-
Paper Information
- Paper Submission
-
Journal Information
- About This Journal
- Editorial Board
- Current Issue
- Archive
- Author Guidelines
- Contact Us
Research in Obstetrics and Gynecology
p-ISSN: 2326-120X e-ISSN: 2326-1218
2017; 5(2): 30-34
doi:10.5923/j.rog.20170502.03

Outcome of Pregnancies on Top of Intrauterine Missed IUDs at a Tertiary Care Hospital in Egypt: A Three-Year Retrospective Study
Ayman Shehata Dawood, Mohamed Ahmed Elsharawy
Lecturer of Obstetrics and Gynecology, Tanta University, Egypt
Correspondence to: Ayman Shehata Dawood, Lecturer of Obstetrics and Gynecology, Tanta University, Egypt.
| Email: |  |
Copyright © 2017 Scientific & Academic Publishing. All Rights Reserved.
This work is licensed under the Creative Commons Attribution International License (CC BY).
http://creativecommons.org/licenses/by/4.0/

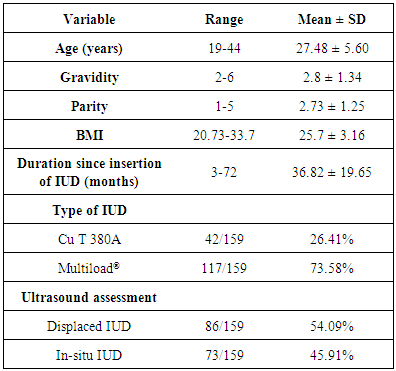
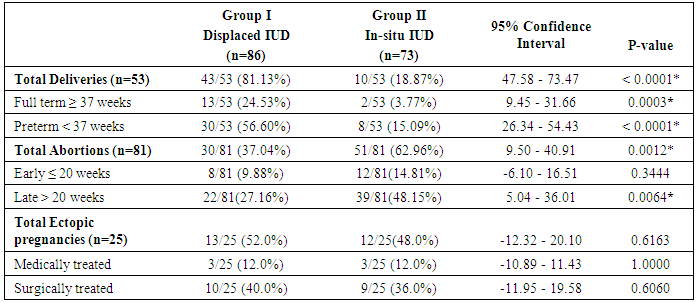
Objective: To determine the outcome of pregnancies occurring on top of missed intra-uterine devices (IUDs) and the relation to IUD site at a tertiary care hospital. Methods: All files of patients admitted at Tanta University Hospitals were reviewed in the period of in the period from January 1, 2013, to December 31, 2015. The relation between pregnancy outcomes and presence of missed IUD were evaluated. Results: The age of enrolled patients was ranged from 19to 44 years, the mean duration since IUD insertion was 36.82 ± 19.65 months. The most common type of IUDs detected in this study was the Multiload® being detected in 73.58% of patients. Most full-term deliveries 13/53 (24.53%) and preterm deliveries 30/53 (56.60%) occurred in the displaced IUD group. On the other hand, abortions were higher in the in-situ IUD group 51/81 (62.96%) versus 30/81 (37.04%) especially late abortions. No differences were found in the incidence of ectopic pregnancies in both groups. Conclusion: Poor pregnancy outcomes were increased with in-situ IUDs rather than displaced IUDs except for preterm labor as most patients in the in-situ IUDs abort early.
Keywords: Pregnancy Outcomes, Missed IUD, Displaced IUD, In-situ IUD
Cite this paper: Ayman Shehata Dawood, Mohamed Ahmed Elsharawy, Outcome of Pregnancies on Top of Intrauterine Missed IUDs at a Tertiary Care Hospital in Egypt: A Three-Year Retrospective Study, Research in Obstetrics and Gynecology, Vol. 5 No. 2, 2017, pp. 30-34. doi: 10.5923/j.rog.20170502.03.
Article Outline
1. Introduction
- Intrauterine devices (IUDs) are a common type of long-acting reversible contraceptives (LARC) which are widely known all over the world being non-hormonal, with a long duration, with high efficacy, cheap and with considerable safety. For these reasons, IUDs become the most popular method among most women desiring long period of contraception. [1, 2]Pregnancy on top of missed intrauterine devices is one of the reported complications of IUDs. This complication could occur whether the loop was displaced or still in-situ. Studies couldn't reach a conclusion whether pregnancy occurs first then the displacement of IUD or the reverse is true. [3, 4, 5]It is well known that pregnancies on top of IUDs have many complications rather than without IUDs. The reported complications were ectopic pregnancy, miscarriage, preterm labor, premature rupture of membranes and intrauterine infections. Most complications occur when the loop was kept in-situ and not removed early in pregnancy. [6] The NHS thus recommends IUD removal if threads are visible, or can be retrieved easily from the cervical canal. This can be commenced up to 12 weeks’ gestation. [7]In this study, we aimed to report complications of pregnancies occurring with this type of IUDs which were not removed early in pregnancy and correlate the site of IUD to pregnancy outcomes.
2. Materials and Methods
- Study design and settings: This retrospective study was conducted at Tanta University Hospital; a tertiary care hospital located at the centre of Nile Delta. It serves the population of four provinces and has a rate of 3500 deliveries per year. It serves the patients with very minimal fees, and sometimes free of charges. It is tertiary care hospital and referral hospital for many small hospitals in the four provinces for any complicated cases, or difficult case. This study was conducted on patients of Obstetrics and Gynecology Department in the period from January 1, 2013, to December 31, 2015.Patients: In this retrospective study, a thorough review of the patients who experienced accidental pregnancy with the Cupper IUDs and all data were extracted. The included patients were those who had non-removed IUD until delivery, abortion or other outcomes. The exclusion criteria were patients who had hormonal IUDs, patients who had the IUD removed early in pregnancy, and patients with incomplete medical records. Methods: All patients' demographic data, type of IUD, site of IUD in Ultrasound whether displaced or not, pregnancy outcomes and the relation to the presence of IUD was evaluated.Allocation: Patients were allocated into 2 groups; the group of displaced IUDs (group I) and the group of in-situ IUDs (group II).Ethical approval: This study was approved by the local institutional review board of Tanta University Hospitals under the code of 31052 in July 2016. As the study is retrospective, the patients' consent was not obtained.Statistical methods: The collected data were statistically analysed with IBM SPSS (version 18, USA) statistical software. The data are displayed as mean ± standard deviation (SD). The tests used were chi-squared test, Fisher’s test, Student’s t-test and Mann–Whitney U-test. P < 0.05 was considered statistically significant.
3. Results
- All files of patients admitted to Obstetrics and Gynecology Department, Tanta University, in the period from January 1, 2013, to December 31, 2015, were reviewed. A total of 14671 patients were admitted at that period. After exclusion of incomplete files (451 cases) either due to discharge prior delivery or escape of patients, the analysed files were 14220 cases. They were distributed as 5820, 4674 and 4726 cases in the years 2013, 2014 and 2015 respectively. As regard distribution of cases into pregnancy outcomes; 10254 cases represent all deliveries, 2461 cases represent abortions and miscarriage and 1500 cases represent all ectopic cases. These data are represented in figure 1.
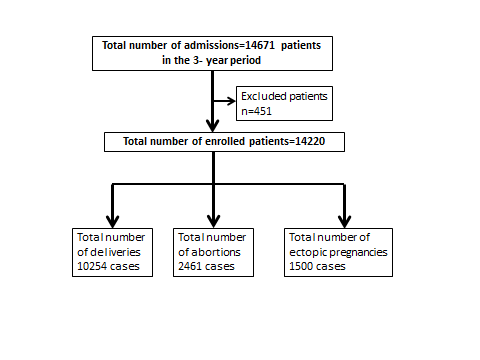 | Figure 1. Number of enrolled data and their distribution according to pregnancy outcomes |
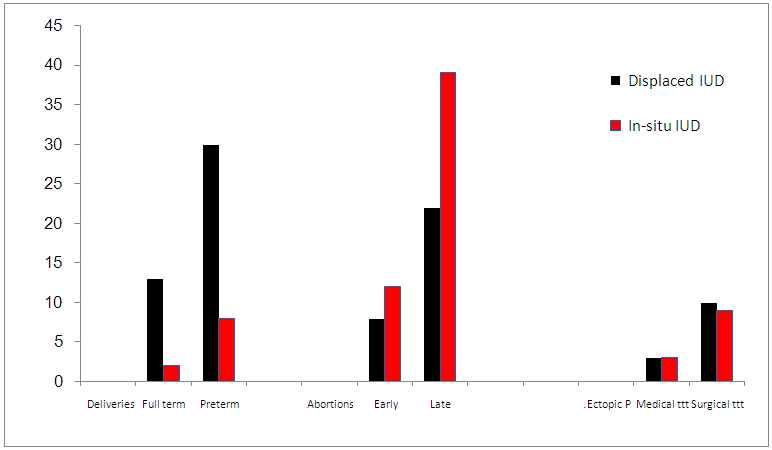 | Figure 2. Distribution of enrolled patients according to pregnancy outcomes (Ectopic P. = Ectopic pregnancies) |
|
|
4. Discussion
- Although pregnancies on top of IUDs are exceptional, women who become pregnant with an IUD are more prone to pregnancy complications than women without an IUD in-utero when conceiving. The risks of abortion, ectopic pregnancies, second-trimester miscarriage, preterm delivery and intrauterine infections are more accentuated if the IUD is left in-situ rather than removed at early diagnosis of conception. [8, 9]Generally, ectopic pregnancies occur at a rate of 2% of all pregnancies. But, if pregnancy occurred with IUD in-utero, the risk of ectopic pregnancy rises to 6%. Similarly, the miscarriage rate is approximately 13% for all pregnant women while that for women with IUDs is approximately 50-60%. The relative risk of preterm birth is increased 3- 4.5-folds if IUD is left in-situ. [10, 11]In the current study, the incidence of poor pregnancy outcomes was noticed in group II where IUD is in-situ rather than displaced IUDs. The incidence of full-term deliveries was 43/53 (81.13%) in group I compared to 10/53 (18.87%) in group II as most cases in this group either abort or deliver prematurely (P-value=0.0001). The incidence of preterm labor was 30/53 (56.60%) in group I compared to 8/53 (15.09%) in group II (P-value= 0.0001). This is explained by increased infections rates with IUDs which are important etiological factors in pathogenesis of preterm labor and premature rupture of membranes. In the current study, the total abortion reported were 30/81 (37.04%) in group I compared to 51/81 (62.96%) in group II (P-value=0.0012) due to increased adherence of IUD to gestational sac. Early abortions were similar in both groups (P-value=0.3444) while the late abortions > 20 weeks were 22/81(27.16%) in group I compared to 39/81(48.15%) in group II (P-value=0.0064). The rate of ectopic pregnancies either treated medically or surgically was nearly similar in both groups (P-value=0.6163).Inal et al, (2005) [12] conducted a prospective study to determine the factors affecting the occurrence of pregnancies with intrauterine devices. They compared 97 women with Cu375 Multiload® IUD inserted with 25 women with CuT380A IUD in place. They found that intra-cervical displacement of Multiload® IUD occurred among pregnant women, rather than those with correctly positioned IUDs. They found that 40% of pregnant cases resulted in abortion and the miscarriage rate was 77% when IUD left in the uterine cavity. The results of Inal and his colleagues are in agreement with the results of current study where Multiload® IUD was found to be associated with more complications than CuT380A IUD. [12]Similarly, Pakarinen et al (2005) [13] conducted a case-control study, in which 318 women with pregnancies on top of CuT380A IUDs in-situ were compared with 300 controls using CuT380A IUD. They found that the rate of malpositioning of IUD was 64% among pregnant cases, compared to 11% malpositioning rate among the non-pregnant controls (P<.05). [13]Braaten et al (2011) [14] conducted a retrospective case-control study where 182 women with malpositioned IUDs shown by ultrasonography were assessed at a single institution from 2003 to 2008 with 182 women with properly positioned IUDs. They found that more pregnancies occurred within 2 years among those in the malpositioned group than those in the control group (19.2% compared with 10.5%, P=.046). [14]Ekiz et al (2016) [15] conducted a retrospective study to assess the risk factors of pregnancy with CuT380A IUD and pregnancy outcomes. They found 4 ectopic pregnancies and 77 intrauterine pregnancies. The enrolled patients were allocated in into 2 groups group I (n=25/77) whose IUDs were removed, and group II (n=26/77) whose IUD Left in situ. They found that term pregnancy rates were 76% when IUD removed versus 20.8% when IUD left in-situ, p=0.002). Abortion rates were 16% when IUD removed versus 53.84% when IUD left in-situ, p=0.008). The results of Ekiz et al are in agreement with the current study results. [15]
5. Conclusions
- Intrauterine devices left in situ with pregnancy are linked to many adverse pregnancy outcomes. In this study, complications were more evident when IUD was in-situ rather than displaced IUDs. The incidence of preterm labor was found to be more in displaced IUD group as most patients of in-situ IUD group abort early. The recommendations of early removal of IUD when pregnancy occurs should be applied even if abortion occurred.
Abbreviations
- IUDs: Intrauterine devicesLARC: Long acting reversible contraceptives NHS: National Health Service
Key Message
- Most studies compared pregnancy outcomes in removed and non-removed IUDs while in this study comparison was done between displaced and in-situ IUDs. The important message is that in-situ IUDs had more adverse pregnancy outcomes than displaced ones and both should be removed whenever pregnancy diagnosed.
 Abstract
Abstract Reference
Reference Full-Text PDF
Full-Text PDF Full-text HTML
Full-text HTML