and their signs. On the other hand, the decrease could be an indication of missed opportunities for health talks. Health talks in ANC clinics are normally conducted early in the morning before normal health services delivery starts, mothers arriving late are likely to miss out on these sessions where among other topics, pregnancy related complications are discussed. The major causes of maternal direct mortality are hemorrhage whose danger sign is vaginal bleeding; sepsis whose indicator danger sign is fever; pregnancy induced hypertension whose danger signs are swollen limbs and face, severe headache and blurred vision; and prolonged labor whose indicator is labor for more than 12hours [15]. In the current study, the most common mentioned danger sign during across all phases in this study was vaginal bleeding. This is consistent with studies from Uganda [14], Tanzania [16] and Ethiopia [17]. This is encouraging as 33% of all maternal deaths are caused by hemorrhage [18]. This can partly be attributed to the perceived threat attached to bleeding in all the phases. In most African cultures, blood red denotes danger, thus it is easily remembered and associated with danger by mothers.The trimester in which a mother first booked for ANC was significantly associated with the knowledge of obstetric danger signs. A higher proportion of women who booked their first ANC clinic during the first trimester were significantly more knowledgeable of danger signs of obstetric complications compared to those who started in their second or third trimester. This finding is however contrary to a similar study conducted in Malaysia that reported no association [19]. Women who start antenatal care clinic during the first trimester have a relatively longer time and increased chances of interacting with healthcare workers and subsequently learning of obstetric danger signs compared to their counterparts who start their clinics in the second and third trimesters. Other socio-demographic characteristics like age, level of education, parity and marital status were not associated with the knowledge of obstetric danger signs, this finding is contrary to previous studies conducted in Malaysia, Tanzania, Ethiopia and Nigeria [10, 19-21]. The difference in results could partly be attributed to differences in methodological approaches adopted for this study. Nevertheless, age, level of education, parity and marital status play an important role in knowledge of obstetric danger signs marital status and parity were not significantly associated with the knowledge of obstetric danger signs. However, earlier studies found association between maternal education, parity and knowledge of obstetric danger signs. The study was a facility based study, in Kenya 94% of pregnancy women attend ANC clinics [4] thus missed only a few who missed ANC clinic. However, there were some limitations. First being a cross sectional study, it would not show a temporal association. Secondly, the study was lacked the qualitative aspect.
5. Conclusions
- Knowledge of women about obstetric danger signs was low in the area of study. Vaginal bleeding was the most mentioned obstetric danger sign during pregnancy, at birth and after delivery. There was a declining trend in the proportion of women who were knowledgeable about obstetric danger signs in pregnancy, at birth, and after birth. Trimester of initiating antenatal care clinic was significantly associated with knowledge of obstetric danger signs; however, age, level of education; parity and marital status were not associated. Sensitization campaigns to raise awareness on obstetric danger signs should be carried out in hospitals and at the community level so as to reach all women and their care givers irrespective of their social- demographic characteristics. The research employed only qualitative design thus there is need for future researches to focus on qualitative designs among women attending Antenatal care clinics to further unearth depth of knowledge on this subject in the community. The study did not assess the quality of counseling about obstetrics danger signs. Therefore further research should be conducted to assess whether the quality of counseling provided to pregnant women explains the level of knowledge about obstetric danger signs.
ACKNOWLEDGEMENTS
- We acknowledge all the study participants for giving their honest responses to make this study a reality.
Funding
- This study was financially supported by National Commission for Science, Technology and Innovation (NACOSTI) -Kenya. The funder had no role in study design, data collection and analysis, or preparation of the manuscript.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML